Mechanical Stresses, Arterial Stiffness, and Brain
Small Vessel Diseases
Shimanami Health Promoting Program Study
Yoko Okada, MD; Katsuhiko Kohara, MD; Masayuki Ochi, MD; Tokihisa Nagai, MD;
Yasuharu Tabara, PhD; Michiya Igase, MD; Tetsuro Miki, MD
Downloaded from http://stroke.ahajournals.org/ by guest on September 30, 2016
Background and Purpose—Arterial stiffness, a risk factor of brain small vessel diseases (SVD), causes hemodynamic
changes. Mechanical stresses, circumferential wall tension (WT), and shear stress (SS) may change with arterial stiffness
and be related to SVD. We investigated the associations between mechanical stresses and arterial stiffness and SVD.
Methods—A total of 1296 subjects without apparent cardiovascular diseases were recruited. Brachial-to-ankle pulse wave
velocity (baPWV) was measured as an arterial stiffness index. Silent lacunar infarction and deep subcortical white
matter hyperintensity were evaluated as SVD indices. Circumferential WT and SS at peak systole and end diastole were
measured at the common carotid artery. Second peak of systolic blood pressure was obtained from the radial waveform
and used as a central systolic blood pressure substitute.
Results—baPWV was associated positively with WT (P<0.0001) and negatively with SS (P=0.0007) even after correction
for confounding parameters including baPWV. SVD was associated with significantly higher WT (P<0.0001) and lower
SS (P<0.0001). After adjustment for confounding parameters (including baPWV), second peak of systolic blood pressure
WT (odds ratio, 1.30; P=0.0017) and end diastolic WT (odds ratio, 1.60; P=0.0038) were related to presence of silent
lacunar infarction, whereas peak systolic (odds ratio, 0.95; P=0.014) and end diastolic SS (odds ratio, 0.94; P=0.014)
were associated with presence of deep subcortical white matter hyperintensity grade >3. Regression lines between blood
pressure and WT were significantly steeper in subjects with SVD than without SVD (β=0.02; P<0.0001).
Conclusions—These findings indicate that SVD is phenotype-specifically associated with alterations in WT and SS
independently of arterial stiffness. (Stroke. 2014;45:3287-3292.)
Key Words: brain small vessel disease ◼ carotid artery ◼ mechanical stress ◼ vascular stiffness
B
rain small vessel disease (SVD) is becoming of increasing clinical interest owing to its associations with stroke
and risk for cognitive decline.1,2 Arterial stiffness is considered an underlying mechanism for SVD.3–7 For example, it
was hypothesized that attenuation of arterial buffering properties results in persistent pulsatility flow and pressure in the
cerebral arterioles, leading to small vessel injury.8 In support,
pulse wave velocity (PWV), an index for arterial stiffness,
has been shown to be significantly associated with SVDs.3–7
Arterial stiffness also causes other hemodynamic changes,
including blood pressure (BP) and blood flow.9 At the same
time, aortic stiffness also affects central BP.
Although diastolic BP is nearly identical throughout the
arterial tree, systolic BP (SBP) differs between peripheral and
central locations because of the phenomenon of pulse pressure
amplification,10 where the brachial and radial SBP are higher
than concurrently measured central aortic SBP. This pulse
pressure amplification is influenced by arterial stiffness and
augmentation by the reflected pressure wave. Early return of
the reflected wave, which is observed in aged and stiffer arteries, can augment aortic SBP, whereas delayed return, which is
observed in young and elastic arteries, does not.9,10 As a result,
central SBP and pulse pressure is relatively higher in stiffer
arteries compared with peripheral BP. Central BP is known to
be more closely associated with end-organ damage and cardiovascular events compared with peripheral BP.10,11 However,
to our knowledge, the local mechanical forces based on central BP have not been evaluated.
Local mechanical stress is also involved in the development
of atherosclerosis.12,13 Circumferential wall tension (WT) and
longitudinal shear stress (SS) are major mechanical stresses
and cause acute and chronic changes in arterial function and
structure.12–15 In the carotid artery, higher WT and lower SS
are associated with carotid arterial remodeling.16,17 WT was
suggested to cause stretching of the arterial wall resulting in
arterial hypertrophy, whereas reduced SS causes endothelial
Received July 23, 2014; accepted August 26, 2014.
From the Department of Geriatrics and Neurology, Ehime University Graduate School of Medicine, Toon-City, Ehime, Japan (Y.O., K.K., M.O., T.N.,
M.I., T.M.); and Department of Medical Genetics, Kyoto University Graduate School of Medicine, Kyoto, Japan (Y.T.).
The online-only Data Supplement is available with this article at http://stroke.ahajournals.org/lookup/suppl/doi:10.1161/STROKEAHA.114.
006539/-/DC1.
Correspondence to Katsuhiko Kohara, MD, Department of Geriatrics and Neurology, Ehime University Graduate School of Medicine, Shitsukawa, ToonCity, Ehime 791-0295, Japan. E-mail koharak@m.ehime-u.ac.jp
© 2014 American Heart Association, Inc.
Stroke is available at http://stroke.ahajournals.org
DOI: 10.1161/STROKEAHA.114.006539
3287
3288 Stroke November 2014
dysfunction leading to atherosclerosis.12,15 However, studies
evaluating potential alterations of mechanical stresses related
to arterial stiffness are limited.
In this context, we hypothesized that local mechanical
stresses are associated with arterial stiffness and contribute to
the development of arterial remodeling. Thus, we evaluated
the relationship between PWV and local mechanical stresses
in 1296 subjects. WT and SS were compared in subjects with
and without SVD. We evaluated 2 forms of manifestations
of SVD: silent lacunar infarction (SLI) and deep subcortical
white matter hyperintensity (DSWMH). Peak systolic WT
was obtained with central SBP as well as brachial SBP to
determine whether the index with central BP was superior to
that obtained with peripheral BP.
