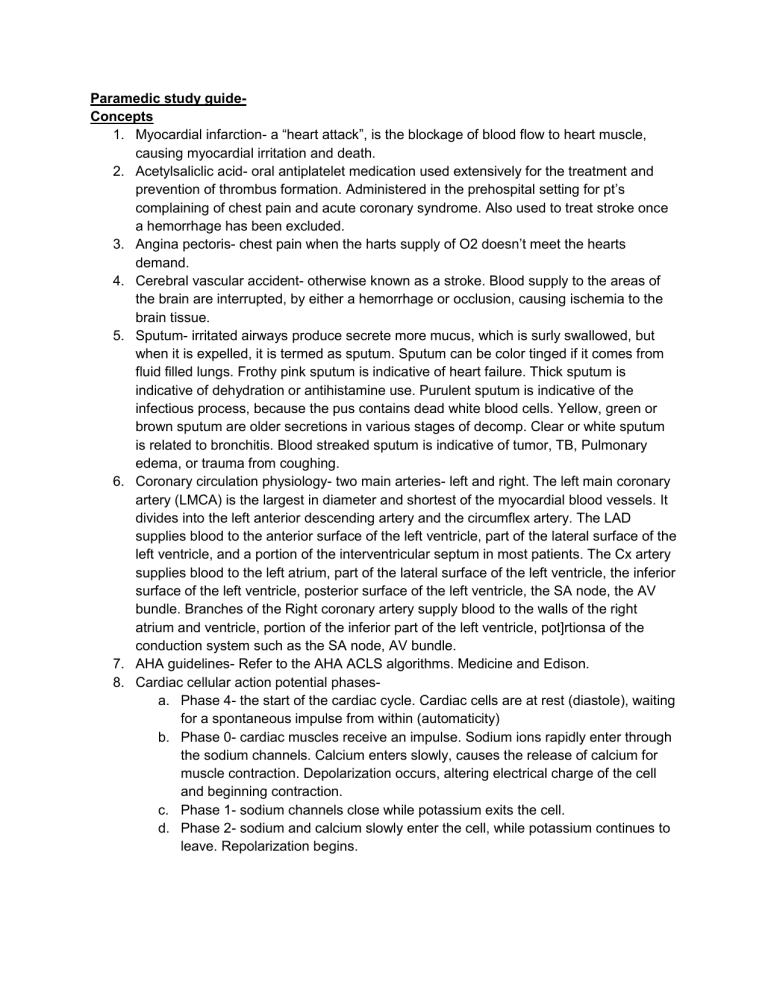
Paramedic study guideConcepts 1. Myocardial infarction- a “heart attack”, is the blockage of blood flow to heart muscle, causing myocardial irritation and death. 2. Acetylsaliclic acid- oral antiplatelet medication used extensively for the treatment and prevention of thrombus formation. Administered in the prehospital setting for pt’s complaining of chest pain and acute coronary syndrome. Also used to treat stroke once a hemorrhage has been excluded. 3. Angina pectoris- chest pain when the harts supply of O2 doesn’t meet the hearts demand. 4. Cerebral vascular accident- otherwise known as a stroke. Blood supply to the areas of the brain are interrupted, by either a hemorrhage or occlusion, causing ischemia to the brain tissue. 5. Sputum- irritated airways produce secrete more mucus, which is surly swallowed, but when it is expelled, it is termed as sputum. Sputum can be color tinged if it comes from fluid filled lungs. Frothy pink sputum is indicative of heart failure. Thick sputum is indicative of dehydration or antihistamine use. Purulent sputum is indicative of the infectious process, because the pus contains dead white blood cells. Yellow, green or brown sputum are older secretions in various stages of decomp. Clear or white sputum is related to bronchitis. Blood streaked sputum is indicative of tumor, TB, Pulmonary edema, or trauma from coughing. 6. Coronary circulation physiology- two main arteries- left and right. The left main coronary artery (LMCA) is the largest in diameter and shortest of the myocardial blood vessels. It divides into the left anterior descending artery and the circumflex artery. The LAD supplies blood to the anterior surface of the left ventricle, part of the lateral surface of the left ventricle, and a portion of the interventricular septum in most patients. The Cx artery supplies blood to the left atrium, part of the lateral surface of the left ventricle, the inferior surface of the left ventricle, posterior surface of the left ventricle, the SA node, the AV bundle. Branches of the Right coronary artery supply blood to the walls of the right atrium and ventricle, portion of the inferior part of the left ventricle, pot]rtionsa of the conduction system such as the SA node, AV bundle. 7. AHA guidelines- Refer to the AHA ACLS algorithms. Medicine and Edison. 8. Cardiac cellular action potential phasesa. Phase 4- the start of the cardiac cycle. Cardiac cells are at rest (diastole), waiting for a spontaneous impulse from within (automaticity) b. Phase 0- cardiac muscles receive an impulse. Sodium ions rapidly enter through the sodium channels. Calcium enters slowly, causes the release of calcium for muscle contraction. Depolarization occurs, altering electrical charge of the cell and beginning contraction. c. Phase 1- sodium channels close while potassium exits the cell. d. Phase 2- sodium and calcium slowly enter the cell, while potassium continues to leave. Repolarization begins. e. Phase 3- calcium channels slowly close and calcium leaves the cell while potassium channels open, enabling the rapid movement of potassium out of the cell. Repolarization ends. 9. CPAP- noninvasive means of providing ventilators support for pt’s experiencing respiratory distress. 10. MOA for cardiac medicationsa. Class 1 antidysrhythmic meds- Sodium channel blockers- allow the movement of sodium through channels in certain cardiac cells. Class 1A- prolongs QRS and QT intervals. Class 1B- resolves ventricular dysrhythmias and suppresses ectopic foci. b. Class 2- Beta-adrenergic block agents- competitively inhibit catecholamine (epi and norepinephrine) activation at the beta receptor sites. Affects HR, contractility, cardiac contraction, velocity. c. Class 3- Potassium channel blockers- increase phase 1,2,3 of cardiac conduction cycle. Prolong cellular action potential, prolong refractory period, treating atrial or ventricular tach. d. Class 4- Calcium channel blockers- reduce BP, control HR and decrease hearts demand for O2 during ischemia. Displace calcium and certain receptor sites . Relaxes the smooth muscle present in the heart. Slow conduction through AV node, decrease