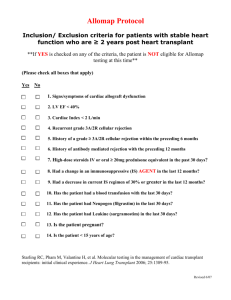
Transplantation in plastic surgery Dr. S. Vijay Kannan History In 1954, Dr. Joseph E. Murray, Plastic surgeon - first successful kidney transplant between identical twins. In 1958, human leukocyte antigen (HLA) In 1960, 6-mercaptopurine and its precursor azathioprine (AZT) by Charles Zukosi and Roy Calne Nomenclature • VCA - Vascularised Composite Allograft • CTA - Composite Tissue Allotransplantation • Autograft • Isograft • Allograft • Xenograft • Orthotopic - anatomically same • Heterotopic - different site Transplant Immunology • • • • • The major histocompatibility complex (MHC) genes code the strongest transplant antigens. Human MHC molecules called human leukocyte antigens (HLAs) are coded by a group of genes located on the short arm of chromosome 6. MHC class I molecules (HLA-A, HLA-B, and HLA-C) are expressed on all nucleated cells and generally present endogenous antigens Class II molecules (HLA-DP, HLA-DQ, and HLA-DR) are constitutively expressed only on antigen- presenting cells (APCs), including dendritic cells, macrophages, and B-cells. HLA match in kidney transplants is HLA-DR > HLA-B > HLA-A, respectively. NON-HLA ANTIGENS: • ABO BLOOD GROUP ANTIGENS • • triggers hyperacute rejection of the organ due to the presence of the preformed hemagglutinin A and/or B antibodies. MINOR HISTOCOMPATIBILITY ANTIGENS • Recognized by CD8 cytotoxic T-cells, leading to graft rejection. • H-Y MiHA is encoded by the Y chromosome in males • Mitochondrial proteins and enzymes ALLORECOGNITION PATHWAYS • • Direct pathway - recipient’s T-cells recognize the intact allogeneic HLAs expressed by the donor cells. • Immediate post-transplant period • Acute cellular rejection Indirect pathway - T-cells recognize peptides derived from the donor HLAs presented by the recipient APC. • • Late onset of rejection & Chronic rejection. Semi-direct pathway - the recipient dendritic cells or other APCs, acquire the intact HLAs from the donor cells and present them to the recipient T cells. T-CELL ACTIVATION B-CELL ACTIVATION • B cells express antigen-specific receptors as immunoglobulins on their surfaces. • When these receptors bind donor HLA antigens in the presence of helper T cells (CD4 Th2) - B cells are activated. + • • They divide, differentiate, and become plasma cells to secrete antibodies. • Some activated B cells become memory B cells HLA antibodies bind antigens and can cause graft injury • • • activating the complement cascade (complement-dependent cytotoxicity) via the Fc receptor on natural killer (NK) cells, neutrophils, and eosinophils (antibody-dependent cellular cytotoxicity). In addition to producing antibodies, B cells act as APCs. - Indirect pathway REJECTION • • • It is an inflammatory process developed by a specific immunologic response to the allograft antigens. 85% of hand and face recipients experienced at least one episode of acute rejection in 1st yr Hyperacute rejection - very rapidly within a few minutes after transplantation and represents the classic example of the antibody-mediated rejection process • • associated with the preexisting antibodies against the MHC of donor cells. Accelerated rejection - 24 h and 5 days post transplantation. • • • The increased risk of developing an accelerated phase of rejection arises from sensitization of the allograft recipient, for example, by a previous allograft. classic, humoral mediated response; it precedes T-cell- dependent mechanisms, IgM, IgG, C3, fibrin and leukocyte infiltrations interstitial hemorrhages, vascular thrombosis, and leukocyte infiltrations. ACUTE REJECTION • Within a few days to a few weeks • Cell-mediated process and arises from the activation of T cells • • • • Morphologic evidence of tissue injury: fibrinoid necrosis of arteries, aggregation of the platelets leading to vascular obstruction. Immunopathologic evidence: presence of complement factor 4 (C4) deposition Serologic evidence: circulating antibodies to the donor human histocompatibility antigens (HLA) or other endothelial antigens Components of acute composite allograft rejection include vasculitis, dermatitis, myositis, and perineural involvement – confirmed through the skin biopsy specimens. CHRONIC ALLOGRAFT VASCULOPATHY (CHRONIC REJECTION) • Slow process that occurs over months and/or years • The frequency of chronic allograft vasculopathy correlates • acute rejection episodes • recipient sensitization • insufficient MHC-antigen matching • recipient age and race • inadequate immunosuppression • hypertension • cytomegalovirus (CMV) infection/ reactivation • prolonged ischemia time of the graft before transplantation • smoking and hyperlipidemia. • • • • • Endothelial injury of the affected vessels Inflammatory cascade, allograft arteriosclerosis and graft fibrosis. Cardinal feature : luminal obliteration. Blockage occurs due to the proliferation of the smooth muscle cells Finally interstitial fibrosis leads to allograft dysfunction. IMMUNE TOLERANCE The ultimate goal of transplantation science is to make genetically diffe • Clonal deletion : T cells that express a TCR specific for a certain antigen are eliminated. • • Anergy: state in which T cells are alive but unable to respond to the antigen stimulation. • • • • occur in the thymus (central deletion) or extra thymically (peripheral deletion). induced by the lack of co-stimulatory signals - leads to apoptosis. Two major co-stimulatory interactions that take place between a T cell and antigenpresenting cell involve CD28/B7 and CD40L/CD40 pathways. The blockade of these second signals using antibodies to specific receptors (CD40R, B27) to induce a peripheral form of tolerance. “Prope” (almost) tolerance - introduced by Calne • • defined as the donor- specific hypo responsiveness under a low dose of immunosuppressive therapy. leads to reduced immunosuppression-related side effects and allows for improved allograft survival without episodes of acute or chronic rejection. Immunotherapy Immunosuppressive medications must inhibit the body’s ability to reject a transplanted organ, but not at the expense of the defense network against pathogens. • • • Induction protocols : to prevent allograft recognition during the peritransplantation period. Maintenance regimen: to maintain the transplant. Rescue agents : when ongoing rejection occurs, it is often necessary to use to stop ongoing rejection and salvage a transplant that would otherwise be lost. Immunotherapy Mechanism of action SKIN TRANSPLANT Skin allograft • In large burns either in combination with autograft or in isolation. • Along with autograft shows improved healing in comparison to autologous graft alone. • Preservation with glycerol reduces the antigenicity of skin allografts and prolongs graft survival. • Production of antibodies that may inhibit the possibility of future VCA. • 1 limiting factors: harvesting and banking services are not uniformly available, and significant risk of disease transmission, susceptible to rejection Skin xenograft • • Porcine xenograft has been used as a temporary dressing in large burns with seeding of autologous grafts beneath it limited use : susceptible to hyperacute rejection. Bone allograft • • • • Frozen bone allograft commonly used for the reconstruction of long bone defects Acts as scaffold for ingrowth of osteocytic precursors that repopulate the donor scaffold by creeping substitution. Problems: • susceptible to stress fracture and loosening of metal fixation devices. • Vascularized allogeneic bone is susceptible to immunologic rejection. Removal of marrow by irradiation or by replacement with recipient marrow has been shown experimentally to prolong allograft survival. Cartilage allograft • • • • • Chondrocytes express HLA antigens on their surface and are immunogenic & matrix is only weakly antigenic. Surgical scoring or dicing with resultant exposure of allogeneic cells has been shown to hasten reabsorption of allogeneic cartilage. After irradiation pretreatment - used for volume augmentation in the facial skeleton. Initial good results in a large number of patients but long-term data suggest a high rate of resorption. Bovine-derived cartilage xenografts are susceptible to xenogeneic mechanisms of rejection, which results in poorer outcome in comparison to either allogeneic or autogenous cartilage grafts. Nerve allograft • • • • • Nerve autograft has a limited number of donor sites. In large nerve defects, nerve allograft has been used in a small number of patients. Immunologic rejection of nerve allograft can be prevented with immunosuppression & decellularizing techniques Immunosuppression needs