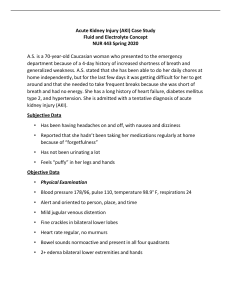
ACUTE KIDNEY INJURY IN ICU DR. SATISH PATEL SENIOR RESIDENT D.M. (CRITICAL CARE MEDICINE) DEPT. OF ANAESTHESIOLOGY AND CRITICAL CARE INTRODUCTION Acute kidney injury (AKI) is sudden deterioration of previously normal or stable kidney function, usually occurring over hours or days. Oliguria is considered the oldest recognised sign of renal failure as described by the English physician William Heberden nearly 200 years ago. Creatinine as a marker of renal function was detected by Max von Pettenkofer in 1844. However, the systematic inclusion in the definition of AKI did not occur until the description of the Risk, Injury, Failure, Loss, End-stage (RIFLE) criteria in 2004, where a urinary output of less than 0.5 ml/kg/hr for more than 6 hours was introduced as an alternative criterion to a rise in serum creatinine by 1.5-fold from baseline. DEFINITIONS AKI Acute Kidney Disease (AKD) – If AKI persists at day 7, it is termed as AKD Chronic Kidney Disease (CKD) - If AKD is present on day 90, it becomes CKD Recovery of AKI - Absence of creatinine and urine output criteria within 7 days after AKI onset. Rapid Reversal - If recovery occurs within 48 hours of onset INCIDENCE In the ICU the incidence of AKI varies between one-third to two-thirds of ICU patients when defined by the RIFLE, AKIN, or KDIGO criteria Of all ICU patients with AKI 10-15% require renal replacement therapy (RRT) Approximately one in five patients developed AKI after major surgery. The mortality in patients with AKI requiring RRT more than 50%. RISK FACTORS Multifactorial Recognizing these risk factors may help to prevent AKI or stop the development of AKI progressing. NON-MODIFIABLE RISK FACTORS MODIFIABLE RISK FACTORS Beginning and Ending Supportive Therapy for the Kidney AKI – SHORT AND LONG TERM EFFECTS In the long-term, AKI is associated with higher mortality and morbidity. DIAGNOSIS OF AKI Currently, diagnosis of AKI and staging into three stages is based on the Kidney Disease Improving Global Outcomes (KDIGO) classification established in 2012. AKI is diagnosed if serum creatinine increases by 0.3mg/dl or more in 48 hours or rises to at least 1.5-fold from baseline within 7 days or urine volume <0.5 ml/kg/h for 6 hours. The importance of both criteria (serum creatinine and urine output) was confirmed in a recent study of >32,000 critically ill patients showing that short- and long-term risk of death or RRT were greatest when patients met both criteria for AKI and when these abnormalities persisted for longer than 3 days. RIFLE and AKIN CRITERIA KDIGO CRITERIA The AKIN criteria emerged from the joint work of nephrologists and intensivists to make the RIFLE criteria more sensitive and reliable. Several pieces of evidence suggested that even small changes in serum creatinine may be associated with increased mortality. The AKIN criteria classified the minor changes in serum creatinine i.e more than 0.3 mg/dl increase in values over a period of 48 h to determine the AKI. Later in 2012, the AKI study group, “KDIGO” further modified the AKI definition by considering changes in creatinine within 48 h or a decline in the GFR more than 50% over 7 days LIMITATIONS OF SERUM CREATININE AS AKI CRITERIA LIMITATIONS OF URINARY OUTPUT AS AKI CRITERIA FUROSEMIDE STRESS TEST Performed in euvolemic patients by administering 1.0 mg/kg of furosemide intravenously as a bolus dose (or 1.5 mg/kg in patients who were treated with furosemide within last 7 days). If, in patients with AKI stage 1 and 2, the urine output response is less than 200 mL over the following 2 hours both the risk for progression to stage 3 AKI and need for RRT is high. This test reflects the renal tubular function integrity In the validation study, the furosemide stress test outperformed urinary biomarkers in predicting the development of stage 3 AKI, the need for RRT, and inpatient mortality. AKI BIOMARKERS