European Heart Journal Advance Access published April 28, 2015
European Heart Journal
doi:10.1093/eurheartj/ehv150
CURRENT OPINION
The role of heart rate may differ according
to pathophysiological setting: from SHIFT
to SIGNIFY
Roberto Ferrari 1* and Kim M. Fox 2
1
Department of Cardiology and LTTA Centre, University Hospital of Ferrara and Maria Cecilia Hospital, GVM Care & Research, E.S. Health Science Foundation, Cotignola, Italy;
and 2NHLI Imperial College, ICMS Royal Brompton Hospital, London, UK
Received 31 August 2014; revised 4 December 2014; accepted 20 March 2015
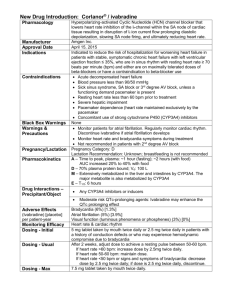
The results of the SIGNIFY (study assessing the morbidity –mortality
benefits of the If inhibitor ivabradine in patients with coronary artery
disease) trial, which were recently published in the New England
Journal of Medicine,1 raise an important pathophysiological question
regarding the relationship between elevated heart rate and outcomes
in cardiovascular disease. Why did heart rate reduction with ivabradine improve prognosis in patients with chronic heart failure and left
ventricular (LV) systolic dysfunction in the SHIFT (systolic heart
failure treatment with the If inhibitor ivabradine trial) study,2 but
not in patients with stable coronary artery disease (CAD) without
heart failure and LV systolic dysfunction in SIGNIFY?
Trial results for ivabradine in
patients with cardiovascular
disease
The 19 102 patients recruited in SIGNIFY presented with stable CAD
plus additional cardiovascular risk factors and resting heart rate
≥70 bpm.1 The SIGNIFY investigators deliberately recruited
patients with no symptoms of heart failure or LV systolic dysfunction:
the population had a mean left ventricular ejection fraction (LVEF) at
baseline of 56.5 + 8.6%.3 All were receiving guideline-based background therapy for their condition. In this stable CAD population,
ivabradine had no effect on the primary endpoint, a composite of cardiovascular death or non-fatal myocardial infarction (MI), with annual
event rates of 3.0% with ivabradine and 2.8% with placebo (hazard
ratio [HR] 1.08, 95% confidence interval [CI], 0.96 –1.20, P ¼
0.20).1 There were no significant differences between the groups in
terms of any of the secondary endpoints including cardiovascular
death (HR 1.10, P ¼ 0.25), non-fatal MI (HR 1.04, P ¼ 0.60), or
all-cause death (HR 1.06, P ¼ 0.35). Treatment with ivabradine was
associated with an increase in primary composite endpoint in a subgroup of 12 049 patients with angina Canadian Cardiovascular
Society (CCS) 2 and higher (63% of the whole population) vs.
those on placebo (HR 1.18, P ¼ 0.018, in patient with CCS class 2
angina or higher; P ¼ 0.02 for interaction). There was no significant
effect of ivabradine on the components of the primary endpoint or
the main secondary endpoints in this angina population. There was
no interaction between the use of ivabradine and outcomes in
seven other pre-specified sub-groups, which were defined according
to age, b-blocker use at baseline, sex, heart rate at baseline, history of
diabetes, previous MI, or previous coronary revascularization.
The SIGNIFY results are in sharp contrast with those of SHIFT,
which included a completely different population with symptomatic
heart failure of ischaemic and non-ischaemic origin. SHIFT included
6558 patients with chronic heart failure, resting heart rate
≥70 bpm, and a baseline LVEF of 29.0 + 5.1%, who were also receiving guideline-based background therapy.2 Treatment with ivabradine
was associated with a highly significant effect on the primary composite outcome of cardiovascular death and hospitalization for heart
failure (annual event rates 14 and 18%; HR 0.82, 95% CI, 0.75–
0.90, P , 0.0001). The effect was found to be driven mainly by
heart failure hospitalization, the risk of which was reduced by 26%
(P , 0.0001). There was no difference in the effect of ivabradine
between ischaemic and non-ischaemic heart failure, with a similar
magnitude of risk reduction whatever the origin of heart failure (nonischaemic heart failure, HR 0.72, 95% CI 0.60 –0.85; ischaemic heart
failure, HR 0.87, 95% CI 0.78 –0.97; P ¼ 0.059 for interaction).
There were a number of differences between the two studies
(Table 1).1 – 6 Notably, SIGNIFY used a regimen involving higher initiation and uptitration doses (7.5 and 10 mg bid, respectively) than in
SHIFT. Therefore, SIGNIFY reported a lower heart rate achieved
(63% of SIGNIFY patients had heart rate ,55 bpm at least one
visit vs. 48% of SHIFT patients) and a higher incidence of bradycardia
(18% vs. 10% in SHIFT). The SIGNIFY population was also at much
The opinions expressed in this article are not necessarily those of the Editors of the European Heart Journal or of the European Society of Cardiology.