to be administered only while the recipient axons traverse the allograft and can then be terminated. Decellularizing techniques : cold preservation, radiation, lyophilization, and freeze thawing Current clinical protocol involves 7 days of cold preservation of the nerve allografts at 4–5°C in University of Wisconsin solution prior to implantation HAND TRANSPLANTATION History In 1964, the first hand transplant was performed by Dr. Gilbert in Ecuador. • The patient was a bilateral upper extremity amputee that received a single hand transplant. he was given azathioprine and prednisone for immunosuppression. The patient experienced acute rejection and underwent amputation 3 weeks post-transplant. In 1998, the first modern hand transplant was performed by Dr. Jean-Michel Dubernard and colleagues in Lyon, France. • The patient was a 48-year-old male amputation at the mid- forearm level in 1984. The donor was a 41-year-old brain dead beating heart donor. The surgery was a technical success, but the patient was non- compliant with his postoperative immunosuppression and rehabilitation regimen and elected to have his transplanted hand amputated in 2001. In 1999, second hand transplant by Dr. Warren Breidenbach and his team at the University of Louisville. • The patient was a 37-year-old male who lost part of his dominant forearm and whole hand in a fireworks accident. He currently has the longest surviving transplant Hand Recipient Criteria Hand Donor Criteria Pre OP workup Team Flow of events 1. PATIENT SCREENING 2. PREOPERATIVE PLANNING 3. CADAVER REHEARSAL 4. TEAM ASSIGNMENTS 5. OPERATING ROOM SET-UP 6. DONOR OPERATION 7. RECIPIENT OPERATION 8. POSTOPERATIVE COMPLICATIONS 9. REHABILITATION 10. OUTCOMES Donor Operation • Under tourniquet control • Incision is outlined • • • • • • medial/volar component dissection down through the nerves to the brachial artery/veins. The brachial artery is isolated. It is ligated proximally and distal control is obtained. Cannulate the artery and this is secured with suture. The veins are clipped or ligated proximally and cut distally. anterior to posterior dividing muscle Disarticulation of elbow or osteotomy through the humerus. Back-table dissection: perfusion solution is instilled. The solution is instilled until at least 500 mL have been infused or all effluent is clear. • Closure of the skin of the arm stumps. • donor is then fitted with a prosthetic hand • RECIPIENT OPERATION Standard incisions made 90° to the incisions used on the donor to ensure Z-plasty such as interdigitation postoperatively. • OSTEOSYNTHESIS • MUSCLE/TENDON RECONSTRUCTION • extensor reconstruction first followed by flexor reconstruction. • NERVE RECONSTRUCTION • REVASCULARIZATION • • • • no more than 7–8 h of cold ischemia have elapsed. few vena comitans or deep veins and most superficial veins are left open until after reperfusion has been performed to allow efflux of the initially perfusing blood until the blood becomes brighter red then remaining open veins are then anastamosed. The final vein to artery ratio is typically 2 or 3 : 1. SKIN CLOSURE Immunotherapy • • • Currently, there is no standard immunosuppressive regimen established for extremity transplantation Induction therapy : polyclonal (antithymocyte globulin, ATG) or monoclonal (alemtuzumab or basiliximab) Maintenance therapy with triple-drug therapy. • • • Calcineurin inhibitor - to prevent early activation of T cells (e.g., tacrolimus) Antimetabolite agent - to prevent lymphocyte proliferation (e.g., mycophenolate mofetil) Steroid (e.g., prednisone). Early Complications Surgical Medical Vessel thrombosis Pneumonia Hematoma Sepsis Skin necrosis Nonsurgical infections Adverse medication Arteriovenous fistulae reactions Acute limb loss REHABILITATION OUTCOMES Hand Transplantation Score System, HTSS. • 100-point scale that evaluates six functional areas: 1. appearance (15) A total score • 81 to 100 points - excellent 3. movement (20) • 61 to 80 - good 4. psychological and social acceptance (15) • 31 to 60 - fair 5. daily activities and work status (15) • 0 to 30 - poor. 2. sensibility (20) 6. patient satisfaction and general wellbeing (15). Face Transplant History The world’s first partial face transplant was done in November 2005 - prof. Jean Michel Dubernard on a 38-yearold Isabella Dinoire after