Methods
Downloaded from http://stroke.ahajournals.org/ by guest on September 30, 2016
Subjects
Subjects were middle-aged to elderly persons recruited from consecutive visitors to the Anti-Aging Center at Ehime University Hospital
between March 2006 and October 2011. The subjects attended a voluntary medical check-up program, Anti-Aging Doc, a program provided to residents of Ehime Prefecture, Japan, specifically designed
to evaluate aging-related disorders, including atherosclerosis, cardiovascular disease, physical function, and cognitive impairment.6,18–21
Of the 1526 consecutive patients initially approached, 1296 (mean
age, 65.4±9.1 years) gave written consent to all procedures and had
no history of symptomatic cardiovascular events including peripheral
arterial disease, stroke, coronary heart disease, or congestive heart
failure. All participants were functionally independent in their daily
lives. The series of studies to which the present study belongs is in
accordance with the Helsinki Declaration and were approved by the
Ethics Committee of Ehime University Graduate School of Medicine.
device was programmed to automatically determine the pressure
against the radial artery to obtain the optimal arterial waveform. Second
peak of SBP (SBP2) was calculated by calibration with the brachial
SBP. The measurements were repeated twice and the mean values were
obtained. SBP2 has been shown to accurately reflect transfer function–
derived aortic SBP and was used as central SBP substitute.6,24,25
Echo-Doppler Examination of the Carotid Arteries
Carotid arteries were evaluated using an SSD-3500SV (Aloka Co,
Ltd, Tokyo, Japan) with a 7.5-MHz probe equipped with a continuous-flow Doppler and phase-locked echo-tracking system. Internal
diameters of the common carotid artery at end-diastole (Dd) and peaksystole (Ds) were measured.16 Doppler evaluation was performed on
the bilateral common carotid arteries at 1 cm proximal to the bulb
and, if an abnormality including a plaque was present, upstream of
the abnormality. Peak systolic flow velocity (Vs) and end-diastolic
flow velocity (Ved) were obtained.
Determination of Mechanical Stresses
Wall Tension
WT was determined by Laplace low with the following equations.16,26,27 End diastolic WT=diastolic BP×Dd/2. Peak systolic
WT=SBP×Ds/2. Peak SBP2 WT=SBP2×Ds/2.
Shear Stress
The viscosity at shear rates of 104 and 52 per second was obtained by
the following equation.28,29 Whole blood viscosity (104 per second)
=(0.12*Ht)+(0.19*TP)−2.13 (cP). Whole blood viscosity (52 per se
cond)=(0.14*Ht)+(0.22*TP)−2.60 (cP), where Ht is hematocrit (in
%) and TP is plasma protein concentration (in g/dL). The regression
SVDs on Brain MRI Examination
Brain MRI was performed with a 3-T scanner (Sigma Excite 3.0T;
GE Healthcare, Milwaukee, WI). As a manifestation of SVD, SLI and
DSWMH were evaluated in each subject. SLI was defined as areas of
low signal intensity (3–15 mm diameter) on T1-weighted and fluidattenuated inversion recovery images and of high intensity on T2weighted images. DSWMH was graded into 5 grades in accordance
with Japanese guidelines.22 Images were analyzed by 2 neurologists
without clinical information on the subject.6,19 SVD was defined as
the presence of SLI and the presence of DSWMH grade ≥3.
Pulse Wave Velocity
PWV was measured using a volume-plethysmograph (PWV/ankle
brachial index; Omron Healthcare Co, Ltd, Kyoto, Japan). A detailed
explanation of this device as well as the validity and reproducibility
of its measurements have been provided elsewhere.23 Brachial-to-ankle
PWV (baPWV) was calculated from the time interval between the wave
fronts of the brachial and ankle waveforms (ΔTba) and the path length
from the brachium to the ankle. Path length from the suprasternal notch
to the brachium (Lb) or ankle (La) was obtained using the following
formulae: Lb=0.2195×height+2.0734; La=0.8129×height+12.328.
baPWV was then obtained using the equation (La−Lb)/ΔTba. The
intrameasurement reproducibility of baPWV in our laboratory was
2.1±1.8%, and between measurements it was 2.2±1.5%.21
Radial Waveform Analysis and BP Measurement
Radial waveform was analyzed in the left radial artery using an automated tonometric method (HEM-9000AI; Omron Healthcare Co, Ltd),
with subjects in the sitting position after ≤5 minutes of rest. Brachial
BP was measured simultaneously in the right brachium with an oscillometric device incorporated into the HEM-9000AI. The HEM-9000AI
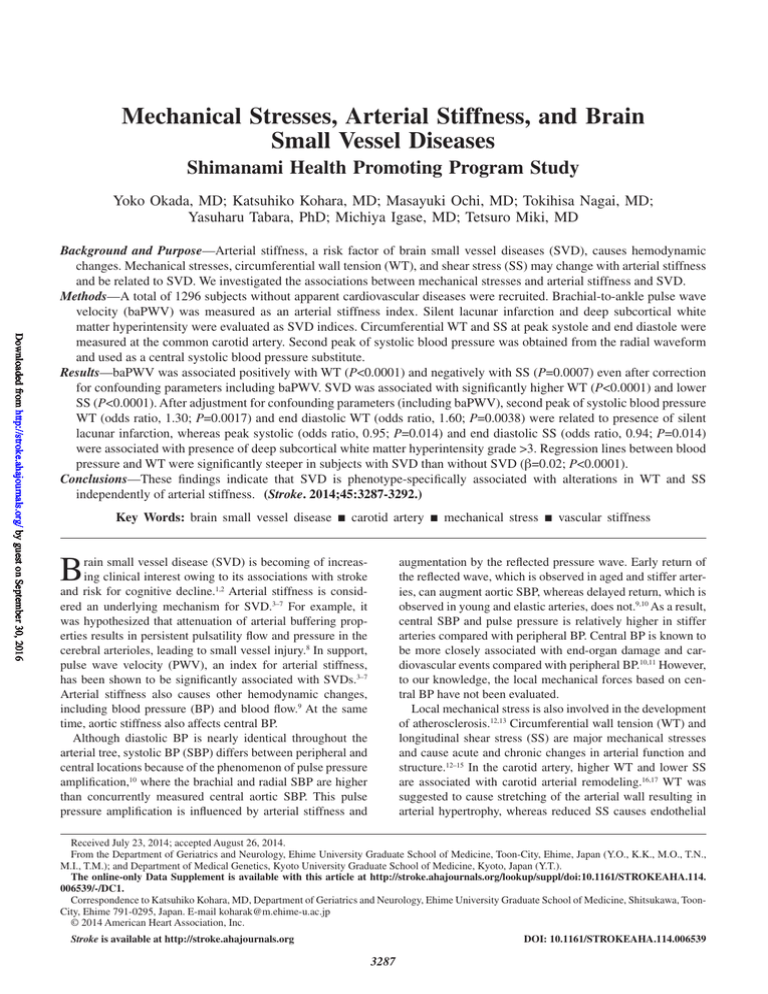
Figure 1. Scatter plots between brachial-to-ankle pulse wave
velocity (baPWV) and peak systolic wall tension (WT), second
peak of systolic blood pressure WT, end diastolic WT, peak systolic shear stress (SS), and end-diastolic SS. All associations are
statistically significant. n=1294 in associations between baPWV
and WT, and n=1197 in associations between baPWV and SS.