automaticity of ectopic foci, decrease velocity fog cardiac contraction. e. Adenosine- treats SVT, assists with identifying p or flutter waves. f. Alpha adrenergic receptor antagonists- “alpha blocker”- prevent endogenous catecholamines from reaching the alpha receptors, primarily in the smooth muscle of blood vessels. LOwer BP (diastolic), decrease SVR. g. Anticholinergic meds- block ACh at synapse in the central and peripheral nervous system. Inhibit parasympathetic nervous system by selectively blocking the binding of ACh to receptor sites. h. Anticoagulants- Decrease clotting ability of the blood. i. Antiplatelet- Keeps blood clots from forming by preventing blood platelets from sticking together. j. ACE inhibitors- Expands blood vessels and decreases resistance by lowering levels of angiotensin II. Allows blood to flow more easily and makes the hearts work easier or more efficient. k. Angiotensin II receptor blockers (inhibitors)- Prevent the chemical from having any effect on the heart or blood vessels, keeps BP from rising. l. Digitalis preparations- increases the force of the hearts contraction. Beneficial for HF and irregular heart beats. m. Diuretics- causes the body to rid itself of excess fluids and sodium through urination. Reduces the hearts workload. n. Catecholamines and sympathomimetics- stimulate the receptor sites in the sympathetic nervous system. 11. Effects of vagal nerve stimulation- slows HR down. 12. Cardiac electrical conduction system- Starts at the SA node (receives blood from RCA), spreads through three pathways- Bachman bundle, Wenkebach tract, Thorel. Next is the Av node. The AV junction (gatekeeper to the ventricles) is comprised of the AVE node and the bundle of His.next, are the secondary pacemakers. These fire normally from the SA-AV node tact, or if the SA and AV nodes aren’t working, these can fire on their own. These secondary pacemakers include the Purkinje fibers. The accessory pathways are extra heart muscle tissue that connects the atria and ventricles, bypassing the AV node. These include- James pathways, Mahaim fibers, bundled of Kent. (These accessory pathways was can trigger abnormally fast heart rates.) 13. Pharmacologic Therapy for cardiogenic shock- Treatment focuses on strengthening contractility without increasing the heart rate, altering preload and afterload, and controlling any dysrhythmias that are contributing to shock. Vasoactive IV medications to treat cardiogenic shock include: Dopamine, Norepinephrine, Epinephrine. 14. Starlings law- effects on intrathoracic pressure on cardiac output- increased venous return augments preload. Heart muscle fiber stretch in response to the expanded volume (preload) before contracting. The stretching of the muscle fibers allows the heart to eject more forcefully the additional volume, thereby boosting the stroke volume. So, in the normal heart, the greater the preload, the greater the force of the ventricular contraction, and the greater the stroke volume, resulting in increased CO. 15. Effects of intrathoracic pressure on cardiac output- Increases in intrathoracic pressure decreases left ventricular afterload and will augment left ventricular ejection. In patients with hypervolemic heart failure, this afterload reducing effect can result in improved left ventricular ejection, increased cardiac output and reduced myocardial O2 demand. 16. Signs and symptoms of stroke- Language- Slurred speech, aphasia, agnosia, apraxia. Movement- hemiparesis, hemiplegia, arm drifting, facial droop, tongue deviation, swallowing difficulties, ptosis, ataxia. Sensory- Headache, sudden blindness, sudden unilateral parathesia. Cognitive effects- decreased LOC, difficulty thinking, seizures, coma. Cardiac- Hypertension. FAST mnemonic to assess for stroke- F- facial droop. Aarm drift. S- Speech impairment. T- time is critical-call 9-1-1 Skills 1. Differentiate and react hemodynamically unstable or a symptomatic arrhythmia. Hemodynamically unstable- Edison. (TCP for unstable bradycardia, Synchronized cardioversion for wide complex tach with a pulse, defibrillator for wide complex tach with no pulse). Hemodynamically stable- medication.