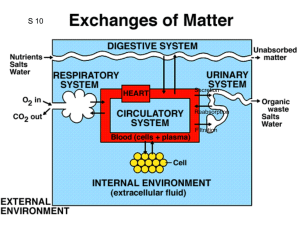
Chapter 25 Body water 60% of body weight, less in women cuz more fats With prolonged heavy exercise, urine output decreases but sweat increases Intracellular fluid is 40% - 28L Extracellular is 20% - 14L Interstitial fluid 11L Plasma 3L - higher protein concentration Blood is 5L - 2L RBC Osmotic pressure (pi)- amount of pressure preventing osmosis from a semipermeable membrane; pi = CRT (C - solutes concentration, R - gas constant, T absolute temperature in K) Isotonic = having the same osmotic pressure 19.3 mmHg force per 1mOsm/L solution Isotonic solution - 0.9% saline, 5% dextrose Isotonic solution - same osmolarity as a cell Hypertonic - more osmotic substances than the cell Intracellular swelling - hyponatremia, lack of nutrition → Na ions stay in the cell → water influx Acute - cell water increases Chronic - cel ions decrease Hypernatraemia - dehydration or no ADH (diabetes insipidus) Extracellular edema - leakage of fluids to the interstitial space and lymphedema (lymphatics do not bring fluid to blood) Kf is the capillary filtration coefficient (the product of the permeability and surface area of the capillaries), Pif is the interstitial fluid hydrostatic pressure, pc is the capillary plasma colloid osmotic pressure Too increased filtration → edema In heart failure capillary pressure is increased, reduced blood flow triggers RAAS and water retention Safety factors: Low tissue compliance (3 mmHg) if Pif is negative, if interstitial V ↑ → Pif increases Lymph flow can increase (7mmHg) which decreases protein concentration and lowers net filtration force, washdown of interstitial fluid concentration (7 mmHg) ● Most fluid in the interstitium is in gel form in a proteoglycan mesh and it has negative pressure. When P becomes positive, there is free fluid - pitting edema Combined - 17mmHg safety factor Chapter 26 Excretion = Filtration – Reabsorption + Secretion Vasa recta - peritubular capillaries supply the renal medulla Micturition - the urinary bladder empties Ureters - renal pelvis to bladder, pushed by parasympathetically elicited peristaltic contractions Detrusor bladder muscle Sacral plexus - pelvic nerves (Six Ps ● ● ● ● ● ● nerve to piriformis (S1-S2) perforating cutaneous nerve (S2-S3) posterior femoral cutaneous nerve (S1-S3) parasympathetic pelvic splanchnic nerves (S2-S4) pudendal nerve (S2-S4) perineal branch of S4 (S4) SLIP, DSP ● ● ● ● ● ● ● S: superior gluteal nerve L: lumbosacral trunk I: inferior gluteal nerve P: posterior femoral cutaneous nerve D: direct branches to lateral rotators (including nerve to piriformis, nerve to obturator internus, nerve to quadratus femoris, etc), and pelvic floor S: sciatic nerve P: pudendal nerve) Pudendal nerve can inhibit the external sphincter and cause urination Filtration fraction (renal blood flow that is filtered) = 0.2 Filtration fraction = GFR/Renal Plasma Bloodflow Pg - hydrostatic inside capillaries = 60mmHg Pb - opposes filtration = 18 Pig - colloid pressure inside capillaries, opposes filtration = 32 Pib - around zero, no effect Urine stones ↑Pb ↑arterial colloid pressure or ↑filtration fraction (that concentrates the plasma proteins) →↓GFR Glomerular capillary hydrostatic pressure (Pg) is controlled by arterial pressure, afferent arteriole resistance (decreases it) and efferent arteriole resistance (increases it) Control: SNS decreases GFR (constricts arterioles) Epireprine too Endothelin constricts arterioles Angiotensin II constricts efferent arterioles ♥ →↑GFR Increases Na+ reabsorption in the proximal tubule (aldosterone does it in the distal) Prostaglandins prevent the afferent arterioles from being constricted ANP is opposite to RAAS, it decreases sodium reabsorption, it is released upon cardiac stretch ENDO ↑GFR Prostaglandins might dampen angiotensin response on afferent arterioles (aspirin blocks them → ↓GFR) Prerenal - decreased pressure in glomerular capillaries Renal - filtration is affected