Okada et al Mechanical Stress and Small Vessel Diseases 3289
between shear rate and viscosity was determined for each subject,
because blood viscosity was shown to be linearly related to shear rate.
The viscosity in situ, at both peak systolic shear rate and end diastolic
shear rate, was calculated from the regression line between shear rate
and viscosity for each subject.
In vivo wall shear rates were calculated with the use of a Poiseuillean
parabolic model of velocity distribution across the arterial lumen
based on the assumption of laminar blood flow, according to the following formula: shear rate (γ)=4×blood flow velocity in center/carotid
arterial diameter.16,26 SS values were determined by multiplying the
shear rate and viscosity, with the assumption that blood is a Newtonian
fluid. Peak systolic SS and end-diastolic SS were obtained.16,26
Evaluation of Risk Factors
Lifestyle, medical history, and prescribed drugs were evaluated by questionnaire. Anthropometric measurements were performed by a trained
nurse. Venous blood was collected in the morning after >11 hours fasting for measurement of serum lipid and plasma glucose concentrations.
Downloaded from http://stroke.ahajournals.org/ by guest on September 30, 2016
Statistical Analysis
Values are expressed as mean±SD unless otherwise specified. First, we
examined for an association between baPWV and WT and SS. Further
multiple regression analyses were performed to ascertain whether WT
and SS were associated with baPWV independently of other possible
confounding parameters. Second, subjects were categorized based on
the presence or absence of SLI and the grade of DSWMH, grade 0 to
1, grade 2 and grade ≥3. Clinical background and mechanical stresses–
related parameters were compared among the SVD groups. Logistic
regression analyses were performed to evaluate whether mechanical
stresses were associated with the presence of SVD independently of
confounding parameters including baPWV. Last, regression lines between BP and mechanical stresses were compared in subjects with
and without SVD. Interactions between BP and the presence of SVD
on mechanical stresses were evaluated. Differences in numeric variables between groups were assessed using ANOVA testing followed
by Tukey correction for multiple comparisons, whereas differences in
frequency were assessed using the χ2 test. Corrections for confounding
parameters were made using these parameters in multiple regression
analyses. All analyses were performed using commercially available
statistics software (JMP version 10.0; SAS Institute, Cary, NC), with
P<0.05 considered statistically significant.
Results
Association Between baPWV and Mechanical
Stresses
The relationships between baPWV and carotid mechanical
stresses in the total population are summarized in Figure 1.
Even after adjustment for possible confounding parameters
including BP, WTs showed positive and SSs showed negative associations with baPWV (Table I in the online-only Data
Supplement).
Clinical Characteristics of Subjects With
Brain SVDs
Clinical characteristics of subjects with and without SVD are
summarized in Table II in the online-only Data Supplement.
SLI was observed in 13% and DSWMH grade ≥3 in 8% of
Figure 2. Mechanical stresses in subjects
with and without silent lacunar infarction
(SLI) and in subjects divided into 3 groups
based on the severity of deep subcortical white matter hyperintensity (DSWMH).
Peak systolic wall tension, second peak
of systolic blood pressure (SBP2) wall
tension, end-diastolic wall tension, peak
systolic shear stress, and end-diastolic
shear stress are illustrated. All mechanical
stresses are statistically different among
groups of small vessel diseases. Number
in the column indicates number of subjects.
3290 Stroke November 2014
the studied population. Parameters related to mechanical
forces with and without SVD are summarized in Table III in
the online-only Data Supplement. SVD was associated with
carotid dilatation and low flow velocity, whereas viscosity was
only related to DSWMH.
Mechanical Forces in Subjects With Brain SVDs
Mechanical stresses in subjects with and without SVD are
summarized in Figure 2. Both SLI and DSWMH showed significantly higher WT. By contrast, SVD was associated with
significantly lower SS in both peak systole and end-diastole
(Figure 2).
Logistic Regression Analyses for Brain SVDs
Downloaded from http://stroke.ahajournals.org/ by guest on September 30, 2016
Independent association of mechanical stresses with the presence of SVD was further analyzed by logistic regression
analyses (Table). After adjustment for all possible confounding parameters, peak SBP2 WT and end-diastolic WT, but not
peak systolic WT, were independently and significantly associated with the presence of SLI, whereas SS was associated
with the presence of DSWMH grade ≥3.
Interaction Between BP and Brain SVDs on
Mechanical Forces
We further compared the relationship between BP and
mechanical stresses between the presence and absence of
SVD. In a multiple regression analyses including all confounding parameters and interaction between SBP2 and the
presence of SVD, the SBP2-related increase in WT was significantly higher in subjects with SVD (Figure 3; Table IV
in the online-only Data Supplement). Similar findings were
also observed in SBP and diastolic BP (Tables V and VI in the
online-only Data Supplement).
Discussion
In the present study, we found that baPWV was significantly
and positively associated with circumferential WT and negatively related to SS. Two forms of manifestation of brain SVD,
Table. SLI and DSWMH, were associated with alteration of WT and
SS. After adjustment for all possible confounding parameters,
wall stresses were independently associated with SLI, whereas
SS was a significant determinant of the presence of DSWMH
grade ≥3. Regression lines between BP and WT were significantly steeper in subjects with SVD, indicating that the effect
of BP on mechanical forces was more potent in subjects with
SVD. To our knowledge, this is the first report of an association between mechanical stresses and arterial stiffness and
SVD in a large general population.
Close associations between higher PWV and brain SVD
have been reported in many cross-sectional and longitudinal studies,4–7 indicating a causal role of arterial stiffness in
development of SVD.4 In the present study, we investigated
a possible association between local mechanical stresses and
arterial stiffness, because these stresses also play pivotal roles
in the development of atherosclerosis.
WT is increased by elevation of BP and arterial dilatation
and is reduced by arterial wall thickening.12,13 SS is increased
by elevation of blood flow and blood viscosity, but decreased
by arterial dilatation.12 In general, high SS causes vessel dilatation and atheroprotection through endothelial stimulation. In
the chronic phase, an alteration in mechanical stresses causes
arterial remodeling.12
In association with an elevation of PWV, blood flow and BP
increase during systole and decrease during diastole. Because
higher WT and lower SS are assumed to be atherogenic,12–17
peak systolic WT and end-diastolic SS may underlie the association between baPWV and atherosclerosis. In fact, in the
present study, simple correlation coefficients with baPWV
were significantly higher for systolic WT (r=0.58 for SBP;
r=0.55 for SBP2) than for diastolic WT (r=0.43; P<0.0001).