(atropine for bradycardia, amiodarone for wide complex tach, adenosine for SVT narrow complex tach). 2. DIfferentiate diastolic and systolic heart failure- Systolic: left ventricle can’t connect completely. Heart won't pump forcefully enough to move blood throughout your bodyheart failure with reduced ejection fraction(HFrEF)-too stretched and weak to pump. Diastolic: heart isn’t able to relax normally between beats, tissue on the left ventricle is too stiff to relax. Heart failure with preserved ejection fraction (HFpEF). 3. Identify chest pain without cardiac origin- Gastroesophageal reflux disease (GERD) or Acid reflux, muscle or bone problems in the chest wall or spine, Lung conditions or diseases of the pleura, the tissue that cover the lungs, Pulmonary embolism (sharp pinpoint chest pain), stomach problems (ulcers), stress, anxiety or depression. 4. Interpret 3 (4 leads) and 12 lead ECG’sa. 4 Leadi. Identify Heart rate ii. Identify Heart Rhythm iii. P waves? (0.08 - .11). iv. PR interval. (0.11 - 0.20) v. QRS complex. (0.06 - 0.11) b. 12 Leadi. Rate- Slow? Fast? ii. Rhythm- Reg? Irreg? Reg Irreg? Irregularly irregular? iii. P wave- 1-1 ratio? Morphology? PR interval? iv. Q- QRS width, voltage v. R- R to R progression vi. S- ST elev? Depression? vii. T- T wave morphology? Inversion? QTc? viii. U- U waves present? (Oh dear) c. Multiple ways to interpret 12 leads. “I See All Leads”, “Big Lie, Little Lie, Say All”= ( L(1)I(2)I(3),x(AVR)L(AVR)I(AVF), S(V1)S(V2)A(V3), A(V4)L(L)L(V6)). 5. Differentiate between cardiac compromise verse compensatory reactiona. Cardiac compromise- refers to any kind of heart problem. Patients may complain of chest pain, flu-like symptoms, or dyspnea(difficulty breathing). The most common complaint is chest pain. The pain may radiate down an arm with the left arm more commonly involved. b. Compensatory reaction- As the heart begins to fail, the body’s compensatory mechanisms attempt to improve CO by manipulating the following: Preload, Afterload, Cardiac contractility, Heart rate. Ultimately, compensatory mechanisms may worsen heart failure. 6. Treat a beta blocker overdose- For cases of beta-blocker poisoning where symptomatic bradycardia and hypotension are present, high-dose glucagon is considered the first-line antidote. AGE- atropine, glucagon, epi. 7. Treat chest pain of cardiac origin- ACLS ACS syndromes algorithm. a. Symptoms suggestive of ischemia or infarction i. EMS assessment and care and hospital prep- Assess ABC’s. Be prepared to provide CPR and Dfib. 1. Administer ASA and consider O2, Nitro, Morphine (fentanyl) if needed. 2. Obtain 12 lead ECG; if ST elevation- Notify receiving hospital with transmission or interpretation; note time of onset band first medical contact. 3. Provide prehospital notification; on arrival, transport to ED/bath lab per protocol. 4. Notified hospital should mobilize resources to respond to STEMI 5. If considering prehospital fibronolysis, use fibronolytic checklist. ii. Concurrent ED/catch lab assessment (<10 min) 1. 2. 3. 4. 5. 6. 8. Activate STEMI team upon EMS notification Assess ABC’s give O2 if needed Establish IV access Preform brief ; targeted history, physical exam Review/complete fibrinolytic checklist; check contraindications Obtain initial cardiac marker levels; complete blood counts and coag studies 7. Obtain portable chest x-ray (<30 minutes); do not delay transport to the catch lab iii. Immediate ED/catch lab and general treatment 1. If O2 sat <90%, start oxygen at 4 L/min, titration 2. Aspirin 162 to 3254 mg (if not given by EMS) 3. Nitro sublingual or trans lingual 4. Morphine IV if discomfort not relieved by nitro 5. Consider administration of P2Y12 inhibitors iv. ECG INTERPRETATION 1. ST elevation or new or presumably new LBBB; strongly suspicious for injury a. STart adjunctive therapies as indicated b. Do not delay reperfusion c. Time from onset of symptoms less than or equal to 12 hours? i. If less than 12 hours, reporfusion goals: therapy defines by pt and center criteria. FMC- to - balloon inflation (PCI) goal of less than 90 min. Door to needle (fibronolysis) goal of 30 min. d. If greater than 12 hours- troponin elevated or high risk ptconsider early invasive strategy if: i. Refractory ischemic chest discomfort ii. Recurrent/persistent ST deviation iii. VTACH iv. Hemodynamically instability v. Signs of heart failure vi. Start adjunctive therapies- Nitro, Hep as indicated. 