The release of these biomarkers in blood and urine is dynamic and temporary, making the timing of the measurement important. So their accuracy for early detection of AKI, before creatinine increases, is best in situations where the clinical insult is clearly defined (eg. cardiac surgery, administration of nephrotoxin). Increased biomarker levels without increase in creatinine level (subclinical injury) Increase of creatinine without increased biomarker level points to a functional AKI/prerenal Greatest limitation is availability and cost. AKI BIOMARKERS 1. AKI STRESS MARKER TIMP-2 x IGFBP-7 FDA-approved and marked for clinical use ≥21 years; to predict the risk of developing stage 2–3 AKI within 12 h of assessment 2. AKI DAMAGE MARKERS C-C CHEMOKINE LIGAND (CCL4) KIDNEY INJURY MOLECULE (KIM-1) KIM-1 levels increase 12–24 h after tubular injury, peaking at 2–3 days NEUTROPHILE GELATINASE ASSOCIATED LIPOCALCIN (NGAL) Levels peak 4–6 h after tubular injury; elevated in sepsis and inflammation and thus, its use is limited in the ICU setting L-TYPE FATTY ACID-BINDING PROTEIN (L-FABP) Dipstick Albuminuria : initial screening tool for the evaluation of kidney disease because of its low cost and rapidity 3. AKI FUNCTIONAL MARKERS CYSTATIN C Cystatin is produced by all nucleated cells at a constant rate and released in the plasma. It has a low MW facilitating glomerular filtration. In the tubule cystatin C is reabsorbed and almost completely catabolized in the proximal tubular cells. The reciprocal of its serum level thus becomes a good marker of glomerular filtration Cystatin-based formulas for the calculation of eGFR are more accurate than creatinine based equations in critically ill patients SERUM CREATININE FUROSEMIDE STRESS TEST,2 H U.O DIAGNOSTIC WORKUP AKI can have multiple, sometimes co-existing aetiologies in critically ill patients Most common causes are sepsis, surgical trauma, heart failure, haemodynamic instability, hypovolaemia and exposure to nephrotoxic substances or contrast. Obstructive nephropathy Acute parenchymal and glomerular renal diseases The specific diagnostic workup in individual patients with AKI depends on the clinical context, severity and duration of AKI but also local availability Clinical examination URINE DIPSTICK Urine dipstick testing is simple and easy to undertake and recommended for all AKI cases The detection of blood, protein, leucocytes, nitrites and/or glucose in urine in a patient with AKI may indicate a potentially treatable glomerular or tubular pathology, including • glomerulonephritis (with haematuria and proteinuria) • acute pyelonephritis (with pyuria/ leucocyturia and nitrites in urine) • interstitial nephritis (occasionally with eosinophiluria) • Interpret the results alongside the clinical history and presentation of the patient URINE ANALYSIS • PRERENAL: bland urinalysis and (transparent) hyaline casts • INTRINSIC/RENAL AKI : Fatty casts - lipids in urine. This is most often a complication of nephrotic syndrome. Granular casts - ATN secondary to ischemia or nephrotoxic injuries Red blood cell casts - in glomerulonephritis mean there is a microscopic amount of bleeding from the kidney. Renal tubular epithelial cell casts reflect damage to tubule cells in the kidney. These casts are seen in conditions such as renal tubular necrosis, viral disease such as cytomegalovirus (CMV) nephritis, and kidney transplant rejection. Waxy casts - can be found in people with advanced kidney disease and long-term (chronic) kidney failure. White blood cell (WBC) casts - are common with acute kidney infections and interstitial nephritis. Finally, urine microscopy can be informative in rare cases of AKI, for instance, ethylene glycol poisoning where oxalate crystals may be seen or in tumour lysis syndrome where urate crystals may be present. • POSTRENAL: bland urinalysis. RBCs with nephrolithiasis URINE ELECTROLYTES Presence of low