By contrast, SS was more strongly associated with baPWV
at end-diastole (r=−0.36) than at peak systole (r=−0.25)
(P<0.01). These findings indicate that hemodynamic changes
related to the development of arterial stiffness deteriorate the
profile of focal mechanical stresses.
In the Prospective Study of Pravastatin in the Elderly at Risk
(PROSPER) study evaluation of SVD and SS in 329 subjects,
Odds Ratio for the Presence of Small Vessel Diseases
DSWMH ≥3
SLI
Model 1
OR (95% CI)
Model 2
P Value
OR (95% CI)
Model 1
P Value
Model 2
OR (95% CI)
P Value
OR (95% CI)
P Value
Peak systolic wall
stress, 104 dyne/cm
1.30 (1.14–1.49)
0.0001
1.20 (0.95–1.53)
0.13
1.31 (1.11–1.54)
0.0015
1.21 (0.99–1.46)
0.058
Peak SBP2 wall stress,
104 dyne/cm
1.32 (1.16–1.51)
<0.0001
1.30 (1.03–1.65)
0.026
1.30 (1.11–1.53)
0.0017
1.22 (1.01–1.46)
0.041
End-diastolic wall
stress, 104 dyne/cm
1.88 (1.46–2.43)
<0.0001
1.70 (1.22–2.37)
0.0017
1.60 (1.17–2.19)
0.0038
1.42 (0.99–2.04)
0.055
Peak systolic shear
stress, dyne/cm2
0.98 (0.95–1.01)
0.29
1.00 (0.97–1.03)
0.95
0.94 (0.90–0.98)
0.0022
0.95 (0.91–0.99)
0.014
End-diastolic shear
stress, dyne/cm2
0.96 (0.89–1.04)
0.31
1.01 (0.93–1.10)
0.77
0.85 (0.76–0.94)
0.0024
0.88 (0.78–0.98)
0.023
Model 1: no correction; model 2: corrected for age, sex, body mass index, total cholesterol, high-density lipoprotein cholesterol, triglyceride, glucose, immunoreactive
insulin, brachial-to-ankle pulse wave velocity, use of antihypertensive drugs, antidyslipidemic drugs, antidiabetic drugs, and current smoking. n=1294 for wall stresses.
n=1197 for shear stress. CI indicates confidence interval; DSWMH, deep subcortical white matter hyperintensity; OR, odds ratio; SBP2, second peak of systolic blood
pressure; and SLI, silent lacunar infarction.
Okada et al Mechanical Stress and Small Vessel Diseases 3291
Downloaded from http://stroke.ahajournals.org/ by guest on September 30, 2016
Figure 3. Interaction between second peak of systolic blood
pressure (SBP2) and the presence of silent lacunar infarction
(SLI) on peak SBP2 wall tension. Dark dots indicate subjects
with SLI. Light dots indicate subjects without SLI. Solid and dotted lines indicate regression line between SBP2 and peak SBP2
wall tension in subjects with and without SLI, respectively. The 2
regression lines are significantly different (P<0.0001).
diastolic SS was found to be associated with SVD.30 In the
present study, we extend these findings to show that SVD is
associated with mechanical forces including WT in a larger population. In our population, both WT and SS were significantly
associated with SVD. Interestingly, significant associations persisted after adjustment for confounding parameters including
baPWV, indicating that mechanical forces were related to SVD
independently of arterial stiffness. After correction for confounding parameters, WT was associated with SLI, whereas SS
was associated with DSWMH. Because both SLI and DSWMH
are clinical manifestations of SVD, the cause of the dissociation
between the 2 indices remains unknown. Recently, DSWMH
was reported to be genetically different from SLI,19,31 indicating that these 2 conditions have different pathophysiological
backgrounds. The present findings may support these etiologic
differences between SLI and DSWMH.32,33
Endothelial dysfunction and consequent blood brain barrier injury was suggested to be related to SVD, especially to
white matter hyperintensity34; this mechanism may connect
low SS to white matter hyperintensity. WT affects not only the
endothelium but also the entire vasculature including smooth
muscle cells. In the present study, we evaluated SBP2 WT in
addition to peak systolic WT determined by brachial SBP.
After adjustment for confounding parameters, both SLI and
DSWMH were more closely related with SBP2 WT than peak
systolic WT, indicating that central BP measurement may be
useful for the determination of systolic WT. We also compared
the regression lines between mechanical stresses and BP in
subjects with and without SVD. The interaction between BP
and SVD was statistically significant for WT (Figure 3), indicating that more strict control of BP would be necessary to
normalize WT in subjects with SVD.
Morphological changes such as dolichocarotid have been
shown to be associated with end-organ damage.35,36 It was
reported that peak systolic velocity was not different at the
outlet of the carotid abnormality among kinking, coiling, and
tortuosity,37 and we avoid any morphological abnormality in
measuring flow velocity. However, we could not completely
rule out the possibility that the presence of dolichocarotid
could affect the local hemodynamic alterations, because we
did not evaluate longitudinal carotid arterial morphological
abnormalities.
There are several other limitations of our study. Blood viscosity was not directly measured, but rather obtained with an
approximation formula. However, parameters affecting viscosity (eg, hemoglobin and total protein) were similar among the
SVD groups, and SS was predominantly determined by blood
velocity and carotid dimension, which were directly measured.
The cross-sectional nature of our study did not allow us to determine causality. The mechanisms linking baPWV and mechanical stresses and brain SVD are beyond the scope of the present
study and will be addressed in future longitudinal observations.
In summary, arterial stiffness was associated with alteration of mechanical stresses, high circumferential WT, and low
SS in the carotid artery. These changes in mechanical stresses
were associated with brain SVD, partly independent of arterial
stiffness.
Sources of Funding
This work was supported in part by Grants-in-Aid for Scientific
Research from the Japanese Ministry of Education, Culture, Sports,
Science, and Technology (No. 23390188 and 30260384), and a research fund from the Mitsui Sumitomo Insurance Welfare Foundation
in Japan.
Disclosures
None.
References
1. Conijn MM, Kloppenborg RP, Algra A, Mali WP, Kappelle LJ, Vincken
KL, et al; SMART Study Group. Cerebral small vessel disease and risk
of death, ischemic stroke, and cardiac complications in patients with
atherosclerotic disease: the Second Manifestations of ARTerial diseaseMagnetic Resonance (SMART-MR) study. Stroke. 2011;42:3105–3109.
2.Kalaria RN. Cerebrovascular disease and mechanisms of cognitive
impairment: evidence from clinicopathological studies in humans. Stroke.
2012;43:2526–2534.
