II. Burst pacing versus multiple premature stimulati
advertisement

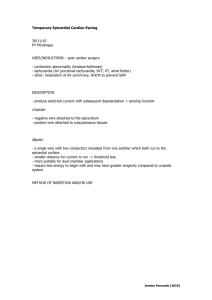
295 lACC Vol. 4, No.2 August 1934:295-304 EXPERIMENTAL STUDIES Reentrant Ventricular Arrhythmias in the Late Myocardial Infarction Period II. Burst Pacing Versus Multiple Premature Stimulation in the Induction of Reentry NABIL EL-SHERIF, MD, FACC, RAHUL MEHRA, PHD, WILLIAM B, GOUGH, PHD, ROBERT H. ZEILER, PHD Brooklyn. New York Isochronal maps of ventricular activation were analyzed in dogs 1 to 5 days after infarction utilizing a 64 channel multiplexer. Only dogs in which circus movement reentry could not be induced by a single premature stimulus were analyzed. Reentrant rhythms could be successfully induced equally by multiple (double or triple) premature stimuli and by burst pacing. Successive premature stimuli as well as successive beats during burst pacing resulted in progressively longer arcs of functional conduction block or slower circulating wave fronts, or both, that succeeded in reexciting myocardial zones on the proximal side of the arc of block to initiate reentry. However, for manifest reentry to be induced by burst pacing, the paced run had to be terminated after the heat that resulted in a critical degree of conduction delay. Otherwise, reentrant activation could be confined (con- Both properly timed premature stimulation and rapid pacing have been utilized to initiate possible reentrant rhythms in the experimental (1-3) and clinical (4-6) settings. The postinfarction canine heart is a documented experimental model for circus movement reentry (7-9). In these hearts, reentry could be induced by programmed premature stimulation and by runs of rapid pacing usually referred to as burst pacing (10), The mechanism of initiation of reentry by more than one premature stimulus has been described from analysis of ventricular activation maps (7,8). In an earlier study (3) that utilized composite electrode recordings, it was shown that initiation of reentry by burst pacing depends not only cealed) by the subsequent paced wave front, which could also arrive earlier to the reentrant circuit zone of slow conduction resulting in block and interruption of reentry. Termination of a paced run after this beat would not result in reentry. If the paced run was extended past this beat, a new sequence of ventricular activation patterns characterized by progressively longer arcs of block or slower conduction, or both, developed again. The number of beats in a paced run that could initiate reentry varied with the cycle length of pacing, as well as in different experiments, and was difficult to standardize. It is therefore concluded that random burst pacing as a technique for induction of reentrant rhythms should probably be abandoned in favor of multiple premature stimulation. on the cycle length of stimulation but also, critically, on the number of beats in the paced run. Burst pacing has been applied more frequently during the last several years in the clinical electrophysiology laboratory for initiation of ventricular arrhythmias (l0,11). The mechanism of initiation of reentrant rhythms by burst pacing and the relation of this technique to programmed premature stimulation are not well understood. Our study was undertaken to investigate this subject in dogs I to 5 days after infarction by analyzing ventricular activation maps. Methods From the Veterans Administration and State University of New York, Downstate Medical Center, Brooklyn, New York. This study was supported by the Veterans Administration Medical Research Fund. It was presented in part at the Annual Meeting of the American College of Cardiology Dallas, Texas, March 1984. Manuscript received November 15, 1983; revised manuscript received January 23, 1984, accepted February 9, 1984. Address for reprints: Nabil EI-Sherif, MD, Veterans Administration Medical Center, 800 Poly Place, Brooklyn, New York 11209. © 1984 r) the American College of Cardiology Downloaded From: https://content.onlinejacc.org/ on 10/01/2016 Experimental preparation. In eight mongrel dogs weighing 15 to 20 kg, the left anterior descending coronary artery was ligated just distal to the anterior septal branch. Details of the surgical technique have been described previously (12). The dogs were reanesthetized with sodium pentobarbital (30 mg/kg intravenously) 1 to 