being bitten by a dog. First, full-face transplant was done in 2010 by a team led by Dr. Barret on Óscar who lost his facial structure by road traffic accident Types Partial facial transplantation • It consists of nose, lips, and amounts of chin and cheek. • It requires sensory and motor nerve anastomoses Full-face transplant • It consists of whole face transfer from donor to recipient. Classification Indication Patients having disfigured face by means of: • Accidents/traumatic injury, • Burn. • Birth defects/congenital defects. • Facial structures lost due to infection which are untreatable with conventional surgical technique. Recipient eligibility Donor eligibility Surgical team Multidisciplinary approach • • • Reconstructive surgeon - Plastic surgeon and oral & maxillofacial surgery, Orthodontist, psychiatrist, otolaryngologist, infectious disease specialist, ophthalmologist social worker, nutritionist, physiotherapist, pain medicine specialist Immunotherapy OUTCOMES Outcomes can be classified into several categories: • • • • Medical (immune-related, metabolic and hematologic derangements, opportunistic infections, neoplastic growth) Functional (speech, smell, airway, taste, mastication, sensory reinnervation, facial animation, pain relief) Aesthetic (patient and physician satisfaction, contour, scarring, identity preservation) Social (psychosocial reintegration, cost-effectiveness). Benefits of facial transplantation 1. Improved functionality • ability to breathe, swallow, speak, smile, and show other emotions. 2. Rehabilitation of appearance • Restoration of a near-normal facial appearance gaining the confidence to return to their former lifestyles including social activities and jobs. 3. Pain reduction and discomfort Complications • • • • • Mood swings following transplant surgery. Psychiatric support must be proved to the patients before and after partial facial transplantation. Rejection. Identity issues - will take up a new look different from donor or recipient Risks of taking transplant drugs for a lifetime • Infections. • Diabetes. LARYNGEAL ALLOTRANSPLANTATION Absence of a larynx is associated with the loss of a human sounding voice, an impaired sense of taste and smell, a disposition to a high risk of lower bronchoalveolar infection, and psychosocial disintegration. The first clinical attempt at laryngeal transplantation was in 1969. • A 62-year-old man with carcinoma of the larynx was the recipient of a larynx from a 40-year-old donor. Unfortunately, the patient died due to tumor recurrence at postoperative month 8. The first successful laryngeal allograft procedure took place in 1998. • The recipient was a 40-year-old man who had been in a road accident 20 years previously, resulting in laryngeal dysfunction. A laryngopharyngeal complex, including thyroid, parathyroid, and five rings of the trachea was transplanted. INDICATIONS Not a lifesaving one and is only intended to improve quality of life. The ideal recipients • young trauma victims. • large benign tumor • low-grade malignant tumor resection. DONOR PROCEDURE • • The entire pharyngolaryngeal complex together with upper 5–6 tracheal rings and thyroid and parathyroid glands is harvested, leaving the neurovascular pedicle intact. The vascular pedicle includes the superior thyroid arteries, the internal jugular veins as an extension of the superior and middle thyroid veins, the superior laryngeal nerves, and the recurrent laryngeal nerves bilaterally. RECIPIENT PROCEDURE • The entire vascular and neural structure of the larynx is delineated. • An orthotopic position for transferred tissue is created by removing the strap muscles. • • • • • A pouch is created for the pharynx and larynx and pharyngeal anastomosis is established in the upper part the upper part of the tracheal stroma is revised, the donor trachea is sutured to this in an end-to-end manner. Both superior thyroid arteries are anastomosed to the recipient arteries (end-to-end), or to a branch of the external carotid arteries (end-to-side). Donor internal jugular veins are anastomosed to the recipient internal jugular veins (end-toend or end-to-side) Both superior laryngeal nerves and recurrent laryngeal nerves of the transplanted tissue are sutured to their recipient matches. IMMUNOSUPPRESSIVE PROTOCOL • Drugs: 1. muromonab-CD3 (5 mg/day) 2. cyclosporine (500 mg/day) / tacrolimus 4 mg twice daily 3. methylprednisolone (50 mg/day, decreasing to 20 mg in 4 days) 4. mycophenolate mofetil (MMF) (1 g twice a day). • Wide-spectrum antibiotic therapy should be administered for the first 10 postoperative days. 1. Sulfadoxine pyrimethamine - to prevent Pneumocystis carinii pneumonia. 