3. Singer J, Trollor JN, Baune BT, Sachdev PS, Smith E. Arterial stiffness, the
brain and cognition: a systematic review. Ageing Res Rev. 2014;15:16–27.
4. Rosano C, Watson N, Chang Y, Newman AB, Aizenstein HJ, Du Y, et al.
Aortic pulse wave velocity predicts focal white matter hyperintensities in
a biracial cohort of older adults. Hypertension. 2013;61:160–165.
5. Poels MM, Zaccai K, Verwoert GC, Vernooij MW, Hofman A, van der
Lugt A, et al. Arterial stiffness and cerebral small vessel disease: the
Rotterdam Scan Study. Stroke. 2012;43:2637–2642.
6. Ochi N, Kohara K, Tabara Y, Nagai T, Kido T, Uetani E, et al. Association
of central systolic blood pressure with intracerebral small vessel disease
in Japanese. Am J Hypertens. 2010;23:889–894.
7. Henskens LH, Kroon AA, van Oostenbrugge RJ, Gronenschild EH,
Fuss-Lejeune MM, Hofman PA, et al. Increased aortic pulse wave velocity is associated with silent cerebral small-vessel disease in hypertensive
patients. Hypertension. 2008;52:1120–1126.
8. O’Rourke MF, Safar ME. Relationship between aortic stiffening and
microvascular disease in brain and kidney: cause and logic of therapy.
Hypertension. 2005;46:200–204.
9. Nichols WW, O’Rourke MF, Vlachopoulos C. Contours of pressure and
flow waves in arteries. In: Nichols WW, O’Rourke MF, Vlachopoulos
C, eds. McDonald’s Blood Flow in Arteries. 6th ed. London: Hodder
Arnold; 2011:225–253.
10. Roman MJ, Devereux RB. Association of central and peripheral blood
pressures with intermediate cardiovascular phenotypes. Hypertension.
2014;63:1148–1153.
3292 Stroke November 2014
Downloaded from http://stroke.ahajournals.org/ by guest on September 30, 2016
11.Kohara, K. Central blood pressure and end-organ damage. Curr
Hypertens Rev. 2012;8:100–107.
12. Hoefer IE, den Adel B, Daemen MJ. Biomechanical factors as triggers of
vascular growth. Cardiovasc Res. 2013;99:276–283.
13. Lu D, Kassab GS. Role of shear stress and stretch in vascular mechanobiology. J R Soc Interface. 2011;8:1379–1385.
14. Ando J, Yamamoto K. Flow detection and calcium signalling in vascular
endothelial cells. Cardiovasc Res. 2013;99:260–268.
15. Davies PF. Hemodynamic shear stress and the endothelium in cardiovascular pathophysiology. Nat Clin Pract Cardiovasc Med. 2009;6:16–26.
16.Jiang Y, Kohara K, Hiwada K. Association between risk factors
for atherosclerosis and mechanical forces in carotid artery. Stroke.
2000;31:2319–2324.
17. Irace C, Cortese C, Fiaschi E, Carallo C, Farinaro E, Gnasso A. Wall
shear stress is associated with intima-media thickness and carotid atherosclerosis in subjects at low coronary heart disease risk. Stroke.
2004;35:464–468.
18. Uetani E, Tabara Y, Kawamoto R, Onuma H, Kohara K, Osawa H, et
al. CDH13 genotype-dependent association of high-molecular weight
adiponectin with all-cause mortality: the J-SHIPP study. Diabetes Care.
2014;37:396–401.
19. Tabara Y, Igase M, Okada Y, Nagai T, Uetani E, Kido T, et al. Association
of Chr17q25 with cerebral white matter hyperintensities and cognitive
impairment: the J-SHIPP study. Eur J Neurol. 2013;20:860–862.
20. Kohara K, Ochi M, Tabara Y, Nagai T, Igase M, Miki T. Arterial stiffness in sarcopenic visceral obesity in the elderly: J-SHIPP study. Int J
Cardiol. 2012;158:146–148.
21. Ochi M, Kohara K, Tabara Y, Kido T, Uetani E, Ochi N, et al. Arterial
stiffness is associated with low thigh muscle mass in middle-aged to
elderly men. Atherosclerosis. 2010;212:327–332.
22. A new guideline making committee of a brain dock. Brain MRI examination. In: Japanese Society for Detection of Asymptomatic Brain Disease, ed.
Braindock Guideline 2014 [in Japanese]. 4th ed. Tokyo, Japan: Kyobunsha;
2014:38–47.
23. Tomiyama H, Yamashina A, Arai T, Hirose K, Koji Y, Chikamori T,
et al. Influences of age and gender on results of noninvasive brachialankle pulse wave velocity measurement–a survey of 12517 subjects.
Atherosclerosis. 2003;166:303–309.
24. Kohara K, Tabara Y, Tomita H, Nagai T, Igase M, Miki T. Clinical usefulness of the second peak of radial systolic blood pressure for estimation of
aortic systolic blood pressure. J Hum Hypertens. 2009;23:538–545.
25. Takazawa K, Kobayashi H, Kojima I, Aizawa A, Kinoh M, Sugo Y,
et al. Estimation of central aortic systolic pressure using late systolic
inflection of radial artery pulse and its application to vasodilator therapy.
J Hypertens. 2012;30:908–916.
26. Carallo C, Irace C, Pujia A, De Franceschi MS, Crescenzo A, Motti C, et
al. Evaluation of common carotid hemodynamic forces. Relations with
wall thickening. Hypertension. 1999;34:217–221.
27. Gemignani T, Azevedo RC, Higa CM, Coelho OR, Matos-Souza JR,
Nadruz W Jr. Increased popliteal circumferential wall tension induced by
orthostatic body posture is associated with local atherosclerotic plaques.
Atherosclerosis. 2012;224:118–122.
28. de Simone G, Devereux RB, Chien S, Alderman MH, Atlas SA, Laragh
JH. Relation of blood viscosity to demographic and physiologic variables and to cardiovascular risk factors in apparently normal adults.
Circulation. 1990;81:107–117.
29. Tamariz LJ, Young JH, Pankow JS, Yeh HC, Schmidt MI, Astor B, et
al. Blood viscosity and hematocrit as risk factors for type 2 diabetes
mellitus: the atherosclerosis risk in communities (ARIC) study. Am J
Epidemiol. 2008;168:1153–1160.
30. Mutsaerts HJ, Palm-Meinders IH, de Craen AJ, Reiber JH, Blauw GJ,
van Buchem MA, et al; PROSPER Study Group. Diastolic carotid artery
wall shear stress is associated with cerebral infarcts and periventricular
white matter lesions. Stroke. 2011;42:3497–3501.