5 days after coronary artery ligation and received supplemental doses as 0735-1097/84/$3.00 296 rxcc Vol. 4, No.2 August 1984:295-304 EL-SHERIF ET AL. BURST PACING VERSUS MULTIPLE PREMATURE STIMULATION Table 1. Results of Programmed Premature Stimulation and Burst Pacing Experiment I 2 3 4 5 6 7 8 Programmed Premature Stimulation Burst Pacing* Induced Rhythms S,S2S3 S,S2S3 S,S2S3 S,S2S3S4 S,S2S 3S4 S,S2S3S4 S,S2S3S4 S,S2S 3S4 4,5, 10 5,9, 10 3,4,8 4, 5, 9, 10 4,8,9 5, 9 5,9, 10 4,5,9 MVT MVT PVR MVT PVR PVR, VF PVR, VF PVR, VF *Number of beats in a paced run that resulted in manifest reentry. MVT = monomorphic ventricular tachycardia (10 or more beats at a cycle length :::;300 ms); PVR = pleomorphic ventricular rhythm (two or more beats with more than two QRS configurations at a cycle length :::;300 ms); VF = ventricular fibrillation. required. Each dog was ventilated with room air through an endotracheal tube with a Harvard positive pressure pump, and the jugular vein was cannulated for the administration of fluids. Electrocardiographic lead II and femoral blood pressure were continuously monitored on an Electronics for Medicine DRIO electrophysiologic recorder. To slow the sinus rhythm, stimulation of the right or left vagosympathetic trunk was accomplished by delivery of 0.5 ms square wave pulses of 1 to 10 V intensity at a frequency of 10 to 20 Hz through two Teflon-insulated silver wires (0.012 inch [0.03 em] in diameter). The heart was exposed through a left thoracotomy and cradled in the opened pericardium. Ventricular pacing was achieved with use of two fine Tefloninsulated stainless steel wires (0.005 inch [0.013 em] in diameter) inserted by a 21 gauge hypodermic needle into the right ventricular wall. Both regular pacing and programmed premature stimulation were performed with a programmable digital stimulator (model DTU-lOl MVA, Bloom Associates, Ltd). The stimulator delivered rectangular pulses of variable duration (usually 2 to 5 ms) and twice diastolic threshold with an accuracy of up to alms interval. Stimulation protocol. Programmed premature stimulation. During regular ventricular pacing (SISI) at cycle lengths of 350 to 400 ms, single (S2), double (S2S3) or triple (S2S3S4) premature stimuli were introduced. A single premature stimulus (52) was introduced late in diastole, and the coupling interval was gradually shortened until a ventricular rhythm was initiated or until the effective refractory period of the right ventricular myocardium was reached. In all experiments in the present study, reentry required more than a single premature beat for initiation. In these experiments, 52 was introduced at an interval 5 ms longer than the effective refractory period and 53 was introduced at gradually shorter coupling intervals until S3 either provoked a response or reached refractoriness. If S3 failed to initiate reentry, its coupling was fixed at an interval 5 ms longer than the refractory period and an S4 was introduced at gradually shorter coupling intervals until a ventricular rhythm was initiated. In all experiments, reentry could be induced by double or triple premature stimulation. Downloaded From: https://content.onlinejacc.org/ on 10/01/2016 Burst pacing, Rapid ventricular pacing was applied during a slower sinus or spontaneous ventricular rhythm in the form of individual runs of 3 to 12 paced beats at a fixed cycle length, 5 ms longer than the effective refractory period of 52 (that is, a cycle length equal to the 5\5 2 coupling interval during multiple premature stimulation). This assured 1:1 capture during ventricular pacing. All paced runs were timed manually to start in the late diastolic interval during the slower spontaneous rhythm; and the cycle length preceding burst pacing was consistently longer than 350 ms. The complete burst pacing protocol was applied only at a single cycle length. In three experiments, activation maps were also analyzed during regular pacing at different cycle lengths longer than the one defined in the protocol. Figure 1. Electrocardiographic recordings from experiment 1 in which a reentrant tachycardia could be induced by double pre" mature stimuli (5 15253 , record A) and by burst pacing (BP). Burst pacing could initiate reentry only after paced runs with a critical number of beats (records B and D). See text for details. B __LW c -.l.!L_ _ BP BP D JACC Vol 4, No.2 EL-SHERIF ET AL. BURST PACING VERSUS MULTIPLE PREMATURE STIMULATION August 1%4:295-304 Epicardial isochronal maps. These were constructed from 62 simultaneous bipolar electrode recordings obtained with a sock electrode. A higher density of electrodes (approximately I) to 10 mm between pairs) covered the area of the infarction and the border zones, and a lower density (approximately 15 mm) covered the remaining surface of the heart. In some experiments, a patch electrode was also used to obtain epicardial recordings at a closer interelectrode distance (4 mm). Intramural recordings were obtained with specially designed 21 gauge needles. Details of the recording techniques, the mapping system and the methods for construction of epicardial isochronal maps were reported previously (7,8). After termination of the electrophysiologic study, the anatomic location of the infarction was determined and correlated with epicardial and intramural recordings. Results In three of the eight experiments, reentrant rhythms could be induced by S1S2S3 premature stimulation. In the remaining five experiments, S1S2S3S4 stimulation was required. In all experiments, reentrant rhythms could also be induced by burst pacing. However, manifest reentry was dependent on the number of beats in a paced run. The latter varied with the cycle length of pacing as well as from one experiment to the other. The cycle length of burst pacing ranged from 180 to 225 ms. Each programmed stimulation protocol was repeated twice and, with few exceptions, the results were reproducible. Reentrant beats with different QRS morphologic features (that is, pleomorphic) were induced in four of five experiments in which three premature stimuli as well as burst pacing were used and in one of the three experiments in which reentry was initiated by two premature stimuli. The pleomorphic configuration was due to varying sites of early reexcitation resulting in different ventricular activation patterns. In the remaining three experiments, a monomorphic rhythm was induced by both premature stimulation and burst pacing. In three experiments, a pleomorphic rhythm induced by burst pacing degenerated into ventricular fibrillation. In two of these experiments, ventricular fibrillation could also be induced by SIS2S3S4 stimulation. Results from all experiments are summarized in Table 1. Monomorphic ventricular tachycardia. Electrocardiogram. Figure 1 illustrates electrocardiographic recordings from experiment 1, in which a monomorphic reentrant tachycardia could be induced by both S1S2S3 premature stimulation and burst pacing. Record l A shows that during SIS1 stimulation at a cycle length of 350 ms, S2 and S3 stimuli were introduced at coupling intervals of 220 and 185 ms, respectively, and initiated a monomorphic ventric- ECG Figure 2. Epicardial isochronal maps during SlSZS3 premature stimulation and the first reentrant beat (V I) from the same experiment shown in Figure I (see text for details), In this and subsequent maps, the epicardial surface is depicted as if the ventricles were folded out after a cut was made from the crux to the apex. The top left and right borders represent the right and left atrioventricularjunctions. The two curvilinear surfaces on the right and left are contiguous and extend from the posterior base to the apex of the heart. The arcs of functional conduction block are represented by heavy solid lines and are depicted to separate contiguous areas that are activated at least 40 ms apart. The epicardial border of the infarction is delineated by the interrupted line on the S1 map. The isochronal maps are drawn at 20 ms intervals. ECG = electrocardiogram. Downloaded From: https://content.onlinejacc.org/ on 10/01/2016 297 SOOMS 298 EL-SHERIF ET AL. BURST PACING VERSUS MULTIPLE PREMATURE STIMULATION ular tachycardia at a cycle length of 220 to 230 ms. Burst pacing at a cycle length of 220 ms could initiate the ventricular rhythm only after paced runs of 4 (record IB), 5 or 10 beats (record ID) , but not with paced runs of 6, 7, 8 (record ici, 9, II or 12 beats. Epicardial isochronal maps . Figures 2 to 4 illustrate epicardial isochronal maps from the same experiment shown in Figure I . Figure 2 illustrates the epicardial maps during SlS2S3 premature stimulation and the first reentrant beat (VI) . The isochronal