* Corresponding author. Email: fri@unife.it
Published on behalf of the European Society of Cardiology. All rights reserved. & The Author 2015. For permissions please email: journals.permissions@oup.com.
Downloaded from http://eurheartj.oxfordjournals.org/ by guest on September 30, 2016
Introduction
Page 2 of 5
Table 1
R. Ferrari and K.M. Fox
Main features of the populations of SIGNIFY, BEAUTIFUL with heart rate ≥70 bpm, and SHIFT1 – 6
SIGNIFY (n 5 19 102)
BEAUTIFUL with heart rate
≥70 bpm (n 5 5392)
SHIFT (n 5 6505)
...............................................................................................................................................................................
Main inclusion criteria
Age (years)
≥55
≥55
≥18
Primary diagnosis
Heart rate (bpm)
CAD
≥70
CAD
≥70
Symptomatic HF
≥70
LV dysfunction
No (LVEF . 40%)
Yes (LVEF , 40%)
Yes (LVEF ≤ 35%)
Characteristics at randomization a
Age (years)
65.0 (7.2)
64.6 (8.6)
60.4 (11.4)
Heart rate (bpm)
77.2 (7.0)
79.2 (8.6)
79.9 (9.6)
LVEF (%)
History of CAD
56.5 (8.6)
19 102 (100%)
32.0 (5.6)
5392 (100%)
29.0 (5.1)
4732 (73%)
Class I
Class II
Not assessed
Not assessed
762 (14%)
3190 (59%)
0
3169 (49%)
Class III
NYHA class
1440 (27%)
3223 (50%)
Not assessed
No angina, 4812 (25%)
CCS Class I, 2239 (12%)
CCS Classes II to IV, 12 051 (63%)
0
No angina, 4680 (87%)
Limiting angina, 712 (13%)
111 (2%)
Not assessed
Dosage of study
treatment
Starting dose of 7.5 mg bid titrated to
maximum of 10 mg bid or matching
placebo
Patients ≥75 years were initiated at
5 mg bid
Starting dose of 5 mg bid titrated to
maximum of 7.5 mg bid or matching
placebo
Patients ≥75 years were initiated at
2.5 mg bid
Starting dose of 5 mg bid titrated to
maximum of 7.5 mg bid or matching
placebo
Patients ≥75 years were initiated at
2.5 mg bid
Primary endpoint
Composite of CV mortality and non-fatal
MI
Composite of CV mortality, hospital
admission for HF, or hospital
admission for MI
Composite of CV mortality or hospital
admission for HF
Secondary outcomes
Individual components of the primary
endpoint, all-cause mortality
Individual components of the primary
endpoint, all-cause mortality
Individual components of the primary
endpoint; all-cause mortality; HF
mortality; composite of CV mortality,
hospital admission for HF, or hospital
admission for non-fatal MI
Recruitment period
October 2009 to April 2012
January 2005 to December 2006
October 2006 to June 2009
Median duration of
follow-up
27.8 months (IQR 21– 35)
19 months (IQR 15– 24)
23 months (IQR 18– 28)
Main outcomes
Recruitment
CAD, coronary artery disease; CV, cardiovascular; HF, heart failure; LVEF, left ventricular ejection fraction; MI, myocardial infarction; NYHA, New York Heart Association.
a
Values are number of patients (%) or mean (SD).
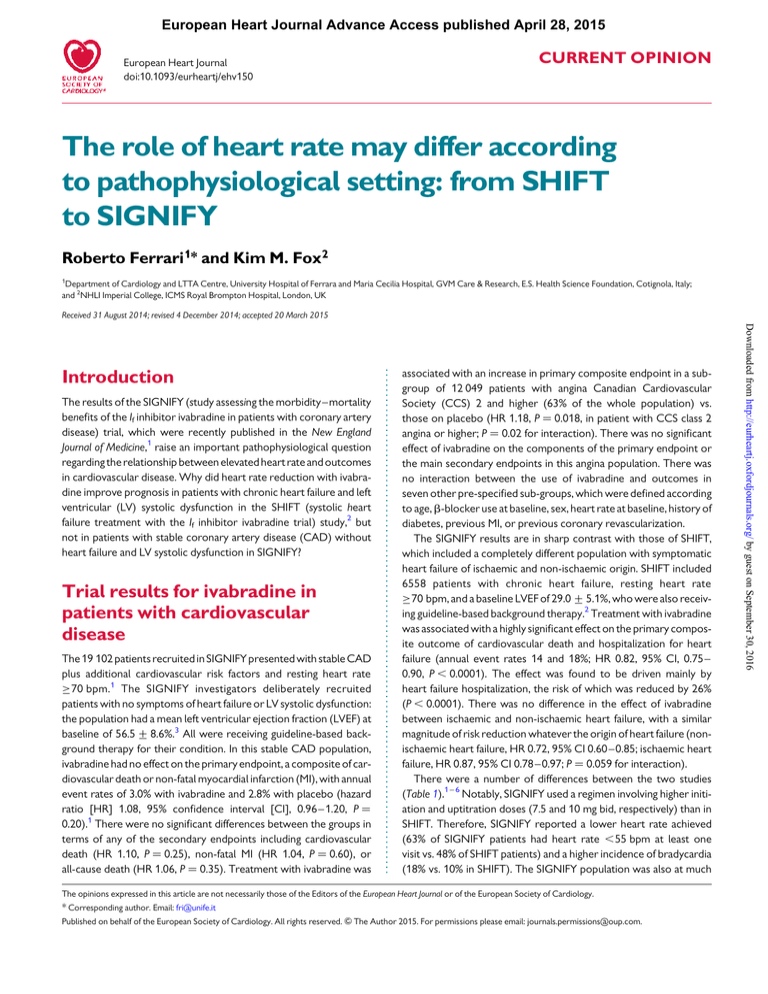
lower cardiovascular risk (annual incidence for CV mortality 1.4% vs.