31. Adib-Samii P, Rost N, Traylor M, Devan W, Biffi A, Lanfranconi S,
et al; Australian Stroke Genetics Collaborative; Wellcome Trust CaseControl Consortium-2 (WTCCC2); METASTROKE; International
Stroke Genetics Consortium. 17q25 Locus is associated with white matter hyperintensity volume in ischemic stroke, but not with lacunar stroke
status. Stroke. 2013;44:1609–1615.
32. Debette S, Markus HS. The clinical importance of white matter hyperintensities on brain magnetic resonance imaging: systematic review and
meta-analysis. BMJ. 2010;341:c3666.
33. Gouw AA, Seewann A, van der Flier WM, Barkhof F, Rozemuller AM,
Scheltens P, et al. Heterogeneity of small vessel disease: a systematic
review of MRI and histopathology correlations. J Neurol Neurosurg
Psychiatry. 2011;82:126–135.
34. Topakian R, Barrick TR, Howe FA, Markus HS. Blood-brain barrier
permeability is increased in normal-appearing white matter in patients
with lacunar stroke and leucoaraiosis. J Neurol Neurosurg Psychiatry.
2010;81:192–197.
35. Ciccone MM, Sharma R, Scicchitano P, Cortese F, Salermo C, Berchialla
P, et al. Dolichocarotids: echo-color Doppler evaluation and clinical role.
J Atheroscler Thromb. 2014;21:56–63.
36.Ciccone MM, Scicchitano P, Palumbo V, Cortese F, Valecce R,
Dentamaro I, et al. Dolichocarotids and dilated cardiomyopathy: is there
a relationship? Int J Cardiol. 2012;158:123–125.
37. Togay-Işikay C, Kim J, Betterman K, Andrews C, Meads D, Tesh P, et al.
Carotid artery tortuosity, kinking, coiling: stroke risk factor, marker, or
curiosity? Acta Neurol Belg. 2005;105:68–72.
Mechanical Stresses, Arterial Stiffness, and Brain Small Vessel Diseases: Shimanami
Health Promoting Program Study
Yoko Okada, Katsuhiko Kohara, Masayuki Ochi, Tokihisa Nagai, Yasuharu Tabara, Michiya
Igase and Tetsuro Miki
Downloaded from http://stroke.ahajournals.org/ by guest on September 30, 2016
Stroke. 2014;45:3287-3292; originally published online September 16, 2014;
doi: 10.1161/STROKEAHA.114.006539
Stroke is published by the American Heart Association, 7272 Greenville Avenue, Dallas, TX 75231
Copyright © 2014 American Heart Association, Inc. All rights reserved.
Print ISSN: 0039-2499. Online ISSN: 1524-4628
The online version of this article, along with updated information and services, is located on the
World Wide Web at:
http://stroke.ahajournals.org/content/45/11/3287
Data Supplement (unedited) at:
http://stroke.ahajournals.org/content/suppl/2014/09/16/STROKEAHA.114.006539.DC1.html
Permissions: Requests for permissions to reproduce figures, tables, or portions of articles originally published
in Stroke can be obtained via RightsLink, a service of the Copyright Clearance Center, not the Editorial Office.
Once the online version of the published article for which permission is being requested is located, click
Request Permissions in the middle column of the Web page under Services. Further information about this
process is available in the Permissions and Rights Question and Answer document.
Reprints: Information about reprints can be found online at:
http://www.lww.com/reprints
Subscriptions: Information about subscribing to Stroke is online at:
http://stroke.ahajournals.org//subscriptions/
SUPPLEMENTAL MATERIAL
Mechanical stresses, arterial stiffness, and brain small vessel diseases: J-SHIPP study
Yoko Okada, MD, Katsuhiko Kohara, MD, Masayuki Ochi, MD, Tokihisa Nagai, MD,
Yasuharu Tabara, PhD, Michiya Igase, MD, Tetsuro Miki, MD
Supplemental table I. Multiple regression analysis for baPWV.
Parameter
Model 1
beta
p
Sex, female=1
-0.02
Age, years
0.30
2
-0.15
Body mass index, kg/m
Systolic blood pressure, mmHg
0.30
Total cholesterol, mg/dl
-0.02
HDL cholesterol, mg/dl
-0.01
Triglyceride, mg/dl
0.13
Fasting glucose, mg/dl
0.07
Immuno reactive isulin, μg/ml
0.08
Use of antihypertensive drugs, yes=1 -0.05
Anti-dyslipidemic drugs, yes=1
-0.03
Anti-diabetic drugs, yes=1
0.00
Current smoking, yes=1
0.01
peak systolic wall tension, 10 4 dyne/ 0.20
peak SBP2 wall tension, 104 dyne/cm
end diastolic wall tension, 104 dyne/cm
peak systolic shear stress, dyne/cm2
end diastolic shear stress, dyne/cm2
0.34
<.0001
<.0001
<.0001
0.33
0.62
<.0001
0.002
0.0007
0.025
0.21
0.99
0.58
<.0001
Model 2
beta
p
-0.04
0.31
-0.14
0.37
-0.03
-0.01
0.12
0.08
0.08
-0.05
-0.03
0.00
0.01
0.06
<.0001
<.0001
<.0001
0.25
0.60
<.0001
0.001
0.0008
0.015
0.22
0.87
0.72
0.10
0.01
Model 3
beta
p
-0.03
0.32
-0.15
0.37
-0.03
-0.02
0.12
0.07
0.08
-0.05
-0.03
-0.01
0.01
0.25
<.0001
<.0001
<.0001
0.25
0.36
<.0001
0.002
0.001
0.029
0.15
0.70
0.75
0.13
<.0001
Model 4
beta
p
-0.07
0.30
-0.15
0.45
-0.01
-0.03
0.11
0.08
0.09
-0.04
-0.03
-0.01
0.01
0.002
<.0001
<.0001
<.0001
0.56
0.31
<.0001
0.001
0.0002
0.09
0.16
0.83
0.81
-0.07
0.0017
Model 5
beta
p
-0.05
0.28
-0.16
0.45
-0.01
-0.03
0.11
0.08
0.10
-0.04
-0.03
0.00
0.00
0.02
<.0001
<.0001
<.0001
0.54
0.29
<.0001
0.0016
0.0001
0.11
0.17
0.90
0.90
-0.08
0.0007
HDL, high density lipoprotein; SBP2, second peak of systolic blood pressure. Blank indicates parameters not entered into the model.