fractional sodium, uric acid and urea excretion together with a normal urinary sediment may support the diagnosis of functional AKI (Prerenal), the absence of these typical urinary electrolyte abnormalities do not exclude it. Low FENa values have also been observed in experimental sepsis with increased renal blood flow as well as in the first hours of sepsis in humans. In patients on concomitant diuretic therapy FEUrea can be used DYSMORPHIC RBC RENAL IMAGING Renal USG is the first-line imaging modality in most cases of AKI Reduced corticomedullary differentiation and decreased kidney size is indicative of underlying chronic kidney disease (CKD) while enlarged kidneys may be seen in infiltrative disease or renal vein thrombosis. Also diagnose obstruction of the urinary collecting system/ structural renal disease Renal Doppler ultrasound and contrast-enhanced ultrasound - to estimate renal perfusion and renal cortical microcirculation, respectively. Computer tomography (CT) is commonly used in the ICU : 1. Source of sepsis (pyelonephritis) 2. Diagnostic workup of AKI (abdominal aortic aneurysm, aortic dissection or retroperitoneal haemorrhage, pyelonephritis) AUTOIMMUNE PROFILE Mandatory in patients with AKI presenting primarily with a haemolysis / thrombocytopenia, pulmonary-renal syndrome or haemoptysis but also in patients with clinical symptoms suggestive of an autoimmune disorder to r/o immune mediated vasculitis and CTD. Anti-neutrophil cytoplasmic antibody (ANCA), anti-nuclear antibody (ANA), anti glomerular basement membrane antibody (anti-GBM) and complement component 3 and 4 MEASUREMENT OF INTRAABDOMINAL PRESSURE(IAP) Intraabdominal hypertension is defined as IAP over 12 mm Hg Abdominal compartment syndrome (ACS) is defined as IAP over 20 mm Hg, associated with one or more organ failure (AKI) Intraabdominal hemorrhage, peritonitis, third spacing (abdominal surgery, ileus, pancreatitis) can cause ACS RENAL BIOPSY Renal biopsies are rarely performed in critically ill patients, mainly due to the perceived risk of bleeding complications and general lack of therapeutic consequences A renal biopsy may offer information that is not available through other means and should be considered if underlying parenchymal or glomerular renal disease is suspected ,particularly in case of persistent loss of kidney function, proteinuria greater than 3g/day or a clinical picture suggestive of a systemic disease where the benefits of a histological diagnosis outweigh the risks It has been suggested that transjugular renal biopsies may be safer than percutaneous or open techniques OTHER LAB TESTS Depending on the clinical context, the following tests may be indicated: • lactate dehydrogenase (LDH) (in case of suspected thrombotic thrombocytopenic purpura (TTP)) • serum creatine kinase and myoglobin (in case of suspected rhabdomyolysis) • fragmentocytes (in case of possible TTP / haemolytic uraemic syndrome (HUS)) • N-terminal pro-brain natriuretic peptide (NT-proBNP) and troponin (in case of suspected cardio-renal syndrome) • serum / urine protein electrophoresis (in case of suspected myeloma kidney) MANAGEMENT OF AKI KDIGO GUIDELINES FOR AKI MANAGEMENT High risk patients can either be detected using clinical risk scores, the measurement of new renal biomarkers or both. IV FLUIDS and RESUSCITATION Many patients suffer from absolute (in case of hypovolemic or hemorrhagic shock) or relative (in case of vasodilatory shock) volume depletion at admission, which are both risk factors for AKI – replace fluid In patients with sepsis, the surviving sepsis guidelines strongly recommend a minimum of 30 ml/kg of intravenous fluids during the initial resuscitative phase,but even in patients who benefit from fluid resuscitation in the early phase of septic shock, higher volume resuscitation may worsen outcome. In normovolemic or edematous patients, restrict fluid intake (~ 1500 ml/day) and sodium