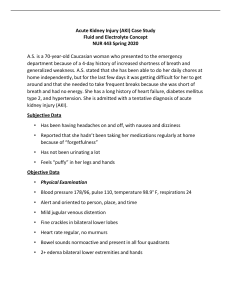
Question 1. Amlodipine is a calcium channel blocker. Why would the patient have been prescribed this? The patient has had a history of HTN for ten years The calcium channel blocker amlodipine is used to lower blood pressure by slowing the movement of calcium into the cells of the heart and blood vessel walls, which makes it easier for the heart to pump. Question 2. HCTZ is a diuretic. Why would the patient have been prescribed this? Hydrochlorothiazide can be used alongside other medications to treat high blood pressure. Hydrochlorothiazide is also used to treat fluid retention (edema) that is caused by congestive heart failure. Question 3. Is this patient technically underweight, overweight, obese, or is this patient’s weight considered healthy? MI is used to broadly define different weight groups in adults. Underweight: BMI is less than 18.5, Normal weight: BMI is 18.5 to 24.9, Overweight: BMI is 25 to 29.9, Obese: BMI is 30 or more. According to his height and weight calculations, the patient BMI is at about 17.2 which is underweight in this category for adults. Question 4. Identify all of this patient’s risk factors for chronic obstructive pulmonary disease and note which of them is the single most significant risk factor. The risk factors for chronic pulmonary disease are advanced age the patient is 57 years old. The patient is a heavy second-hand smoker, which is the primary risk factor for the development of COPD. The patient’s exposure to environmental factors such as asbestos exposure, and occupational exposure plays a part in the risk factors. Question 5. Identify all of the clinical manifestations in this patient that are consistent with chronic bronchitis. The patient has a cough in the morning and usually coughs up a scant amount of clear sputum. Patient Case Question 6. Identify all of the clinical manifestations in this patient that are consistent with emphysema. The patient would have coughing or wheezing, a cough that produces mucus, shortness of breathing and wheezing. Patient Case Question 7. Identify all of the clinical manifestations in this patient that are consistent with pulmonary hypertension and cor-pulmonale. High blood pressure in the arteries of the lungs is known as pulmonary hypertension it is a common cause of cor- pulonale. The manifestations found in the patient Swelling (edema), Shortness of breath, hypertension, fatigue chest, cyanosis, and tachycardia. Patient Case Question 8. To which stage of development has this patient’s COPD progressed? The patient has progress to the level 3 stage out of four which makes him a severe case of COPD. He is showing signs of chronic bronchitis and emphysema. His FEV1 is between 30% and 49%. His FEVI level is 45% according to the patient chart. Patient Case Question 9. Which serious condition is indicated by the patient’s arterial blood gas analysis? Due to the Ph being at 7.32 the patient has acidosis combined with a low amount of o2 and high co2 the patient has respiratory acidosis. This will need to be treated because of the respiratory acidosis the patient has hypoxemia. Patient Case Question 10. The patient has a strong history of alcohol abuse, which can cause liver dysfunction. Are there any indications that liver function has been compromised? All the levels of alanine transaminase (ALT) and aspartate transaminase (AST) are within the normal ranges on the patient chart. The only things that stood out to me that could play a part in liver dysfunction were the patient was hepatosplenomegaly, fluid wave, and distension but I am not sure about this. Patient Case Question 11. Explain the apparent disparity in this patient’s two major renal function tests (i.e., BUN and Cr). The Bun level for the patient is 29mg/dl which is a high level for the BUN the normal levels are 7-20 mg/dl. The level for Cr is 1.1 for the patient, the normal levels are 0.74 to 1.35 mg/dl for men. The high level of BUN could indicate kidneys art working well, could be dehydration, or a urinary tract obstruction. Patient Case Question 12. How can this patient be displaying signs of both dehydration, and fluid retention in the lower limbs coupled with ascites? Ascites is a condition where fluid buildup collects within the abdomen. The patient also has poor skin turgor, and clubbing in the extremities which is both fluid retention in the lower extremities and skin turgor dehydration. Think this is partly due to hypertension and inadequate blood flood. Patient Case Question 13. Would this patient benefit from home oxygen therapy? Yes, this patient would benefit from O2 therapy. The patient is using his accessory muscles at rest, and has poor breath sounds, and crackles. That and his sao2 is at 90% which is low. Patient Case Question 14. Is there any reason to believe that an infection caused this patient’s relapse of chronic obstructive pulmonary disease? Nothing that I could find would cause a relapse of the patient’s COPD. All the report said it said was that he cut back his smoking but did not cease it completely. And smoking is the primary risk factor for the development of COPD. Patient Case Question 15. Is the patient