Supplemental table II. Clinical characteristics studied populaiton devided by the presence of silent lacuar infarct and severity of
deep and subcortical white matter hyperinteisity
Silent lacunar infarct
SLI (-)
SLI (+)
n
Male, n (%)
Age, years
Body height, cm
Body weight, kg
Body mass index, kg/m2
Systolic BP, mmHg
Diastolic BP, mmHg
Systolic BP2, mmHg
Heart rate, beats/min
Total cholesterol, mg/dl
HDL cholesterol, mg/dl
Triglyceride, mg/dl
Fasting glucose, mg/dl
Immunoreactive insulin, μg/m
Antihypertensive drug, n(%)
Antidyslipidemic drug, n(%)
Antidiabetic drug, n(%)
Smoking, current/past/never
1127
442 (39)
64.7±9.3
157.8±8.5
57.8±10.2
23.1±3.0
134.6±19.0
77.0±11.0
127.3±19.3
66.1±9.9
218.3±36.7
67.6±18.1
107.9±60.1
102.7±17.6
5.65±3.78
294 (26)
246 (22)
57 (5)
78/299/750
Brachial-ankle PWV, cm/sec
1562±328
Deep and subcortical white matter hyperintensity grade
p
DSWMH0-1
DSWMH2
DSWMH3+
p
169
80 (47)
69.4±7.0
156.4±8.6
58.2±10.6
23.7±3.0
142.5±21.1
80.7±12.3
135.4±21.7
66.8±10.3
215.1±37.0
65.2±19.6
107.3±58.6
109.0±25.6
6.30±4.15
87 (51)
45 (27)
20 (12)
10/54/105
0.046
<0.0001
0.052
0.64
0.027
<0.0001
<0.0001
<0.0001
0.42
0.30
0.13
0.90
<0.0001
0.039
<0.0001
0.17
0.0016
0.34
727
280 (40)
62.8±9.7
158.5±8.6
58.2±10.4
23.1±3.0
132.5±19.6
76.8±11.4
125.4±19.8
66.0±10.2
217.7±35.5
67.6±18.1
109.9±64.2
102.2±18.2
5.50±3.69
158 (22)
148 (20)
34 (5)
55/195/477
462
164 (41)
68.0±7.3
156.8±8.3
57.6±10.0
23.3±3.0
138.6±18.1
78.4±10.8
131.2±18.7
66.4±9.5
219.0±39.4
67.3±18.9
105.5±54.7
104.1±17.0
5.97±3.79
167 (36)
106 (23)
33 (7)
26/131/305
107
36 (37)
71.2±5.8
154.6±8.0
56.4±9.9
23.5±2.9
143.6±20.4
78.7±11.6
136.3±21.1
66.7±10.5
214.2±32.5
64.7±17.4
104.7±49.8
109.7±28.2
6.23±4.82
56 (52)
37 (35)
10 (9)
7/27/73
0.84
<0.0001
<0.0001
0.20
0.23
<0.0001
0.028
<0.0001
0.66
0.46
0.32
0.39
0.0005
0.046
<0.0001
0.0064
0.072
0.71
1722±326
<0.0001
1531±337
1634±307
1764±344
<0.0001
Values are mean ±SD. BP, blood pressure; HDL, high density lipoprotein; PWV, pulse wave velocity.
Supplemental table III. Parameters related to mechanical stressess in subjects devided by the presence of silent lacuar infarct and
severity of deep and subcortical white matter hyperinteisity
Deep and subcortical wthite matter hyperintensity grad
Silent lacuanr infarct
SLI (-)
n
1127
Carotid peak systolic dimension, m 6.55±0.80
Carotid end diastolic dimension, mm 6.06±0.77
Peak systolic flow velocity, cm/s
74.3±16.9
End diastolic flow velocity, cm/s
20.9±5.8
Hematocrit (%)
42.3±3.6
Total protein, g/dl
7.39±0.38
Viscosity at 104/s, cP
4.36±0.45
Viscosity at 52/s, cP
4.96±0.52
Peak systolic shear rate, /sec
46.6±13.9
End diastolic shear rate, /sec
14.2±5.1
Values are mean ±SD.
SLI (+)
p
169
6.85±0.82
636±0.80
71.0±16.2
19.0±6.1
42.5±3.7
7.40±0.40
4.38±0.47
4.98±0.55
42.8±13.3
12.4±5.2
<0.0001
<0.0001
0.021
0.0001
0.50
0.98
0.52
0.52
0.0014
<0.0001
DSWMH0-1 DSWMH2 DSWMH3+
727
6.50±0.79
6.01±0.77
75.6±17.5
21.5±5.9
42.4±3.6
7.38±0.37
4.36±0.45
4.96±0.52
47.8±14.4
14.8±5.2
462
6.66±0.81
6.17±0.79
71.9±15.5
19.7±5.8
42.5±3.4
7.41±0.40
4.38±0.42
4.98±0.49
44.3±12.9
13.2±5.0
107
6.85±0.79
6.37±0.75
67.9±14.0
18.0±4.9
41.4±4.3
7.44±0.39
4.26±0.54
4.84±0.63
40.5±10.7
11.6±4.0
p
<0.0001
<0.0001
<0.0001
<0.0001
0.014
0.17
0.031
0.031
<0.0001
<0.0001
Supplemental table IV. Multiple regression analysis for second peak systolic wall tension and peak systolic shear stress.
Second peak systolic pressure wall tension
SVD
Parameter
Age, years
Sex, female=1
Body mass index, kg/m2
Total cholesterol, mg/dl
HDL cholesterol, mg/dl
Triglyceride, mg/dl
Fasting glucose, mg/dl
Immuno reactive isulin, μg/ml
Use of antihypertensive drugs, yes=1
Anti-dyslipidemic drugs, yes=1
Anti-diabetic drugs, yes=1
Current smoking, yes=1
baPWV, cm/sec
SBP2, mmHg
Ds, mm
SVD, presence=1
SBP2*SVD
Ds*SVD
Peak systolic shear stress
SLI presence
DSWMH grade>=3
SLI presence
DSWMH grade>=3
n=1294
n=1294
n=1198
n=1198
beta
-0.01
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.72
0.58
0.00
0.02
0.01
p
0.0071
0.4505
0.0008
0.5179
0.5547
0.6978
0.843
0.7192
0.3793
0.9863
0.4513
0.3571
0.3466
<.0001
<.0001
0.1688
<.0001
0.0061
beta
-0.01
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.71
0.58
0.00
0.01
0.02
p
0.0065
0.4621
0.0003
0.4882
0.6903
0.8641
0.8121
0.6603
0.5906
0.7822
0.2815
0.4471
0.3637
<.0001
<.0001
0.0758
0.0077
0.0006
beta
-0.17
-0.34
0.01
0.06
-0.05
0.00
0.02
0.04
0.03
-0.02
0.00
0.00
0.03
-0.05
-0.76
-0.02
0.06
-0.01
p
<.0001
<.0001
0.5629
0.0112
0.0342
0.8880
0.3920
0.1231
0.1012
0.3668
0.8667
0.9635
0.2012
0.1201
<.0001
0.3189
0.0393
0.7999
beta
-0.17
-0.34
0.02
0.06
-0.05
0.00
0.03
0.04
0.03
-0.02
0.01
0.00
0.03
-0.04
-0.75
0.03
0.05
-0.03
p
<.0001
<.0001
0.4717
0.0095
0.0310
0.9551
0.2717
0.1311
0.1746
0.2990
0.8100
0.9670
0.1822
0.2268
<.0001
0.2101
0.1809
0.4679
SVD, small vessel disease; SLI, silent lacunar infarct; DSWMH, deep subcortical white matter hyperintensitiy; BMI, body mass index; HDL,
high density lipoprotein; baPWV, brachial-ankle pulse wave velocity; SBP2, second peak systolic blood pressure; Ds, carotid arteial systolic
demension.