2. NON-ST-elevation a. ST depresssion or dynamic T-wave inversion, transient ST elevation;strongly suspicious for ischemic and /or high-risk score (SEE 1D) b. Normal ECG or no diagnostic changes in ST segment or T wave; low risk score i. Consider admission to ED chest pain unit or to appropriate bed for further monitoring unit and possible intervention. treat unstable Vs stable cardiac treatment: Unstable cardiac: identify the rhythm and then treat symptomatic bradycardia starting with medication ( atropine 0.5mg bolus, rpt 3-5 min, max 3mg) ( dopamine 2-20 mcg/kg per min, titrate to effect taper down slowly) (EPI IV infusion 2-10 mcg per min infusion. Titrate to PT response) if no response to medication consider base and TCP or synchronized cardioversion/unsynchronized/defibrillation. Stable cardiac: pharmacology, pain management, O2, ALS vitals, Nitro, ASA EMT Concepts 1. Dyspnea/nocturnal dyspneaa. Dyspnea- Difficult or labored breathing, b. Nocturnal dyspnea- dyspnea that comes on suddenly in the middle of the night and may be an ominous sign of left-sided heart failure. 2. Pulseless electrical activity (PEA)- electrical activity is present on ECG but there are no pulses or BP. 3. Cardiac Dysrhythmias- syncope, diaphoresis, chest pain, pain radiating to back/arm, palpitations, ALOC, a. Sinus Tachycardia b. SInus Bradycardia c. AFib d. AFlutter e. SVT f. WPW g. VT h. VFib i. Sinus Arrythmis j. Sinus Exit Block k. Sinus Arrest l. Sinus with PAC m. Paced Atrial n. NSR with 1st block o. 2nd degree block type 1 p. 2nd degree block type 2 q. Second degree block 2:1 r. 3rd degree AV block s. NSR with PJC t. Junctional u. Acell junctional v. Junctional tachy w. Wandering pacemaker x. NSR with PVC y. Idioeventricular z. Paced Ventricular 4. Cerebrovascular accident (CVA)/Stroke-otherwise known as a stroke. Blood supply to the areas of the brain are interrupted, by either a hemorrhage or occlusion, causing ischemia to the brain tissue. 5. Angina/Angina Pectoris-Pain felt in the chest when the supply of oxygen in the heart doesn’t meet the hearts needs. Stable and unstable. 6. Hypertension (HTN)/Hypotensiona. HTN- High blood pressure, usually a diastolic pressure of greater than 90mmHg b. Hypotension- Low blood pressure, reads lower than 90 mmHg systolic, 60 mmHg diastolic. 7. Return of spontaneous circulation (ROSC)- Return of spontaneous circulation is the resumption of a sustained heart rhythm that perfuses the body after cardiac arrest. It is commonly associated with significant respiratory effort. Signs include breathing, coughing, or movement and a palpable pulse or a measurable blood pressure. 8. American Heart Association guidelines (AHA)- Refer to ACLS algorithms for treatment plan based on pt. 30-2-compressions per 2 breaths. 9. Shockable rhythms and indications for an AED- Shockable rhythms include pulseless ventricular tachycardia or ventricular fibrillation. Indications for an AED include any situation where the responder feels as though the pt has no pulse or is not breathing, i.e. Medical emergencies for unconscious/unresponsive. 10. Pathophysiology of left-sided-heart failure- Left-sided heart failure occurs when the left ventricle doesn't pump efficiently. This prevents your body from getting enough oxygenrich blood. The blood backs up into your lungs instead, which causes shortness of breath and a buildup of fluid. 11. Anatomy of the cardiovascular system- three main components: the heart, the blood vessel and the blood itself. The heart is the system's pump and the blood vessels are like the delivery routes. Blood can be thought of as a fluid which contains the oxygen and nutrients the body needs and carries the wastes which need to be removed. Left and right atrium, left and right ventricle, pericardium, myocardium, endocardium. 