in this case study alpha-1-antitrypsin deficient? Normal range for AAt is 80-120 and the patient level is at 137mg/dl so no he is not alpha-1-antitrysin deficient. Question 1. What is the pathophysiologic mechanism for adrenal insufficiency in this patient? Primary adrenal insufficiency is shown by decreased aldosterone and cortisol production due to diminished gland function. The patient is taking prednisone to treat the symptoms of low corticosteroid levels this is because the body is not producing any or not enough to support the normal corticosteroid levels. Question 2. What is a potential cause of the abnormal DEXA scan in this patient? Since the patient is on corticosteroid medication, this medication can inhibit calcium absorption and vitamin D intake. Vitamin D helps with the absorption of calcium to build strong bones in the body. If the patient loses this absorption intake of vitamin D and calcium it can lead to problems like weak bones and osteoporosis. Question 3. Why is this patient taking cyanocobalamin IM? Cyanocobalamin is used to treat and prevent the B12 deficiency. The body requires vitamin B12 to make new red blood cells. Since the patient has Crohn’s disease which is inflammation in the intestines this can hinder the proper absorption of food and other substances needed for new blood cells. Question 4. Based on your analysis of this patient’s medication profile alone, what can you deduce about the degree of severity (mild to moderate or severe) of Crohn’s disease in this patient? The patient I would say is severe in the severity of Crohn’s disease. On the surface, it looks like the patient can lead a normal life but with the problems of taking Trazodone an antidepressant, Prednisone, and cyanocobalamin, and is also suffering from abdominal pain, diarrhea, low hormone levels, and vitamin deficiencies. Question 5. What is likely the cause of this patient’s cushingoid facial appearance? Because of the use of steroids and taking medication for her cortisol levels. The medication can cause some inflammation which can get to the face. Question 6. Briefly describe a cushingoid facial appearance. Moon face as it is called is a symptom of Crohn’s disease is round because of the fat deposits around the face. Question 7. What is the most likely cause of the abnormal vital sign of most concern above? The elevated blood pressure is of concern because the patient has diarrhea and vomiting, dehydration, and electrolyte imbalances which lead to fluid loss and the heart is trying to compensate for the loss of fluid. Question 8. What do the examination findings in the skin suggest? With all the fluid that is being lost by the patient these signs of warm and dry with flakiness and poor skin turgor are signs of the patient being dehydrated. Question 9. What does the phrase “sclera without icterus” suggest? That the patient does not have jaundice or yellowing of the sclera. The sclera is the white part of the eye. The lack of the patient having jaundice would lead to that the Cohn’s disease has not caused inflation of the liver at this stage. Question 10. Identify the two abnormal HEENT findings above and provide a pathophysiologic explanation for each of them. 1 Dry mucous membranes is due to dehydration and the is losing fluids as stated before with the loss of diarrhea, electrolytes, and vomiting. 2 Arteriolar narrowing is an early sign of ocular damage including retinopathy, optic neuropathy, and choroidopathy. If the High blood pressure persists it can cause changes in the arterial walls. Question 11. What is a likely cause of “truncal obesity with striae”? The adipose tissue accumulates in the trunk area this is where the high levels of cortisol in the blood are excessive. Question 12. What are striae? Striae are stretch marks that appear on the patient if there is rapid weight loss or gain. These marks are usually red and can cause scars on the skin tissue. Question 13. What is meant by guarding? It is an involuntary reaction to protect an area of pain, as by spasm of muscle on palpation of the abdomen over a painful lesion. Question 14. Identify the four abnormally elevated laboratory findings above and provide a brief and reasonable pathophysiologic explanation for each of them. Glucose fasting is at 120 and should be at 99 or lower the inflammation of Crohn’s can cause the cells to become insulin resistant. White blood cells are at 11,700 which is elevated due to the inflammation and infection that Crohn’s disease cause. Magnesium level is at 2.6mg/dl and the normal range is 1.7-2.2mg/dl, the high magnesium level is an indication the kidneys are not working correctly, and excess magnesium is not leveling the body. Alanine aminotransferase 54 iu/L is possible there is some liver damage from the infection. Question 15. Identify the four abnormally low laboratory findings above and provide a brief and reasonable pathophysiologic explanation for each of them. Total protein 3.9 g/dl should be 6.0-8.3 g/dl the protein is important for the health and growth of the body cells and tissues. Potassium levels should be at 3.6-5.2 mEq/L the patient is 3.0 mEq/L which is low this can cause dehydration by