Postrenal - increased pressure in Bowman's -- pressure build up Tubuloglomerular feedback - ↓BP→↓Na →↓afferent arterioles resistance which ↑Pb and ↑renin Myogenic response - how arteries react to increase or decrease in blood pressure, when smooth muscle cells are stretched, they contract to resist the pressure. Autoregulation Dilation of afferent arterioles increases GFR Decreased GFR increases reabsorption in proximal → less Na+ for distal → macula densa raises piG ↑protein ↑GFR cuz ↑amino acids reabsorption and ↑NACl proximal reabsorption → ↓Cl to macula densa and ↓afferent arterioles resistance Renin is stored in juxtaglomerular cells in the afferent arterioles Chapter 27 Reabsorption: Transcellular route - through membranes Paracellular route - junctional spaces between cells Ultrafiltration → bulk flow through peritubular capillaries (large reabsorptive force, moving from interstitium to blood) Na-K pump on basolateral membrane brings Na to interstitium and K in the cells K rich foods - bananas, oranges, spinach, potatoes, peas, zucchini, avocado, oatmeal Secondary active glucose and AA reabsorption Na diffuses through electrochem gradient, the energy is used to push glucose Transport maximum - max rate of reabsorption ADH determines water reabsorption in distal tubules and ducts Descending loop of henle makes fluid hyperosmotic Ascending loop is impermeable to water but reabsorbs solutes Early distal tubule - diluting segment - 100mOsm/L osmolarity Late distal tubules and cortical collecting tubules: Principal cells (aldosterone acts on them) - potassium sparing happens, K leaves the cell, sodium is reabsorbed Type A intercalated cells, they eliminate H+ and reabsorbs bicarbonate, reabsorb K as well. this is important in acidosis Type B intercalated cells - secrete bicarbonate, important in alkalosis Aldosterone controls Na reabsorption in the distal convoluted tubules Made in the adrenal gland, angiotensinII stimulates aldosterone release Medullary collecting ducts determine final urine output Permeable to urea with transporters →raises osmolarity Secretes H ions No aldosterone →Addison’s → Na loss Conn’s → too much Na → K depletion Angiotensin II: - Stimulates aldosterone secretion - Constricts efferent arterioles which ↑filtration fraction due to ↓renal blood flow →↑reabsorption - Directly stimulates Na Reabsorption Reduces medullary blood flow through vasa recta Atrial Natriuretic peptide ↓Na reabsorption, opposes RAAS Parathyroid hormone ↑Ca reabsorption Renal clearance CX is renal clearance in milliliters per minute, UX V is the excretion rate of substance X (UX is the concentration of X in the urine, and V is urine flow rate in milliliters per minute), and PX is the plasma concentration of X. Creatinine clearance = GFR Rate of filtration = GFR* Plasma concentration Rate of excretion = Ux* Urine volume Chapter 28 ADH makes it permeable to water so water can be reabsorbed, this decreases urine volume but does not alter solute excretion Dilute urine - ↓ADH Concentrated urine: ↑ADH and ↑osmolarity of renal medulla Secreted from pituitary gland, also called vasopressin Countercurrent multiplier - using energy to generate an osmotic gradient that enables water reabsorption Build up of solute concentration in the renal medulla due to: - Active transport from ascending Henle limb - Active transport from collecting ducts - Diffusion of urea - Less water diffusion Vasa recta preserves hyperosmolarity of renal medulla - minimizes solute loss because it flows slowly Osmolar clearance - the rate of which solutes are cleared from the blood - Cosm , V is urine flow rate Free water clearance - difference between water excretion (urine flow rate) and osmolar clearance C(h20) = V-Cosm Disorders of concentration ability: Central diabetes insipidus - ↓ADH secretion Nephrogenic diabetes insipidus - kidneys do not respond to ADH Osmoreceptor-ADH Feedback system - Osmoreceptor cells in hypothalamus stimulate pituitary, ADH