maps were drawn at 20 ms intervals. During SJ, the entire epicardial surface was activated within 80 ms, with the last isochrone located in the central part of the epicardial surface of the infarct (the latter is marked by the dotted line). During S2, an arc of functional conduction block (represented by the heavy solid line) developed inside ~t l '50DMS I lACC Vol. 4. No.2 August 1984:295- 304 the septal border of the infraction . The activation wave front circulated around the upper and lower ends of the arc of block . The central and apical parts of the epicardial surface of the infarct were the last to be activated at 120 ms. The second premature stimulus (S3) resulted in a much longer arc of conduction block inside the upper, septal, apical and lower lateral borders of the infarction. The activation wave front circulated around both ends of the arc of block, coalesced and then advanced slowly in a direction from the lateral to the septal border of the infarction. The slow wave front reached the distal side of the arc of block 200 rns from the onset of right ventricular activation before reactivating an area on the proximal side of the arc to initiate the first reentrant beat (V d. Epicardial activation during V 1 continued in the form of two circulating wave fronts around two _ 5,5 25354 V, V2 Figure 3. Epicardial isochronal maps during a four beat run of burst pacing that induced a reentrant tachycardia from the same experiment shown in Figures I and 2. See text for details. ECG = electrocardiogram. JDD Downloaded From: https://content.onlinejacc.org/ on 10/01/2016 EL·SHERIF ET AL. BURST PACING VERSUS MULTIPLE PREMATURE STIMULATION JACC Vol -i, No.2 August 19l4:295-304 299 ECG'--'I--..rI 500 MS oLLUWJJJ----------. Figure 4. Epicardial isochronal maps of S, to S10 during a 10 beat run of burst pacing that induced a reentrant rhythm from the same experiment shown in Figures I to 3. The S I to S4 maps were similar to those in Figure 3. Reentrant activation initiated by S4 continued during S, with limited contribution from the paced wave front. S6 interrupted reentrant activation, while S7 to SIO resulted in a new sequence of ventricular activation patternsof paced beats characterized by progressively longer arcs of conduction block and slower wave fronts with StO initiating reentrant activation (represented by the dotted line). See text for details. / arcs of block that coalesced into a single wave front. This single wave front conducted slowly over a circuitous pathway before reactivating myocardial sites on the septal border of the infarct to initiate the second reentrant beat. Figure 3 illustrates epicardial isochronal maps during a four beat run of burst pacing that induced a reentrant tachycardia. The activation maps of Stand S2 were similar to those shown in Figure 2. In this and all other experiments, the activation map of S I did not vary in relation to the preceding cycle (::=: 350 ms) or the origin of the preceding beat (supraventricular or ventricular). The second premature stimulus (53) during burst pacing has a coupling interval of 220 ms compared with a 185 ms coupling interval during premature stimulation. It resulted in a shorter arc of conduction block and less conduction delay of the common reentrant wave front. The latter reached the distal side of the arc of block 180 ms from the onset of right ventricular activation compared with 200 ms during the second premature stimulus (S3) in Figure 2. This probably did not Downloaded From: https://content.onlinejacc.org/ on 10/01/2016 provide sufficient time for refractoriness of myocardial zones on the proximal side of the arc of block to expire and explains why a three beat run of burst pacing failed to initiate reentry. In contrast, S4 resulted in more extensive conduction block and a slower wave front that succeeded in reexciting myocardium on the proximal side of the arc of block thus initiating the first reentrant beat (V I). The activation maps of V I and V2 were approximately similar to the V I map shown in Figure 2. Specifically, the upper circulating wave front advanced around a circular zone of functional block that changed its position from beat to beat during the reentrant tachycardia. Figure 4 illustrates the epicardial maps of55to 5 10 during a 10 beat paced run that induced a reentrant rhythm. The S I to S4 