vomiting frequent urination and diarrhea. This can also cause abnormal heart rhythms and muscle cramps. Albumin should be between 3.4-5.4 g/dl the patient is at 2.4 g/dl this protein made by the liver helps keep fluid from leaking out of your bloodstream and into other tissues. Adrenocorticotropic hormone is to stimulate the adrenal glands to release cortisol. The range is 10-60 pg/ml the patient has a level of 2 pg/ml this low level can cause a reduction in the secretion of adrenal hormones resulting in adrenal insufficiency. Question 1. With two words, identify the specific type of hypovolemic shock in this patient. Hemorrhagic shock. Question 2. Based on the patient’s clinical manifestations, approximately how much of her total blood volume has been lost? The patient is in class three shock which is about 30-40% of blood loss and in decreased blood loss. The capillary refill time is at 7-8 seconds is a long time for a capillary refill and on average should be at about 1-2 seconds for a normal adult. She has absented peripheral pulses, and a thready brachial pulse and a doppler ultrasound were needed for an accurate BP reading. Question 3. Is it necessary that sodium bicarbonate be administered to the patient at this time? Yes sodium bicarbonate works to correct metabolic acidosis. Sodium bicarbonate works by mixing with lactic acid which forms in low perfusion states and in periods of inadequate oxygenation. The patient is in acidosis by her low ph, and high CO2 levels. It also helps raise blood pressure because it can have an effect that influences the movement of fluids in the body cells. Question 4. Are arterial blood gas results improving or deteriorating? -pH- 7.31 – 7.36 (NORMAL RANGE 7.38-7.42 pH), -SaO 2- 84% - 95% (NORMAL RANGE - >95%), PaO 2 – 53 mm Hg – 82 mm Hg (NORMALRANGE 75-100 mmHg), -PaCO 2 - 52 mm Hg – 38 mm Hg (NORMAL RANGE 38-42 mm Hg) After taking the sodium bicarbonate and oxygen the patients levels were heading toward becoming homeostasis. Question 5. Based on urine output rate, in which class of hypovolemic shock can the patient be categorized at this time? With the patient having a urine output of 14mL over an hour span that would put her still in the level three shock category. The normal level for urine output is 30mL an hour, But the 1 L of lactated ringer`s and the packed red blood cells that she received have helped improve her condition and possibly drop her to a level two shock category. Question 6. Explain the pathophysiology of the abnormal BUN and Cr. The Bun of the patient is at 37 mg/dl the normal levels are between 6-24 mg/dl. The high BUN levels are an indication that the kidneys aren’t working well. This can be due to not having enough fluids or other reasons. This high BUN level needs to be addressed because the kidneys could get worst. Women’s creatinine levels are between 0.61.1 mg/dl. The patient level is 1.9mg/dl which is at a higher-than-normal level. Creatine is a waste product from a muscular function that is normally filtered by the kidneys, but because of the high level of creatine, it is not getting filtered in the kidneys it shows up as having kidney dysfunction. Question 7. Does the patient have a blood clotting problem? No, the patient does not have a clotting problem. The PT (Prothrombin time) is a test to evaluate blood clotting. The PT for the patient is 12.1 sec the normal ranges is 11-to13.5 so she is well within that range. The PTT (partial thromboplastin time) is a test to measure how long it takes for clot to form in a blood sample. The PTT level in the patient is 33 sec the normal range is 25-35 sec again well within range. Question 8. Explain the pathophysiology of the abnormal serum glucose concentration. The normal blood glucose level is 140 mg/dl the patient is at 157 mg/dl. The rise in blood sugar indicates the degree of severity of the injury earlier than the fall in blood pressure does. The rise in blood sugar is attributable to a reflex increase in glycogenolysis due to catecholamine secretion stimulated via baroreceptors in shock. Question 9. Based on clinical signs after surgery, in which class of hypovolemic shock can the patient be categorized at this time? With all the patient lab values and vital signs improving much better, I would say the patient is now at a level consistent with stage 1 hypovolemic shock PaO 2 – 53 mm Hg – 82 mm Hg (NORMALRANGE 75-100 mmHg) -PaCO 2 - 52 mm Hg – 38 mm Hg (NORMAL RANGE 38-42 mm Hg) Hi savannah, I like what you did on question two about giving all the stats on why the patient has volume blood loss. I also found it beneficial that you recognize that it was an emergency but not only that you were talking about what the next steps were before there were even asked. Because of blood loss, you talked about giving a bolus of fluid and also giving sodium bicarbonate. Hello Jannah, I thought that on question five you did an excellent job explaining the urine output rate. Showing the steps and pathway were well done and very simple to follow. Question eight was also well explained on the pathophysiology of the serum glucose concentration the only thing I would add is how it relates to the patient’s problem.