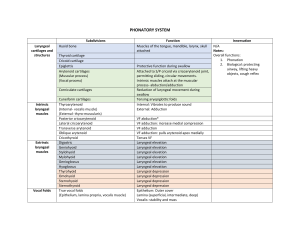
Applied Head and Neck Module The Pharynx & Larynx Disorders Firas M. Hassan Assistant Professor Department of Otolaryngology College of Medicine , University of Kufa, Iraq Disorders of the pharynx Adenoid Mass of lymphoid tissue Produce IgA, IgG, IgM Maximal size 3-8 years (then regress) Enlargement with viral/bacterial infections Adenoid Effects of Enlargement Nasal obstruction Mouth breathing Hyponasal speech Feeding difficulty (esp. infants) Snoring/Obstructive Sleep Apnoea Eustachian tube obstruction Recurrent acute otitis media (earache) Chronic otitis media with effusion (glue ear, reduced hearing) Adenoid Assessment Difficult! Post-nasal space x-ray Post-nasal mirror Fibre-optic endoscope Theatre Obstructive Sleep Apnoea • Spectrum from mild snoring to OSA • Partial/Complete airway obstruction during sleep – turbulent airflow • Over 30 apnoeic episodes in 7 hours of sleep • 5 apnoeic episodes/hour • Daytime tiredness • If severe can cause hypoxia and increase cardiovascular strain Otitis Media Acute Chronic Ventilation Tube Adenoidectomy • Curettage (blind) • Suction diathermy (mirror) Complications • Bleeding • Atlanto-occipital joint dislocation • Eustachian tube stenosis Nasopharyngeal Carcinoma • More common in Chinese population • Usually SCC • TNM staging • Radiotherapy • Limited role for chemotherapy & surgery Tonsillitis Acute Recurrent acute Chronic Tonsillectomy Indications • Recurrent tonsillitis (5/year for at least 2 years) • Previous peritonsillar abscess (quinsy) • Suspected cancer (unilateral enlargement/ulceration) • Obstructive sleep apnoea syndrome Tonsillectomy Risks • GA • Bleeding (primary or secondary) approx. 3% • Infection Technique • Cold steel instruments • Electrosurgery • Laser Pharyngeal Pouch • Posterior herniation of pharyngeal mucosa • Occurs through Killian’s dehiscence – Between inferior constrictor and cricopharyngeus Reasons • Weaker area • Incoordination of pharyngeal phase of swallowing • Cricopharyngeal spasm Disorders of the larynx Recurrent Laryngeal Nerve Palsy Idiopathic Laryngeal cancer Thyroid disease (benign or malignant) Trauma (including iatrogenic – ie. thyroidectomy) Cervical lymphadenopathy Oesophageal cancer Apical lung cancer Aortic aneurysm Neuropathic (diabetes) Hypopharyngeal/Laryngeal Carcinoma Hypopharyngeal • 90% are SCC • Uncommon disease • • • • • Post-cricoid (pharyngooesophageal junction) • Piriform fossa • Posterior pharyngeal wall Laryngeal Over 95% are SCC Commonest H+N Ca in West M:F 5:1 Smoking and Alcohol • Supraglottis • Glottis (good prognosis) • Subglottis (poor prognosis) Hypopharyngeal/Laryngeal Carcinoma History • • • • • • • • FB sensation in throat Dysphagia Odynophagia Otalgia (refered pain – vagus) Hoarseness (spread to RLN/Larynx) Coughing (aspiration, haemoptysis) Weight loss Smoking history (pack/years) Hypopharyngeal/Laryngeal Carcinoma Examination • Loss of laryngeal crepitus (fixed larynx) • Cervical lymph node metastasis • Fibre-optic endoscopy Investigations • Barium swallow (for dysphagia symptoms) • CT/MRI (Head, Neck, Chest) • Direct pharyngo-laryngo-oespohagoscopy and biopsy Hypopharyngeal/Laryngeal Carcinoma • TNM staging • MDT meeting “multidisciplinary teams for cancer “ Management • Radiotherapy +/- chemotherapy • Surgery – Laryngectomy – Pharyngo-laryngectomy – including radical or selective neck dissections • Palliation Summary • Nasopharynx – Adenoid hypertrophy – snoring/OSA, glue ear – Carcinoma • Oropharynx – Tonsillitis/Tonsillectomy • Hypopharynx and Larynx – Pharyngeal Pouch – Recurrent Laryngeal Nerve Palsy – Carcinoma • Thyroid surgery – Iatrogenic LN injury