12. Pathophysiology of acute coronary syndrome- the inhibition of blood flow to the coronary arteries due to thrombus, atherosclerosis, coronary artery spasm, arteriosclerosis, shock, dysrhythmia, PE. Without blood flow to these arteries, the heart cannot function (pump) properly. 13. Complications of electrical injuries and treatmenta. Complicationsi. Cardiac arrest due to the electrical effect on the heart.- run it like a code ii. Muscle, nerve, and tissue destruction from a current passing through the body. iii. Thermal burns from contact with the electrical source. Treat as burn, fluids, cover, airway. iv. Nerve damage, ALOC. Skills 1. Differentiate between left sided and right sided heart failure-Systolic: left ventricle can’t connect completely. Heart won't pump forcefully enough to move blood throughout your body- heart failure with reduced ejection fraction(HFrEF)-too stretched and weak to 2. 3. 4. 5. 6. 7. 8. pump. Diastolic: heart isn’t able to relax normally between beats, tissue on the left ventricle is too stiff to relax. Heart failure with preserved ejection fraction (HFpEF). Differentiate between types of strokesa. SIchemic stroke- occurs when blood vessels supplying blood to the brain is obstructed. It accounts for 87% of all strokes. b. Hemorrhagic stroke- occurs when weakened blood vessel ruptures. The two types of weakened blood vessels that usually cause this are aneurysms and arteriovenous malformations. The most common cause of this type of stroke is uncontrolled HTN. c. TIA (transient Ischemic Attack)- called “mini stroke”, caused by a serious temporary clot. A warning, and needs to be taken seriously. d. Cryptogenic stroke- In most cases, a stroke is caused by a blood clot that blocks the flow of blood to the brain. In some instances, despite testing, the cause of a stroke cannot be determined. A stroke of unknown cause is called a “cryptogenic stroke.” e. Brain Stem Stroke- When stroke occurs in the brain stem, it can affect both sides of the body and may leave someone in a ‘locked-in’ state. When a locked-in state occurs, the patient is generally unable to speak or move below the neck. Evaluate chest pain without cardiac origin-Gastroesophageal reflux disease (GERD) or Acid reflux, muscle or bone problems in the chest wall or spine, Lung conditions or diseases of the pleura, the tissue that cover the lungs, Pulmonary embolism (sharp pinpoint chest pain), stomach problems (ulcers), stress, anxiety or depression. Identify cardiogenic shock- Cardiogenic shock is a serious condition that occurs when your heart cannot pump enough blood and oxygen to the brain, kidneys, and other vital organs.the most common cause is heart attack. Identify chest pain not in cardiac origin- Gastroesophageal reflux disease (GERD) or Acid reflux, muscle or bone problems in the chest wall or spine, Lung conditions or diseases of the pleura, the tissue that cover the lungs, Pulmonary embolism (sharp pinpoint chest pain), stomach problems (ulcers), stress, anxiety or depression. Identify stroke- Sudden numbness or weakness in the face, arm, or leg, especially on one side of the body. Sudden confusion, trouble speaking, or difficulty understanding speech. Sudden trouble seeing in one or both eyes. Sudden trouble walking, dizziness, loss of balance, or lack of coordination. Sudden severe headache with no known cause. a. F—Face: Ask the person to smile. Does one side of the face droop? b. A—Arms: Ask the person to raise both arms. Does one arm drift downward? c. S—Speech: Ask the person to repeat a simple phrase. Is the speech slurred or strange? d. T—Time: last time seen normal? If you see any of these signs, transport emergently. Administer prescribed cardiac medication-10 rights, make sure there are no contraindications for med, recheck the doe, med and name on bottle to conform it matches the pt. Treat hypotension pt- O2, IV fluid, Vasopressor depending on the severity. Identify and treat underlying cause of hypotension- treat for the type of shock that the pt has. 9. Treat for return of spontaneous circulation (ROSC)a. Maintain O2 sat of less than or equal to 94% b. ETCO2 monitor c. Avoid hyperventilation d. Treat hypotension-IV/IO bonus, vasopressin infusion, consider treatable causes e. 12 lead, coronary reperfusion f. Targeted temp management