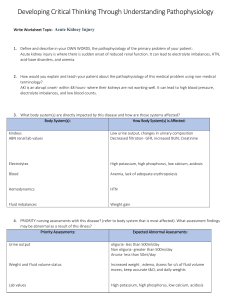
Acute Kidney Injury (AKI) Case Study Fluid and Electrolyte Concept NUR 443 Spring 2020 A.S. is a 70-year-old Caucasian woman who presented to the emergency department because of a 4-day history of increased shortness of breath and generalized weakness. A.S. stated that she has been able to do her daily chores at home independently, but for the last few days it was getting difficult for her to get around and that she needed to take frequent breaks because she was short of breath and had no energy. She has a long history of heart failure, diabetes mellitus type 2, and hypertension. She is admitted with a tentative diagnosis of acute kidney injury (AKI). Subjective Data • Has been having headaches on and off, with nausea and dizziness • Reported that she hadn’t been taking her medications regularly at home because of “forgetfulness” • Has not been urinating a lot • Feels “puffy” in her legs and hands Objective Data • Physical Examination • Blood pressure 178/96, pulse 110, temperature 98.9° F, respirations 24 • Alert and oriented to person, place, and time • Mild jugular venous distention • Fine crackles in bilateral lower lobes • Heart rate regular, no murmurs • Bowel sounds normoactive and present in all four quadrants • 2+ edema bilateral lower extremities and hands • ↑Echocardiogram shows decreased left ventricular function • Urinalysis: Urine dark yellow and cloudy, negative for glucose and ketones, • 24-hour urine output = 300 mL • Laboratory Tests: ✓ ✓ ✓ ✓ ✓ ✓ ✓ ✓ ✓ Hemoglobin Hematocrit RBC WBC Sodium Potassium BUN Creatinine 8 g/dL ↓ 18% ↓ 2.57 million/mm3 ↓ 4.7 mm3 WNL ↓ 132 mEq/L ↓ 5.9 mEq/L ↑ 36 mg/dL ↑ 4.9 mg/dL ↑ Case Study Questions: Please fill out answers and submit work to 443 Blueline 1. Interpret all of A.S.’s laboratory test results and describe their significance. Damaged kidneys do not make enough EPO= ↓RBC production which then ↓in O2 being delivered to the body. ↓Na d/t decreased glomerular filtration and the loss of free water. ↑K+ from leakage from intracellular space, break down of muscle/tissue can lead to cardiac dysrhythmias. ↑BUN/CR d/t lack of perfusion to kidneys 2. What is the most likely cause of A.S.’s AKI and explain why? Heart failure. Decrease in blood flow lead to decrease in glomerular perfusion and filtration of the kidneys. 3. Is this cause of AKI classified as prerenal, intrarenal, or postrenal? Prerenal (disorder that causes decreased systemic circulation) 4. What phase of AKI is A.S. in? (Oliguric, Diuretic, Recovery) Explain how you know this. Oliguric phase Based on lab results. UO <400ml/day as evidenced by 24-hour urine = 300ml; serum electrolyte imbalance: ↓Na, ↑K+, ↑BUN/Cr Neurologic disorder r/t weakness 5. What are the priority nursing diagnoses to address the concern of fluid retention? Risk for dysrhythmia r/t electrolyte imbalance Excess fluid volume r/t acute kidney injury 6. What are the priority nursing interventions for these nursing diagnoses? Restrict fluid Administer diuretics Monitor electrolytes Monitor VS Assess lungs for crackles Monitor I&O’s Daily weights Hemodialysis