is released and the solutes are diluted Cardiovascular reflex stimulation - upon reduced BP or volume (ADH is not very sensitive to blood volume loss) Thirst - due to increased extracellular fluid osmolarity and decreased volume, as well as angiotensin II Aldosterone and Angiotensin II control Na excretion, not Na plasma concentration because - They increase water reabsorption - Thirst and water intake compensate for Na concentration Renal Regulation of Potassium, Calcium, Phosphate, and Magnesium; Integration of Renal Mechanisms for Control of Blood Volume and Extracellular Fluid Volume - 223-235 Chapter 29 Potassium - 4.2mEq/L in ECF, most rapidly moves into the cells with the help of insulin and aldosterone, also during alkalosis, exercise releases K from skeletal muscle Mostly regulated by secretion in distal and collecting tubules in the principal cells by: 1. Passive diffusion from blood to interstitium 2. Na-K pump into cells 3. From cell interior to tubular fluid Factors: ↑K concentration increases secretion ↑aldosterone→↑secretion ↑flow rate→↑secretion Type A intercalated cells can absorb it and type B can secrete it Alkalosis increases secretion Calcium - in bones Parathyroid hormone ↑reabsorption of bone salts, activates vitamin D (that stimulates intestinal Ca+ absorption) PTH reduces excretion, greater phosphate plasma concentration stimulates that Stimulated by acidosis Extracellular fluid - dependent on NaCl Excretion = Glomerular filtration - tubular reabsorption Intrarenal buffering mechanisms: 1. Glomerulotubular balance - ↑reabsorption if ↑GFR (the ability of the nephron to reabsorb) 2. Macula densa feedback - ↑NaCl delivery causes afferent arteriole constriction →↓GFR Pressure Natriuresis Pressure diuretics - ↑arterial pressure→↑water excretion Loss of fluid from plasma to interstitial space (edema) due to ↑capillary pressure, ↓plasma colloid pressure, ↑ capillary permeability ↑SNS activity reduces Na and water excretion due to renal vasoconstriction, increased reabsorption and ↑renin which helps reabsorption ADH guides and increases water reabsorption A lot of Na intake → Inhibited SNS activity increases secretion ↑Atrial natriuretic peptide that decreases reabsorption Suppressed formation of angiotensin II ↑in arterial pressure → pressure natriuretics Increased ECF and blood volume: Heart failure - low pressure, kidneys retain fluid → pulmonary edema Pregnancy increases vascular capacity, varicose veins too → ↑blood volume Increased ECF but normal blood volume: Nephrotic syndrome - loss of plasma protein reduces plasma colloid osmotic pressure → edema cuz capillaries filter larger volumes that decrease plasma volume Liver cirrhosis - decreased plasma protein synthesis Kidney lecture notes: Fraction of filtrate reabsorbed by kidneys - 99% Glomerular filtration -Autoregulation - despite local increase in blood pressure, the GFR remains the same. Happens in the afferent arterioles - The myogenic mechanism is how arteries and arterioles react to an increase or decrease of blood pressure to keep the blood flow within the blood vessel constant. Tubuloglomerular feedback is an adaptive mechanism that links the rate of glomerular filtration to the concentration of salt in the tubule fluid at the macula densa. A high [NaCl] ---- keeps the GFR constant Glomerulotubular balance (GTB) is defined as the ability of each successive segment of the proximal tubule to reabsorb a constant fraction of glomerular filtrate and solutes delivered to it. -- difference? PRA = plasma renin activity Volume regulation is the first reaction if the drink is isotonic and not pure water The effect of RAAS decreases if Na+ uptake increases Thiazide diuretics lead to hypokalemia Insulin deficiency leads to hyperkalemia Hyponatraemia x Cockcroft-Gault Calculator performs best for estimating kidney function Lecture physiology 1 mol NaCL = 58.5g → calculate a gram Volume is not determined by filtration but by Na+ reabsorption