2. CMV prophylaxis - by valganciclovir. ABDOMINAL WALL ALLOTRANSPLANTATION INDICATIONS • Impossible or high-risk direct abdominal closure in patients undergoing intestinal allotransplantation. ABDOMINAL WALL COMPOSITE TISSUE COMPONENT • The transplanted tissue includes one or both rectus abdominis muscles, overlying fascia, underlying sheet and abdominal subcutaneous tissue, and skin. ARTERIAL ANATOMY • The composite abdominal wall flap is perfused by the inferior epigastric vessels. These are left in continuity with the common femoral or iliac arteries. FLAP DESIGN • The surface area may range from 150 cm–500 cm, based on patient age and size. DONOR PROCEDURE • • • • An upper part Mercedes-like incision, which starts from median sternotomy to extend to the bilateral subcostal line. Then a continuous vertical bilateral incision is made in the lateral borders of both rectus abdominis muscles. In the groin region, the two incisions are connected transversely in the midline. Both inferior epigastric vessels are dissected and followed until common femoral vessels are identified. The length of the vascular pedicle is determined based on the desired length obtained. RECIPIENT PROCEDURE • • • • After reperfusion of the intestinal or multivisceral allograft, the composite allograft is transferred as a separate tissue. Vessels of the composite tissue are anastomosed to the iliac vessels in an end-to-side manner. The length of the pedicle is adapted in a smooth curve to prevent uneven tension or kinking. The transplanted abdominal tissue is incorporated into the edges of the recipient abdominal wall defect. IMMUNOSUPPRESSIVE PROTOCOL • • • Induction - Alemtuzumab (0.3 mg/kg) preoperatively, immediately postoperatively, and on postoperative days 3 and 7. Maintenance - Tacrolimus with a targeted serum level of 10 μg/L. In rejection attacks, corticosteroids are used in high doses. UTERUS TRANSPLANTATION INDICATIONS • Not a lifesaving one and is only intended to improve quality of life. The ideal recipient : 1. Age 18–45 2. Infertility related to the uterus 3. Desire for uterine transplantation 4. Medical impossibility of having a baby 5. Congenital uterine agenesis 6. Resection of the uterus due to hemorrhage or trauma except for malignant tumors 7. No history of major trauma or surgery likely to negative affect outcomes 8. Healthy organs and systems 9. Psychosocial stability 10.Good health with no contraindications for immunosuppressive agents 11.Informed concern regarding all adverse effects of immunosuppressive agents IMMUNOSUPPRESSIVE PROTOCOL • Induction period: Antithymocyte globulin and prednisolone. • Intraoperatively : Antithymocyte globulin is initiated at a dose of 2.5 mg/kg per day. • • • • Day of surgery: Prednisolone is started on the, at 1000 mg, and tapered down to 20 mg, 1 week postoperatively. On day 7: Tacrolimus is started (0.2 mg/kg per day with blood levels between 15 ng/mL and 20 ng/mL), On day 10: antithymocyte globulin is stopped Maintenance treatment : prednisolone (20 mg/ day); tacrolimus (blood levels between 15 ng/mL and 20 ng/mL for the first 3 months, then tapered to 7–10 ng/ mL at 6 months postoperatively) and mycophenolate mofetil (MMF) (2 g/day). References 1. Flaps & Reconstructive surgery, Wei Mardini, 2nd edition 2. Neligan Plastic surgery, 4th edition, volume 1 3. Grabb and Smith Plastic surgery, 7th edition 4. Hand Transplantation - A Review., Brendan J. MacKay, M.D., Elliot Nacke, M.D., and Martin Posner, M.D., Bulletin of the Hospital for Joint Diseases 2014;72(1):76-88 5. Face transplant: A revolutionary approach and role of dentist., Tanya Nandkeoliar, Kaushik Ranjan Deb., Journal of Advanced Clinical & Research Insights (2018), 5, 127–132 6. Quality Improvement in Facial Transplantation: Standard Approach for Novel Procedures Rami S. Kantar, MD; William J. Rifkin, BA; J. Rodrigo Diaz-Siso, MD; G. Leslie Bernstein, MPA; Eduardo D. Rodriguez, MD, DDS,. PRS Global Open • 2018 Thank you