maps were similar to the ones shown in Figure 3. The 55 map was remarkably similar to that of V I in Figure 3. This, in addition to the fact that a five beat paced run could also induce a reentrant rhythm, strongly suggests that circus movement reentry continued during S5' How- 300 EL-SHERIF ET AL. BURST PACING VERSUS MULTIPLE PREMATURE STIMULATION ever, the pacing stimulus did result in activation of part of the right ventricular epicardium, although the line of fusion between the paced and reentrant wave fronts could not be determined precisely. On the other hand, the epicardial map of S6 shows that the activation wave front advanced rapidly from the site of right ventricular stimulation to the narrow isthmus of slow conduction on the lateral border of the infarction. During S6, conduction from the site of right ventricular stimulation to the narrow isthmus of slow conduction was 40 to 60 ms compared with 120 to 140 ms between the two sites during reentrant activation. The fast arrival of the paced wave front before expiration of refractoriness of the myocardium at this critical site of the reentrant circuit probably explains conduction block of the wave front at this site. The S6 map also shows that the circulating wave front during S5 succeeded in reexciting a localized myocardial zone at the septal border of infarction. Thus, the most plausible explanation of the S6 map is that the paced wave front resulted in containment of reentrant activation into a small part of the paraseptal myocardium while at the same time it advanced rapidly to the area of previous slow conduction resulting in conduction block and termination of reentrant activation. The relatively fast arrival of the paced wave front could be explained by conduction in myocardial zones that were enclosed within the upper island of functional conduction block and, therefore, were not activated during S5' The S7 map showed an activation pattern very similar to that of SI in Figure 3 (that is, fast conduction with the entire epicardial surface being activated within 80 ms). The S8, S9 and SIO maps were also, respectively, similar to the S2, S3 and S4 maps in Figure 3. Thus, termination of a 10 beat Figure S. Electrocardiographic recordings from experiment 5 in which three premature stimuli (S,S2S3S4) were required to initiate a reentrant rhythm. See text for details. lACC Vol. 4, No.2 August 1984:295-304 paced run resulted in a reentrant rhythm, as did termination of a 4 beat paced run. The S 11 and S'2 maps were to some extent similar to the S6 and S7 maps in Figure 4, and II or 12 beat paced runs did not initiate a reentrant rhythm. Pleomorphic ventricular rhythms. Electrocardiograms. Figure 5 illustrates electrocardiographic recordings from experiment 5 in which three premature stimuli were required to initiate reentry. SISt cycle length was 400 ms and S2, 53 and S4premature stimuli were introduced at cycle lengths of 200, 180 and 165 ms, respectively. SIS2S354 stimulation resulted in three reentrant beats with a negative QRS configuration in lead II. Figure 6 shows electrocardiographic recordings obtained from the same experiment and illustrates the results of burst pacing at a cycle length of 200 ms. Only four, eight and nine beat paced runs could initiate a reentrant rhythm. A four beat paced run induced four reentrant beats with pleomorphic configuration. The first reentrant beat had a narrow predominantly positive QRS configuration, while the remaining three beats had a negative QRS configuration. An eight beat paced run only intermittently resulted in a single reentrant beat with a negative QRS configuration. Similarly, a nine beat paced run could oc- Figure 6. Electrocardiographic recordings from the same experiment shown in Figure 5, illustrating the results of 3 to 12 beat runs of burst pacing (BP). Only four, eight and nine beat paced runs could initiate one or more reentrant beats (the first reentrant beat is marked by an asterisk). The tracing on the bottom of each electrocardiographic recording denotes the timing of stimulation. See text for details. BP BP 3~8~ ~ ~ 4~9~ 4-L9~ ~ ~ 5 ~ ~ 6~10~ ~ ~ 7~11.J8Wv ~ ~ 8 I 1SEC Downloaded From: https://content.onlinejacc.org/ on 10/01/2016 ~ 12~AMMij\~ EL-SHERIF ET AL. BURST PACING VERSUS MULTIPLE PREMATURE STIMULATION JACC Vol 4, No, 2 August 19~4:295-304 casionally result in a single reentrant beat with prolonged coupling and a positive QR5 configuration. Epicardial isochronal maps. Figure 7 illustrates the epicardial maps during a four beat paced run that initiated a pleomorphic reentrant rhythm. The entire epicardial surface was activated within 80 ms during S I, with the central part of the epicardial surface of the infarction being the last to be activated; 52 resulted in a relatively short arc offunctional conduction block and a limited degree of slow conduction (last isochrone at 120 ms). 