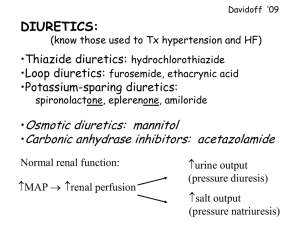
Introduction to Pharmacology James Karboski, PharmD Clinical Professor Overview of the Urinary System Functions of Urinary System • Maintenance of body fluids • Maintenance of electrolyte balance • Excretion – – – – Metabolic waste Excess electrolytes Excess water Drugs Anatomy Kidneys Bladder Ureters Urethra Afferent arteriole Efferent arteriole Major Processes • Glomerular Filtration Glomerular Filtration • Arterial pressure forces blood across glomerulus • Blood flow to kidneys 1200 ml/min (25% of CO) • Filtration sustained at mean BP>50 mmHg • Role of afferent/efferent arterioles Major Processes • Glomerular Filtration • Tubular Reabsorption • Tubular Secretion Movement of Electrolytes and H20 Peritubular Capillary Renal Tubule Na+ Cl- K+ Movement of Electrolytes and H20 • Proximal Tubule – 60-70% sodium/water reabsorbed • Descending Loop of Henle – Very low sodium permeability • Ascending Loop of Henle – High sodium permeability – 20-25% sodium reabsorbed Movement of Electrolytes and H20 • Distill Tubule – 5-10% sodium/water reabsorbed – Depends on aldosterone • Collecting Duct – Water reabsorbed if ADH present Actions of Kidney Actions of Kidney Peripheral Edema Peripheral Edema Pitting Edema Pulmonary Edema Pulmonary Edema Ascites Lymphedema Conditions Causing Fluid Overload • • • • • Heart Failure Liver Disease (Cirrhosis) Kidney Disease Hyperaldosteronism Corticosteroid Therapy Diuretics Diuretics • A drug that increases the rate of urine production • Used to reduce extracellular fluid volume • Most work by blocking the reabsorption of Na+ Remember: Water follows sodium! Na+ Cl- K+ Peritubular Capillary Renal Tubule F Categories of Diuretics • • • • • • Thiazide-Type Diuretics Loop Diuretics Potassium-Sparing Diuretics Aldosterone Antagonists Osmotic Diuretics Carbonic Anhydrase Inhibitors Thiazide-Type Diuretics Thiazide-Type Diuretics • • • • • Hydrochlorothiazide (Microzide®) Chlorothiazide (Diuril®) Chlorthalidone (Hygroton®) Metolazone (Zaroxolyn®) Indapamide (Lozol®) Thiazide-Type Diuretics • • • • • Hydrochlorothiazide (Microzide®) Chlorothiazide (Diuril®) Chlorthalidone (Hygroton®) Metolazone (Zaroxolyn®) Indapamide (Lozol®) Thiazide-Type Diuretics • Inhibits sodium reabsorption at the distill convoluted tubule • Oral dosage forms only • Moderate potency – Can only affect 10% of sodium load – Loses diuretic effect after 1-2 weeks of sustained use – Not effective in patient with significant renal disease • Primary use: – Hypertension – Short-term mild/moderate diuresis Loop Diuretics Loop Diuretics • Furosemide (Lasix®) • Bumetanide (Bumex®) • Torsemide (Demadex®) Loop Diuretics • Furosemide (Lasix®) • Bumetanide (Bumex®) • Torsemide (Demadex®) Loop Diuretics • Inhibit sodium reabsorption at the ascending Loop of Henle • Most effective diuretic class – Affect 20-25% of sodium reabsorption • Infinite dose-response – “High ceiling diuretics” • Retain their efficacy in patents with renal disease • Oral and IV dosage forms Loop Diuretics • Primary Use – Conditions resulting in moderate/severe edema • Heart failure, liver disease, renal disease – High blood pressure resulting from volume overload Loop and Thiazide ADRs • Dehydration – Too much diuresis – Dry mouth, increased thirst, low urine output • Hypovolemia – Too much or too rapid diuresis – Monitor blood pressure – Look for orthostatic changes • Dizziness, lightheadedness – Especially when going from sitting to standing Loop and Thiazide ADRs • Hypokalemia – Normal potassium 3.5-5 mEq/L – Potassium loss occurs in 40% of patients, but supplementation needed in 10% – Direct correlation to amount of diuresis – Consequences • Muscle weakness and cramps • Cardiac arrhythmias Loop and Thiazide ADRs • Glucose intolerance/Hyperglycemia – Worsen control in patients with