Clinical uses
advertisement

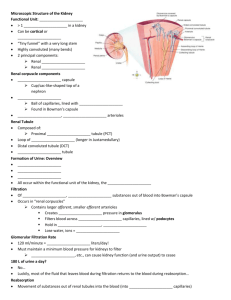
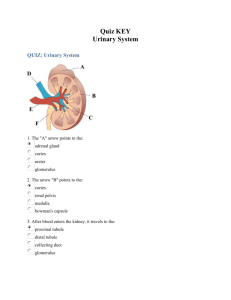
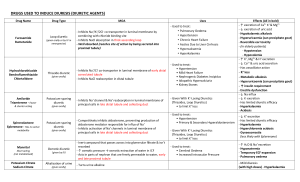
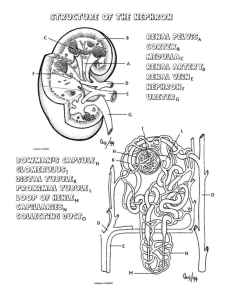
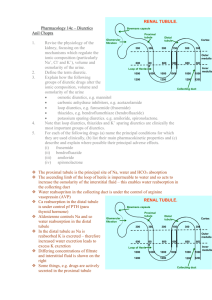
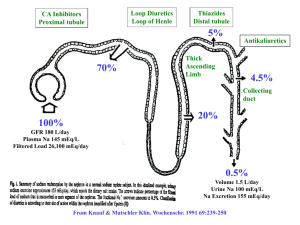
Diuretics and Dehydrants §1 Diuretics • Abnormalities in fluid volume and electrolyte composition are common and important clinical problems. Drugs that block the transport functions of the renal tubules are valuable clinical tools in the treatment of these disorders. It was not until 1957 that a practical and powerful diuretic agent (chlorothiazide) became available for widespread use. • Technically, the term "diuresis" signifies an increase in urine volume, while "natriuresis" denotes an increase in renal sodium excretion. Because natriuretic drugs almost always also increase water excretion, they are usually called diuretics. • Most diuretics act upon a single anatomic segment of the nephron. Because these segments have distinctive transport functions, the first section of this chapter is devoted to a review of those features of renal tubule physiology that are relevant to diuretic action. Renal Tubule Transport Mechanisms 1. Proximal tubule 2. thick ascending limb of Henle’s loop 3. Distal tubule and collecting ducts Proximal Tubule acetazolamide Loop of Henle loop diuretics Distal Convoluted Tubule thiazide Collecting Tubule Triamterene ※Common diuretics Common diuretics • exert effects on specific membrane transport proteins in renal tubular epithelial cells (loop diuretics, thiazides, amiloride, and triamterene) • exert osmotic effects that prevent water reabsorption (mannitol) • exert effects by inhibiting enzymes (acetazolamide) • exert effects by interfering with hormone receptors in renal epithelial cells (spironolactone) Ⅰ. High –ceiling diuretics (loop diuretics) Furosemide, Ethacrynic acid, Bumetanide [Pharmacological actions] Site of action: thick ascending limb of Henle’s loop Mechanism: competing with Cl- for Cl- joint-part of Na+ -K+ -2Cl- cotransporter Effects 1. Diuresis: Na+, K+, 2Cl-, Mg2+, Ca2+ excretion↑ 2.↑renal blood flow: ↓renal vescular resistance pharmacokinetics • 1. p.o. & intravenous administration • 2. excretion: by organic acid secretion route in the proximal tubule uric acid (尿酸) ↑ gout indomethacin( 吲哚美辛) probenecid (丙磺舒) Clinical uses • 1. Acute and Severe edema • Acute pulmonary edema cerebral edema Clinical uses • 3. acute renal failure: early stage • 4. Hypercalcemia : • 5. Overdose of some toxicants: bromide , fluoride , iodide Adverse reactions 1. Electrolyte disorders: • hypochloremia, hypomagnesemia, hypokalemia※ CHF: ↑intoxication with digitalis Hepatic cirrhosis: coma 2. Ototoxicity: dose-related hearing impairment: tinnitus, hearing loss, etc. Adverse reactions 3. hyperuricemia • (1) hypovolemia: reabsorption of uric acid • (2) competing with diuretic for organic acid secretion route →secretion of uric acid↓ 4. Others: GI reactions, allergic reactions Ⅱ.Moderate efficacy diuretics • Thiazides: ※Hydrochlorothiazide (氢氯噻嗪), chlorothiazide (氯噻嗪) • Indapamide (吲哒帕胺) • chlortalidone(氯酞酮) Pharmacological actions Site of action: proximal end of distal tubule Mechanism: inhibit Na+ -Cl- cotransporter Effects 1) Diuresis: Na+ , K+ , 2Cl - , Mg2+excretion↑ 2) ↑Ca2+ reabsorption in distal tubules: primary hypercalciuria 3) reduced peripheral vascular resistance Clinical uses 1. Chronic edema mild to moderate cardiac edema: first choice ascites(腹水)due to cirrhosis(肝硬 变) 2. hypertension early stage: ↓ blood flow late stage : excretion of Na+↑→ Na+-Ca2+ exchange↓ → ↓Ca2+ in cell → tension of arterial↓ 3. nephrogenic insipidus 1) ↓ PDE → intracellular cAMP↑→ water permeating the tubule↑ → reabsorption of water↑ • 2) excretion of NaCl↑ → plasma osmotic pressure↓ → thirst feeling↓ → amount of drinking↓ → urine↓ 4. Primary hypercalciuria Adverse reactions • • • • 1. electrolyte disorders 2. retention of uric acid and calcium 3. hyperglycemia and hyperlipidemia 4. allergic reaction: Ⅲ. Potassium-sparing diuretics • Site of action: distal tubule and collecting duct aldosterone antagonist: Spironolactone (antisterone) 【 mechanism 】 : competing with ald. for ald-R in distal tubule and collecting duct → Na+-K+ exchange↓ 【 characteristics 】 ※ ineffective in adrenalectomized animal ※ slow onset & long duration Clinical uses • 1. primary hyperaldosteronism • 2. liver cirrhosis and nephritis syndrome (1)inactivation of ald.↓ (2)circulation blood volume↓ Adverse reaction • 1. hyperkalemia: renal insufficiency • 2. endocrine abnormality: impotence, gynecomastia, nonaldosterone antagonists ※ triameterene(氨苯蝶啶) ※ amiloride (阿米洛利) • Mechanism : Block Na+ –channel → ↓ Na+ entry →K+ secretion↓ • clinical uses : • adverse reaction : §2 dehydrants • • • • Difficultly penetrate membrane filtrated by glomerulus easily Not be reabsorpted by renal tubules Not be metabolized mannitol(甘露醇) • Pharmacological actions • 1. dehydrant effect • 2. diuretic effect Cliniucal uses • 1. Brain edema • 2. Glaucoma • 3. Prevent acute renal failure Adverse reaction • extracellular volume expansion • contraindication: chronic heart failure