53 and 54 resulted in progressively longer arcs of conduction block and slower conduction, During S4, the slow common reentrant wave front reached a site on the distal border of the septal arc of block at the 200 ms isochrone and succeeded in reexciting myo- cardial zones on the septal border of the infarction to initiate reentry. The septal breakthrough resulted in a predominantly basal to apical activation of the left ventricle during V I and may explain the narrow positive QR5 configuration in lead II. Ventricular activation continued during VI in the form of two circulating wave fronts that coalesced and conducted slowly toward the apex before reexciting apical zones to initiate the second reentrant beat (V 2). The predominantly apical to basal ventricular activation during V2 explains the negative QR5 complex in lead II. Figure 8 illustrates the epicardial maps of S4 to Sg during an eight beat paced run that initiated a single reentrant beat (VI) with a negative QRS complex. Similar to what was described in Figure 4, 55 initiated an activation wave 20 60 Figure 7. Epicardial isochronal maps during a four beat burst pacing run that initiated a pleomorphic reentrant rhythm from the same experiment shown in Figures 5 and 6. See text for details. ECG = electrocardiogram. 240 Downloaded From: https://content.onlinejacc.org/ on 10/01/2016 301 302 EL-SHERIF ET AL. BURST PACING VERSUS MULTIPLE PREMATURESTIMULATION lACC Vol. 4, No.2 August 1984:295-304 ECG~ -------, Figure 8. Epicardial isochronal maps of S4 to S8 during an eight beat burst pacing run that initiated a single reentrant beat (VI) from the same experimentshown in Figures 5 to 7. The SI to S4 maps were similarto thosein Figure7. S5 interrupted the reentrant activation that was initiated by S4. Subsequently, S6 to S8 showedprogressively longerarcsof conduction block and slowerwave fronts, with S8 initiating a single reentrant beat. See text for details. ECG = electrocardiogram, Sa front that advanced rapidly through myocardial zones that were not excited during 54' As a consequence, the wave front reached the areas of slow conduction at the apex and the central part of the infarct before expiration of their refractoriness, resulting in conduction block and the termination of the reentrant process. The paced activation front also resulted in containment of the reentrant wave front induced by 54 into a small localized zone on the septal border of the infarction. 56, S7 and S8 initiated a new series of sequential activation patterns showing progressively longer arcs of conduction block and slower conduction. During S8, the last isochrone at 200 ms could intermittently succeed in reexciting apical myocardium to initiate a single reentrant beat with a negative QRS configuration (VI)' During Vb the two circulating wave fronts failed to conduct in the Downloaded From: https://content.onlinejacc.org/ on 10/01/2016 central part of the epicardial surface of the infarct, resulting in termination of the reentrant process. Ventricular activation during rapid ventricular pacing at long cycle lengths. Patterns of ventricular activation during rapid ventricular pacing at cycle lengths longer than the SISz coupling interval were analyzed in three experiments. In each experiment, sequential paced beats showed similar ventricular activation patterns with relatively rapid conduction and no arcs of functional conduction block up to a critical short pacing cycle length. At shorter cycle lengths, sequential beats showed progressively longer arcs of functional block and slower conduction. For example, in the experiment in Figures I to 4, sequential ventricular paced beats at cycle lengths longer than 240 ms showed similar ventricular activation patterns with relatively fast conduction EL-SHERIF ET AL. BURST PACING VERSUS MULTIPLE