- The Annals of Thoracic Surgery
advertisement

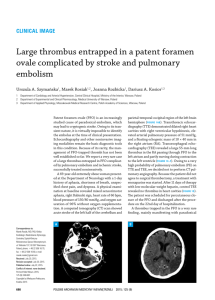
Embolus Entrapped in Patent Foramen Ovale: Impending Paradoxical Embolism Helena Podrouzkov a, MD, PhD, Vladimír Horv ath, MD, PhD, Ota Hlinomaz, MD, PhD, Jan Bedan, MS, Miroslav Bambuch, MD, PhD, Petr N emec, MD, PhD, and Marek Orban, MD International Clinical Research Center, Brno; Center of Cardiovascular Surgery and Organ Transplantation, Brno; VUT Brno, Brno; Tomas Bata Regional Hospital, Zlin, Czech Republic An impending paradoxical embolism is a rare finding, with fewer than 200 cases being documented so far. A 68-year-old woman, who presented with 3 weeks of increasing exertional dyspnea and exercise intolerance, underwent transesophageal echocardiography with a finding of an embolus in both right and left atria. At an emergent cardiac surgery, a worm-shaped, 5-cm-long thrombus was found in the right atrium, it was protruding to left atrium through the foramen ovale. The thrombus was removed intact, and the foramen ovale was closed. By our experience, an emergent cardiac surgery should always be considered as a treatment option for impending paradoxical embolism. (Ann Thorac Surg 2014;98:e151–2) Ó 2014 by The Society of Thoracic Surgeons P aradoxical embolization defined as passage of thrombotic masses through intracardiac or other shunts. It is usually a dangerous clinical situation associated with symptoms of systemic and pulmonary embolism. Relatively rarely, a moment when migrating thrombus entrapped in the shunt (typically patent foramen ovale) is seen and recorded during clinical examinations (including three-dimensional [3D] transesophageal echocardiography [TEE]) and consequently removed intact from cardiac chambers as it was in the presented case. Fig 1. Transesophageal two-dimensional echocardiography in high esophageal position (horizontal plane) showing a large thrombus (arrow) entrapped in patent foramen ovale. (LA ¼ left atrium; RA ¼ right atrium.) pressure in the pulmonary artery of 50 mm Hg. There was no regional wall motion abnormality in the left ventricle. Because of echo-dense structure in the right atrium, intracardiac thrombus was suggested and a TEE examination was recommended. TEE including 3D imaging revealed an embolus in the right and left atria, entrapped in patent foramen ovale (PFO; Fig 1). 3D transesophageal echocardiography confirmed the finding of impending paradoxical embolism in a relatively large PFO (Fig 2). Massive pulmonary embolism was shown by computed tomography, and emergent surgery was indicated. The results of a neurologic examination before surgery were negative with no signs of cerebral embolism. At an emergent cardiac surgery, a worm-shaped, 5-cm-long thrombus was found in the right atrium. It was attached to the interatrial septum, and it protruded to left atrium through foramen ovale. The thrombus was removed intact, and the foramen ovale was closed (Fig 3). Several thrombi were also removed from the left and right main branches of pulmonary artery. Two weeks after the An obese 68-year-old white woman presented with 3 weeks of increasing exertional dyspnea and exercise intolerance. Her cardiovascular history was unremarkable except for well-controlled hypertension. Two months before admission, the patient underwent umbilical hernia resection. In addition, the patient received a diagnosis and treatment for breast cancer 1 year before admission. On admission, the vital signs were normal, and the patient suffered no resting dyspnea. The physical examination revealed only minor varices in both lower extremities. TEE showed dilatation of the right ventricle with moderate tricuspid regurgitation and signs of moderate pulmonary hypertension, with an estimated systolic Accepted for publication Aug 29, 2014. Address correspondence to Dr Orban, Center of Cardiovascular Surgery and Organ Transplantation, Pekarska 53, 65691 Brno, Czech Republic; email: maor@post.cz. Ó 2014 by The Society of Thoracic Surgeons Published by Elsevier Fig 2. Three-dimensional echocardiographic image of the entrapped thrombus. 0003-4975/$36.00 http://dx.doi.org/10.1016/j.athoracsur.2014.08.072 e152 ET AL CASE REPORT PODROUZKOV A IMPENDING PARADOXICAL EMBOLISM Fig 3. Intraoperative image of intact wormlike thrombus removed from the patent foramen ovale. operation, the patient was discharged with oral vitamin K antagonist therapy. At 6-month’s follow-up, the patient was doing fine and had no complaints except for mild exertional dyspnea. Paradoxical embolism is defined by a transit of thrombi from the venous system into the systemic circulation. Typically, paradoxical embolism is associated with several underlying conditions. First, venous thrombosis usually presents with at least one thrombotic risk factor, such as hypercoagulable state, postoperative status, malignancy, or long-term bed rest. Second, the inevitable condition for paradoxical embolism is a communication between venous and systemic circulation. Most frequently, it is PFO or atrial septal defect. The third condition is a right-to-left pressure gradient, typically in the massive pulmonary embolism or intermittently during the Valsalva maneuver, allowing the thrombus to migrate from right to the left atrium. Paradoxical embolism presents as a coincidence of venous thrombosis with pulmonary embolism and systemic embolism. The most common manifestation of systemic embolism is a cerebrovascular event, such as stroke or transient ischemic attack. Other possible presentations of systemic embolism are peripheral vascular ischemia of embolic origin, acute myocardial infarction, and renal or abdominal ischemia. When the thrombus is large and the orifice of the venous to arterial shunt is Ann Thorac Surg 2014;98:e151–2 relatively small, the thrombus becomes stuck in the aperture and threatens with systemic embolism. This state is referred to as impending paradoxical embolism. Impending paradoxical embolism is a rare finding, with fewer than 200 cases being documented. It is also an extremely dangerous clinical setting, with an estimated mortality of 18% at 30 days. At the time of diagnosis, the systemic embolism is already present in 25% of cases [1]. Besides cerebral embolism, cases of coronary embolism [2], embolism into abdominal aorta and its branches [3, 4], or embolism into peripheral arteries of limbs [4] have been documented. The main cause of death in impending paradoxical embolism is cardiogenic shock with right heart failure owing to massive pulmonary embolism or a stroke [1]. Treatment options for impending paradoxical embolism include anticoagulation, thrombolysis, and surgery. According to an analysis of 174 cases with impending paradoxical embolism, surgical thrombectomy showed a nonsignificant trend toward improved survival and significantly reduced systemic embolism compared with anticoagulation alone. Thrombolysis and anticoagulation showed an increased prevalence of embolism after treatment initiation compared with surgery [1]. By our experience, an emergent cardiac surgery should always be considered as a treatment option. This study was supported by the European Regional Development Fund, Project FNUSA-ICRC (No. CZ.1.05/1.1.00/02.0123). References 1. Myers PO. Impending paradoxical embolism. Systematic review of prognostic factors and treatment. Chest 2010;137: 164. 2. Willis SL, Welch TS, Scally JP, et al. Impending paradoxical embolism presenting as a pulmonary embolism, transient ischemic attack, and myocardial infarction. Chest 2007;132: 1358–60. 3. Rousselle M, Ennezat P-V, Aubert J-M, et al. Momentarily stuck in the foramen ovale. Eur J Echocardiogr 2007;8:223–6. 4. Guo S, Roberts I, Missri J. Paradoxical embolism, deep vein thrombosis, pulmonary embolism in a patient with patent foramen ovale: a case report. J Med Case Rep 2007;1:104.