Thyroidectomy
advertisement

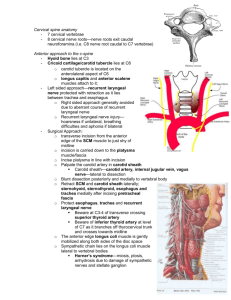
Tony Tuan H. Nguyen, MD June 8, 2010 Post-Thyroidectomy Considerations Indications: FNA findings of definite/suspicious/inconclusive for malignancy; goiter; thyroid cancer (papillary, follicular, medullary, anaplastic); thyroid nodule; hyperthyroidism; Grave's disease Cancer (50%): papillary (80%); follicular (10%); medullary (5%); anaplastic (1%); lymphoma (1%) Benign lesions (50%): nontoxic goiter (20%); thyrotoxicosis (10%); thyroiditis (5%); benign nodules (5%); other (10%) Demographics: 15-80yo, Male:Female 1:8 Routine Procedure: Time: 1-2 hours. Blood loss: 50-70ml Postop Considerations: Hypoparathyroidism (↓ Ca+ +): 3–5% - Presents 24-48 hours postop. - Trousseau's sign: Inflate blood pressure cuff. After 3 minutes, you will get carpopedal spasms - Chvostek's sign: Tap on facial nerve and you will elicit facial nerve spasms - Acute Mild Symtoms: fatigue, hyperirritability, anxiety, depression peri-oral numbness, paresthesias of the hands and feet, muscle cramps) - Acute Severe Symptoms: carpopedal spasm, laryngospasm, and focal or generalized seizures, generalized tonic muscle contractions secondary to severe tetany (<4.3 mg/dL), no neuromuscular symptoms. - Hypotension, EKG changes (prolonged QT, U waves, flat or inverted T waves) Hematoma: 1–2% - Airway compromise: immediate drainage and/or reintubation Thyroid storm (usually in association with Graves' disease) - Life-threatening exacerbation of hyperthyroidism occurring during periods of stress - Hyperthermia (> 40°C), tachycardia, widened pulse pressure, anxiety, altered mental state → psychosis → coma, and myopathy (rhabdomyolysis in 50%; severe in 4%). - Mistaken for malignant hyperthermia, sepsis, anaphylaxis, neuroleptic malignant syndrome. - Treatment: oxygen, fluid, electrolyte correction, cooling blankets, acetaminophen. o Propylthiouracil to block synthesis by blocking thyroid peroxidase and iodinase o Methimazole to block thyroid peroxidase o Sodium iodide to block release by negative feedback on anterior pituitary to inhibit release of TSH and thyroid hormone (give after PTU, otherwise you may get iodine escape) o Steroids (hydrocortisone or dexamethasone) to block peripheral conversion o ß-blockers (propranolol) to block peripheral effects and peripheral conversion Wound infection: 0.2–0.5% Recurrent laryngeal nerve damage Unilateral (hoarseness): 0.77% Bilateral (aphonia, respiratory obstruction): 0.39% Vagus - - Superior laryngeal nerve o external branch – motor to the cricothyroid muscles (tenses vocal cords for high pitch sound) o internal branch – sensory to the interior of the larynx to the level of the subglottic space Recurrent laryngeal nerve – motor to all muscles of larynx (except cricothyroid) sensory to subglottic area **All intrinsic muscles of the larynx are innervated by the recurrent laryngeal nerve of CN X except cricothyroid which is innervated by the superior laryngeal nerve Recurrent laryngeal nerve (Unilateral) injury to leads to hoarsenss. Recurrent laryngeal nerve (Bilateral) injury leads to unopposed cricothyroid muscles -> airway obstruction Superior laryngeal nerve injury leads to hoarseness and presdisposes to aspiration