PREMATURE STIMULATION lACC Vol. 4, No.2 August 1 9 ~4 : 295-304 and no arcs of conduction block . However , during pacing at a cycle length of 240 ms, functional conduction block and slow conduction began to develop and increased in magnitude in sequential beats . A five beat paced run was required before sufficient conduction delay developed so that the slow wave front could reexcite myocardial zones on the proximal side of the arc to block and initiate reentrant activation. In contrast, a four beat paced run was only required when pacing was applied at 220 ms. The range of cycle lengths during which paced runs could initiate reentry in the same experiment varied from 10 to 30 ms. Discussion Our report includes only experiments in which reentry was induced by more than one premature stimulus. In experiments in which a reentrant rhythm could be induced by a single premature stimulus, burst pacing could also initiate reentry and the e1ectrophysiologic mechanism is essentially similar to the one described in this study. Those experiments were not included , however , because of their limited clinical relevance . Usually in a clinical setting, burst pacing is not utilized when arrhythmias can be induced by a single premature stimulus . Mechanism of induction of reentrant rhythms byburst pacing. The mechanism by which burst pacing could initiate reentry was suggested from earlier studies (3) that utilized composite electrode recordings. However , detailed analysis of ventricular activation pattems of successive paced beats was necessary for a more thorough elucidation of the mechanism. In the present study , successive paced beats applied at a critically short cycle length resulted in progressively longer arcs of functional conduction block or slower circulating wave fronts, or both. The slow wave front reaching the distal side of the arc of block after a critical degree of conduction delay could reexcite myocardial zones on the proximal side of the arc after expiration of their refractoriness to initiate circus movement reentry. However. for manifest reentry to take place , the paced run should be terminated after the beat that resulted in a critical degree of conduction delay. If rapid pacing was extended past this beat , reentrant activation could be confined (concealed) to a zone of early reexcitation or a varying degree of fusion between the reentrant and paced wave fronts, or both, could occur . Furthermore , a paced wave front could advance rapidly to the critical zone of slow conduction of the reentrant circuit before expiration of its refractoriness. This would result in conduction block and interruption of circulating excitation. Termination of a paced run after this beat would not result in reentrant activation . In our study . the earlier arriva l of the paced wave front could be attributed, at least in part. to activation of myocardial zones that were not stimulated during the preceding beat and thereby had recovered full excitability. However , because this was asso- Downloaded From: https://content.onlinejacc.org/ on 10/01/2016 303 ciated with a change of the pathway of the paced wave front the role of a " faster" rate of conduction of the wave front in certain myocardial zones could not be precisely determined . When the paced run was continued past the beat that interrupted reentry , a new sequence of ventricular activation patterns of paced beats characterized by progressively longer arcs of conduction block or slower wave fronts, or both, developed . Once again , manifest reentry could only develop if the paced run was terminated after the beat that resulted in a critical degree of conduction delay. It should be emphasized that the rules for initiation of reentrant rhythms by burst pacing are the same whether the resulting rhythm is a monomorphic tachycardia or a nonsustained pleomorphic rhythm. Our study has shown that the mechanism of induction of reentry by a series of paced beats at a critically short cycle length is essentially similar to that of multiple premature stimulation. A minor difference was that multiple premature stimuli were introduced at gradually shorter cycle lengths compared with the constant cycle length during burst pacing. This resulted in a more prompt development of the necessary prerequisites of reentry in terms of zones of functional conduction