Supplemental table V. Multiple regression analysis for peak systolic wall tension and shear stress.
SVD
Parameter
Age, years
Sex, female=1
Body mass index, kg/m2
Total cholesterol, mg/dl
HDL cholesterol, mg/dl
Triglyceride, mg/dl
Fasting glucose, mg/dl
Immuno reactive isulin, μg/ml
Use of antihypertensive drugs, yes=1
Anti-dyslipidemic drugs, yes=1
Anti-diabetic drugs, yes=1
Current smoking, yes=1
baPWV, cm/sec
SBP, mmHg
Ds, mm
SVD
SBP*SVD
Ds*SVD
Peak systolic wall tension
SLI presence
DSWMH grade>=3
n=1294
n=1294
beta
-0.01
0.00
-0.01
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.68
0.59
0.00
-0.02
-0.01
p
0.0065
0.5277
0.0007
0.5475
0.6221
0.6958
0.5340
0.5781
0.2551
0.8086
0.2103
0.7100
0.9575
<.0001
<.0001
0.3790
<.0001
0.0364
beta
-0.01
0.00
-0.01
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.68
0.60
0.00
-0.01
-0.01
p
0.0068
0.5325
0.0004
0.4971
0.7644
0.7843
0.5555
0.7031
0.5074
0.5881
0.0833
0.8419
0.9486
<.0001
<.0001
0.0536
0.0018
0.0010
Peak systolic shear stress
SLI presence
DSWMH grade>=3
n=1198
n=1198
beta
-0.18
-0.34
0.01
0.06
-0.05
0.00
0.02
0.04
0.04
-0.02
0.00
0.00
0.02
-0.02
-0.76
-0.02
0.06
-0.01
p
<.0001
<.0001
0.6548
0.0124
0.0265
0.9274
0.3779
0.1252
0.0818
0.3706
0.8732
0.9675
0.5664
0.5395
<.0001
0.3095
0.0230
0.7266
beta
-0.17
-0.34
0.01
0.06
-0.05
0.00
0.03
0.04
0.03
-0.02
0.01
0.00
0.02
-0.02
-0.75
0.03
0.05
-0.03
p
<.0001
<.0001
0.5509
0.0112
0.0265
0.9258
0.2633
0.1256
0.1473
0.2920
0.7993
0.9733
0.5067
0.6406
<.0001
0.2155
0.1419
0.4112
SVD, small vessel disease; SLI, silent lacunar infarct; DSWMH, deep subcortical white matter hyperintensitiy; BMI, body mass index;
HDL, high density lipoprotein; baPWV, brachial-ankle pulse wave velocity; SBP, systolic blood pressure; Ds, carotid arterial systolic
demension.
Supplemental table VI. Multiple regression analysis for end diastolic wall tension and end diastolic shear stress.
SVD
Parameter
Age, years
Sex, female=1
Body mass index, kg/m2
Total cholesterol, mg/dl
HDL cholesterol, mg/dl
Triglyceride, mg/dl
Fasting glucose, mg/dl
Immuno reactive isulin, μg/ml
Use of antihypertensive drugs, yes=1
Anti-dyslipidemic drugs, yes=1
Anti-diabetic drugs, yes=1
Current smoking, yes=1
baPWV, cm/sec
DBP, mmHg
Ds, mm
SVD
DBP*SVD
Ds*SVD
End diastolic wall tension
SLI presence
DSWMH grade>=3
n=1294
n=1294
beta
-0.01
0.00
-0.01
0.00
0.01
0.01
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.69
0.62
0.00
-0.02
0.00
p
0.0006
0.2156
0.0444
0.4506
0.0033
0.0029
0.1885
0.9193
0.7076
0.2022
0.7599
0.4830
0.4211
<.0001
<.0001
0.4740
<.0001
0.2395
beta
-0.01
0.00
-0.01
0.00
0.01
0.01
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.70
0.61
0.00
-0.02
0.01
p
0.0011
0.1423
0.0315
0.3754
0.0075
0.0032
0.2681
0.8536
0.8721
0.0952
0.5524
0.5653
0.4345
<.0001
<.0001
0.6255
<.0001
0.0383
End diastolic shear stress
SLI presence
DSWMH grade>=3
n=1198
n=1198
beta
-0.26
-0.05
-0.03
0.05
-0.07
-0.02
-0.01
0.03
0.04
-0.02
0.03
-0.02
-0.04
0.07
-0.63
-0.01
0.03
-0.01
p
<.0001
0.0292
0.1529
0.0278
0.0037
0.3455
0.7763
0.1721
0.0443
0.2788
0.2359
0.2076
0.1439
0.0165
<.0001
0.5762
0.3425
0.8395
beta
-0.25
-0.05
-0.03
0.05
-0.07
-0.03
0.00
0.03
0.04
-0.03
0.03
-0.03
-0.04
0.05
-0.61
0.03
0.04
-0.03
p
<.0001
0.0337
0.1546
0.0225
0.0033
0.2773
0.9422
0.1580
0.0722
0.2197
0.2146
0.1804
0.1608
0.1281
<.0001
0.1053
0.2588
0.3822
SVD, small vessel disease; SLI, silent lacunar infarct; DSWMH, deep subcortical white matter hyperintensitiy; BMI, body mass index;
HDL, high density lipoprotein; baPWV, brachial-ankle pulse wave velocity; DBP, diastolic blood pressure; Dd, carotid arterial diastolic
demension.