intake < 2gm/day. Input = Urinary + extrarenal + insensible losses In volume overload and non oliguric AKI diuretics are mainstay of treatment DIURETICS Loop diuretics such as furosemide may theoretically protect kidneys against ischemic injury by reducing renal tubular oxygen consumption and hasten renal function recovery by washing out necrotic debris blocking the tubules. Several RCTs assessed the potential efficacy of furosemide to prevent or treat AKI. A systematic review of these RCTs found no evidence that the use of diuretics reduces the incidence and the severity of AKI. Hence, diuretics should be used only with the goal to treat fluid overload HEMODYNAMIC MANAGEMENT Under normal conditions, renal blood flow (RBF) remains constant by autoregulation, a process that is impaired in pathological circumstances. In these patients, RBF is directly dependent on arterial pressure and consequently, a minimum perfusion pressure is required to prevent renal injury. The increasing awareness of the deleterious effects of fluid overload has also increased the reliance on vasopressors for restoring or maintaining MAP. The SEPSISPAM trial lower MAP targets in patients with vasodilatory shock seem safe, and MAP targets of 60-65 mmHg are acceptable in patients aged more than 65 years. In chronic hypertensive patients, higher MAPs may prevent the occurrence or progression of AKI so in these patients, the risk of cardiac arrhythmias must be outweighted against the risk of AKI progression. Renal perfusion and function may also be affected by the intra-abdominal pressure and tissue oedema that augments the hydrostatic pressure in the capsula of Gerota. Norepinephrine is an alpha-agonist that has also beta-agonistic effects resulting in increased contractility that may partly compensate for the vasoconstriction-induced increase in afterload. Norepinephrine is currently the first-line vasopressor in patients with septic shock and AKI Epinephrine may increase both cardiac output and perfusion pressure but is not recommended as first-line vasopressor because of its metabolic side effects (hyperglycemia, acidosis and hyperlactatemia), pro-arrhythmogenic properties and potential deleterious effect on the splanchnic circulation Dopamine - The surviving sepsis campaign recommends against dopamine for the treatment of septic shock. It also recommends against the use of low-dose dopamine for renal protection only Vasopressin (VASST and VANISH trial) DRUGS Avoid nephrotoxins when possible Adjust dose of all renally excreted drugs except in early sepsis. Withold NSAIDs and ACE inhibitors Avoid magnesium containing drugs (eg antacids and milk of magnesia) RENAL REPLACEMENT THERAPY Refractory Hyperkalemia Severe pulmonary oedema (diuretic resistance fluid overload) Poisoning by dialysable agent Metabolic Acidosis Uraemia The duration of decreased urine output is not per se an indication to initiate RRT within the first 48h following severe AKI. The consequences of oligo-anuria (AKI) are much more important for the decision to start RRT. CONTRAST INDUCED NEPHROPATHY(CIN) Defined as an absolute increase in serum creatinine of 0.5 mg/dl or a relative increase of 25% from the baseline within 48 to 72 hours of contrast exposure. RISK FACTORS Pre-existing renal insufficiency Diabetic Nephropathy Volume depletion Diuretic use Large contrast dosage (>2ml/kg) High osmolar contrast agents CHF and Hepatic failure Age >60 years CIN PREVENTION No specific treatment for radiocontrast induced nephropathy Volume expansion with normal saline or isotonic bicarbonate (3 ml/kg bolus over 1 hour prior to procedure, followed by 1ml/kg/hr for 6 hours post exposure) Avoid high osmolar contrast agents Discontinue diuretics, ACE inhibitors, NSAIDs and other nephrotoxic drugs for 24 h postprocedure N-Acetylcysteine( 4 dosage of 600- 1200 mg PO every 12 h with 2 dosage before and 2 dosage after procedure) THANK YOU