block and slow circulating wave fronts . Thus, in the experiments shown in Figures I to 4, two premature stimuli at a cycle length of 220 and 185 ms, respectivel y, could initiate reentry , while a series of three short cycles at 220 ms during a four beat paced run was required to do the same. Clinical implications. The present study was only designed to analyze the mechanism of induction of reentry by burst pacing and to compare this with multiple premature stimulation. It does not address other issues that may be relevant in the clinical setting . One such issue is the clinical significance of reentrant rhythms induced by more aggressive stimulation protocols, such as triple premature stimuli and burst pacing particularly in the absence of a spontaneous clinical arrhythmia. However, this study may provide useful guideline s regarding the use of burst pacing to initiate reentrant rhythms in the clinical laboratory . In our experiments, multiple premature stimuli and burst pacing were equally successful in inducing reentry . However, because burst pacing was critically dependent on the number of beats in the paced run , the majority of paced runs applied in a single experiment failed to initiate reentry and only a few did. The critical number of beats in runs of burst pacing that can initiate reentry is difficult to standardize and varies in different experiments as well as with the cycle length of pacing in the same experiment. This is not the case with programmed multiple premature stimulation . Therefore, within accepted limits of extrapolating experimental observations to the clinical setting, our study suggests that random burst pacing as a technique of induction of reentrant rhythms should be abandoned in favor of multiple premature stimulation. 304 EL-SHERIF ET AL. BURST PACING VERSUS MULTIPLE PREMATURE STlMULATIO/\ We thank Gerald Cohen and his staff for technical assistance, Ann Basile aIId Barbara Grebin for the preparation of the manuscript and Mike Yu for the art work. lACC Vol. 4. No.2 August 1984:295· 304 the heart in patients with ventricular tachycardia. Circulation 1972;46:216--26. I. MendezC, Moe GK. Demonstration of a dual A-V conductionsystem in the isolated rabbit heart. Circ Res 1966;19:378-92. 7. El-Sherif N, Mehra R, Gough WB. Zeiler RH. Ventricularactivation patternof spontaneousand induced ventricular rhythms in canine oneday-old myocardial infarction. Evidencefor focal and reentrant mechanisms. Circ Res 1982;51: 152-66. 8. Mehra R, Zeiler RH, Gough WB, EI-Sherif N. Reentrant ventricular arrhythmias in the late myocardial infarction period. 9. Electrophysiologic-anatomic correlation of reentrant circuits. Circulation 1983;67: 11-24. 2. Wit AL, Cranefield PF, Hoffman BF. Slow conduction and reentry in the ventricular conducting system. I. Return extrasystole in canine Purkinje fibers. Circ Res 1972;30:1-10. 9. EI-SherifN. Mehra R, Gough WB, Zeiler RH. Reentrant ventricular arrhythmias in the late myocardial infarction period. Interruption of reentrant circuit by cryothermal techniques. Circulation 1983;68:644-50. 3. EI-SherifN, Hope RR, Scherlag BJ, Lazzara R. Reentrantventricular arrhythmias in the late myocardial infarction period. 2. Patterns of initiation and termination of re-entry. Circulation 1977;55:702-17. 10. Fisher 10, Cohen HL, Mehra R, Altschur H. Escher DJW, furman S. Cardiac pacing and pacemakers. II. Serial electrophysiologicpharmacologic testing for control of recurrent tachyarrhythmias, Am Heart J 1977;93:658-68. References 4. Durrer D, Schuo L, Schuilenburg RM, Wellens H11. The role of premature beats in the initiation and termination of supraventricular tachycardia in the Wolff-Parkinson-White syndrome. Circulation 1967;36:644-62. 5. Coumel PL, Cabrol C, Fabiato A, Gouryon R, Slama R. Tachycardie permanente par rhythme reciproque. Arch Mal Coeur 1967;60: 1830-42. 6. Wellens H11, Schuilenburg RM, Durrer D. Electrical stimulation of Downloaded From: https://content.onlinejacc.org/ on 10/01/2016 II. Wellens HJJ. Value and limitations of programmed electrical stimulation of the heart in the study and treatment of tachycardias. Circulation 1978;57:845-53. 12. EI-Sherif N, Scherlag BJ, Lazzara R. Reentrant ventricular arrhythmias in the late myocardial infarction period. I. Conduction characteristics in the infarction zone. Circulation 1977;55:686--701.