diabetes • Calcium wasting – Affect bone metabolism • Ototoxicity – Loop diuretics only Potassium-Sparing Diuretics Potassium-Sparing Diuretics • Amiloride (Midamor®) • Triamterene (Dyrenium®) • Amiloride + Hydrochlorothiazide = Moduretic® • Triamterene + Hydrochlorothiazide = Dyazide® Potassium-Sparing Diuretics • Mechanism of Action – Block the sodium channels in the distal tubule – Prevents secretion of potassium • Different from thiazides and loop diuretics – Weak diuretics • Most of the sodium has already been reabsorped earlier in the tubule – Typically used in combination with thiazide diuretics • To maintain neutral potassium balance and enhance diuresis Potassium-Sparing Diuretics • Hyperkalemia – Normal potassium 3.5-5 mEq/L – Risk Groups • Renal Impairment • Diabetics • Elderly • Hidden potassium – Salt substitutes – Blood transfusions – Some low-sodium foods Potassium-Sparing Diuretics • Hyperkalemia – Complications • Muscular weakness • Paralysis • Cardiac arrhythmias Aldosterone Antagonists Aldosterone Antagonists • Spironolactone (Aldactone®) • Eplerenone (Inspra®) • Spironolactone + Hydrochlorothiazide = Aldactazide® Aldosterone Antagonists • Mechanism of Action – Aldosterone is a hormone that acts in the distal tubule and collecting duct to increase sodium reabsorption and prevent diuresis – Blocking the action of aldosterone • Decreases sodium reabsorption – Causing diuresis • Increases potassium retention – Labelled a potassium-sparing diuretic in some references Aldosterone Antagonists • Primary Use – Patients with increased levels of aldosterone • Heart failure • Liver failure • Cautions – Hyperkalemia • ADRs – Hormonal effects (spironolactone only) • Menstrual irregularities • Gynecomastia (men) • Hirsutism and breast tenderness (women) • Erectile dysfunction and decrease libido (men) Osmotic Diuretics Osmotic Diuretics • Glycerin • Mannitol • Urea Osmotic Diuretics • Mechanism of Action – Acts as “water magnet” – When in renal tubule • Trap water in tubule to cause diuresis – When in blood • Draw blood from tissues into blood – Cerebral edema – High intraocular pressure in glaucoma Carbonic Anhydrase Inhibitors Carbonic Anhydrase Inhibitors • Acetazolamide (Diamox®) Carbonic Anhydrase Inhibitors • Mechanism of Action – In tubule, carbonic anhydrase necessary for reabsorption of bicarbonate – Without bicarbonate, sodium ions not reabsorbed as efficiently – Results in increased urine volume and alkaline urine • Uses – Edema (rarely) – Glaucoma (reduces production of aqueous humor) – Some drug overdoses Nursing Considerations • For once daily dosing of furosemide, give the dose in the morning to prevent nocturia • Be aware of other risks for hypovolemia – Diarrhea – Vomiting – Significant sweating (we are in Texas after all) Nursing Considerations • Monitoring – Daily weights: report gains or losses of >2 lbs/day – The Big 4 Labs • Potassium • Sodium • Blood urea nitrogen (BUN) • Serum creatinine/Creatinine clearance – Blood pressure (especially postural changes) – Hydration status • I/O, weight, skin, pulse, mucus membranes Assessing Renal Function Creatinine Clearance 𝐶𝐿𝑐𝑟!"/!$% 140 − 𝐴𝑔𝑒 𝐵𝑊 = 𝑆𝑐𝑟 72 (x 0.85 for females) IBW(male) = 50 kg + (2.3 x inches over 5 ft tall) IBW(female) = 45 kg + (2.3 x inches over 5 ft tall) Grading Renal Function Creatinine Clearance Normal >80 ml/min Mild Impairment 50 - 80 ml/min Moderate Impairment 10 - 50 ml/min Severe Impairment <10 ml/min Example 1 Male 30 year old 6’0” 84 kg Scr = 1.2 Example 1 30 year old male, 84 kg (all muscle), 6’0”, Scr = 1.2 CLcr = ml/min [140 - Age] Wt [ Scr] [72 kg] Example 2 Female 72 year old 5’5“ 84 kg Scr = 1.2 Example 2 72 year old female, 84 kg (obese), 5’5”, Scr = 1.2 CLcr ml/min = [140 - Age] Wt [ Scr ] [72 kg] = Basics of Pharmacology James Karboski, PharmD Clinical Professor