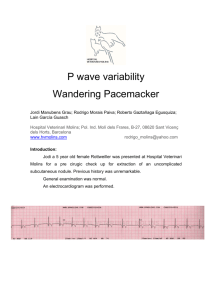
Atrial Fibrillation -No identifiable P waves -Irregular R-R -Random (can be fast, regular, or slow) atrial spikes -loss of atrial kick -MOST COMMON NORM CAUSE OF CVD Alcohol, infection, caffeine Wandering Pacemaker -normal overall rate -P wave shape varies (at least 3 different P wave shapes) -Irregular R-R -Atrial rate is <100 bpm Multifocal Atrial Tachycardia (MAT) -P wave shape varies -Irregular R-R (ventricular rhythm) -Atrial rate is >100 bpm - common in pulmonary issues (COPD) -digoxin toxicity *fibrillations are all the atrial foci randomly firing; only some make it through to ventricles (QRS) *irregularly shaped P waves may be hidden by rapid rate (Rate is much faster in MAT than in wandering pacemaker) Atrial Escape Beat/ Rhythm 60 – 80 bpm Pause followed by: Pointed or normal P wave Normal QRS Junctional Escape Beat/ Rhythm 40 – 60 bpm Pause followed by: NO P wave or inverted Normal QRS Ventricular Escape Beat/ Rhythm < 40 bpm Pause followed by: NO P wave Wide QRS > .12 Usually no P because no atrial depolarization Can be because of parasympathetic activity Premature Atrial Beats/ Contractions (PAC) Irregular R-R Unusually shaped P wave followed by a QRST Beat comes BEFORE compensatory pause P wave and reg. rhythm reset after one cycle *P’ may be hidden in previous T wave�look for T taller than others Premature Junctional Beats/ Contractions Irregular R-R NO P wave/inverted P wave Slightly widened QRS (or normal) Beat comes BEFORE pause Premature Ventricular Beats/ Contractions (PVC) Irregular R-R NO P wave Wide and deep QRS Beat comes BEFORE compensatory pause Cause: HYPOXIA Atrial Flutter “Saw Tooth” Multiple P waves, not all followed by QRS P P P P P QRS P P P Regular: R to R the same Numbers indicate a ratio of # of P waves to QRS Baseline vanishes between flutters Supraventricular Tachycardia (SVT) Narrow QRS (b/c coming from above ventricles) No P waves (hidden by preceeding T waves) Can be atrial or junctional (PAT or PJT) (narrow PR interval) Regular R-R **big diff b/w a fib Rate: 150-250 Has a subtype: paroxysmal atrial tachycardia (PAT) meaning it is intermittent SVTs *usually regular, but it can vary in # of P waves sometimes Ventricular Tachycardia (VT) (BAD) Tosades de Pointes Ventricular Fibrillation (WORST!) Wolff-ParkinsonWhite Syndrome (WPW) First degree Second degree, Type I (Wenkebach) Wide QRS >=3 consecutive PVCs No visible P wave REGULAR 1 irritable foci Long QT interval 250-350 bpm Series of ventricular complexes Due to hypomagnesium “twisted ribbon” outline Causes: low K, meds, congenital QT Can develop into Vfib NO identifiable waves/pattern “bag of worms” Ventricles are twitching CARDIAC ARREST Rapid discharge of multiple irritable ventricular foci Immediate CPR and defibrillation Delta wave Wide QRS BASE (>0.12s) Short PR interval Impulse is getting to ventricles from SA node Reentrant rhythm PR interval >0.2 seconds PR length is consistent Think delay Long PR interval – lengthens in successive cycles Irregular R-R Dropped QRS “Long, longer, longer, drop, now you’ve got a Wenkebach” Not dangerous *push immediate MgSO4 and then find the cause *Hypoxia sets in and causes sustained damage & scarring *NOT obvious on EKG Second degree, Type II (Mobitz or Mobitz type II) PR intervals consistent Dropped QRS Occurs below AV DANGEROUS; need a pacemaker Third degree Multiple P waves and a lot less QRS complexes R-R equal P-P equal * Some P waves are hidden in other waves Will not be sinus because things are out of order Right Bundle Branch Block (RBBB) Left Bundle Branch Block (LBBB) - RT ventricular dep. is delayed - CLASSICAL APPEARANCE: - Wide QRS - “Rabbit ears” in V1 and V2: R-R’(prime) - Slurred S wave in I and V6 - LT ventricular dep. is delayed - CLASSICAL APPEARANCE: - Wide QRS - “Rabbit ears” in V5 & V6: R-R’(prime) - Wide, deep, downward deflection in V1 & V2 MISCELLANEOUS WPW (WolfeParkinson-White) Wide QRS BASE Delta wave Short PR interval Long and narrow unslurring Impulse is getting to ventricles rom SA node Asystole Straight line Artifact Looks like Afib, but it is not because R-R equal Occurs if person is moving or lead not pushed on well EKG must be redone REGULAR Common causes: Movement, electrical interference, breathing heavy (heart moving) Atrial pacing/ Pacer Spikes Ventricular pacing/ Pacer Spikes If pacer spike happens before the P wave Straight up and down lines that doesn’t look like a wave Wide QRS Pacer spike appears before QRS Wandering Baseline Brugada “Rollercoaster” Caused by respiratory distress and movement Baseline is not uniform Young men famHx SCD V1/2 tenting/ski slope Wellen’s waves Deep, symmetrical t waves Pending STEMI Take to cath lab Hyperkalemia Elevated potassium Peaked t waves � wide QRS Hypokalemia Low potassium Hypercalcemia High calcium QT interval = short Hypocalcemia Low calcium QT interval = long