8.5% in SHIFT). Another major difference between the two studies is
that there was heart failure in SHIFT, but not in SIGNIFY, i.e. the
patients had LV dysfunction in SHIFT, but normal LV function in
SIGNIFY. Heart rate reduction was associated with an improvement
in prognosis in patients with low LVEF in SHIFT, but had no impact on
risk in patients with normal LVEF in SIGNIFY. As ivabradine has no
haemodynamic effects other than heart rate reduction through inhibition of the If channel, this implies that effects of elevated heart rate
differ according to LV function (Figure 1).
The results of the BEAUTIFUL (morbidity–mortality evaluation of
the If inhibitor ivabradine in patients with coronary disease and leftventricular dysfunction) trial4 can be regarded as being intermediate
to those of SHIFT and SIGNIFY (Table 1, Figure 1), since the patients in
that trial have stable CAD with LV systolic dysfunction (LVEF ¼ 32%
and New York Heart Association heart failure classes I to III). As
there was no inclusion criterion regarding heart rate in BEAUTIFUL
(beyond a heart rate ≥60 bpm), for proper comparison, Table 1
includes the pre-specified sub-group of BEAUTIFUL patients with
elevated heart rate (≥70 bpm). In these patients, ivabradine did
not affect the primary composite endpoint of cardiovascular death,
hospitalization for acute MI, and hospitalization for heart failure
(event rates 17.2 and 18.5%; HR 0.91, 95% CI 0.81 –1.04, P ¼ 0.17).
An echocardiographic sub-study of BEAUTIFUL also reported evidence that ivabradine could reverse cardiac remodelling in patients
with LV dysfunction.7
Downloaded from http://eurheartj.oxfordjournals.org/ by guest on September 30, 2016
Not assessed
Class IV
Angina status
The role of heart rate from SHIFT to SIGNIFY
Page 3 of 5
The role of heart rate in left
ventricular systolic dysfunction
The role and significance of an increase in heart rate in heart failure is
complex. In heart failure, heart rate reflects the degree of neuroendocrine stimulation, i.e. sympathetic activation, which is known to be
beneficial in the short term, but detrimental in the long term.8 The
elevation of heart rate is closely associated with stroke volume,
and so its early increase could be considered as a compensatory
mechanism. However, this is only true in the initial stages; prolonged
neuroendocrine activation has deleterious effects on the myocytes
resulting in ventricular changes for the worse and remodelling
of the ventricle, another complex phenomenon whereby the ventricles progressively enlarge and ejection fraction reduces. It follows
that, in these later stages, an increased heart rate is identified as
a marker of the progression of disease and adverse prognosis.
This has been clearly demonstrated by the results of the SHIFT
study, showing that the higher baseline heart rate, the worse the
outcome and, conversely, that the more heart rate could be
reduced by ivabradine (which lacks any other effects), the greater
the reduction in risk.9 This is because elevation of heart rate
itself has pathological effects, including generation of a further
deterioration of LV systolic function, which in turn increases heart
rate as the ventricle enters a vicious circle of decline. This so-called
tachycardia-mediated cardiomyopathy has been reported in a
number of animal models and clinical studies.10 – 13 Exploration of
the effect of different pacing rates in heart failure patients with
implanted pacemakers has demonstrated that heart rate per se
impacts LV dysfunction, with increases in volumes and reduction in
ejection fraction at higher rates of pacing.14,15 As heart failure progresses, the force-frequency relationship—by which the normal
heart regulates cardiac function—becomes negative and the compensatory mechanism of increased heart rate is lost; myocardial contractility no longer improves with increasing heart rate. On the
contrary, it further deteriorates, leading to progression of LV dysfunction.13 The situation is further aggravated by a heart rateassociated increase in energy deprivation, inducing hypoxia, which
stimulates local production of a range of cytokines, free radicals,
and vasoconstrictors implicated in the development of LV remodelling.16 Our data are supported by studies in patients with LV dysfunction.17 Furthermore, an analysis from a registry of 3079 post-MI
patients explored the interaction between the impact of heart rate
on 5-year mortality and the presence or absence of LV dysfunction.
Elevated heart rate at discharge had no impact on outcomes in
Downloaded from http://eurheartj.oxfordjournals.org/ by guest on September 30, 2016
Figure 1 Comparison of left ventricular function at baseline in SIGNIFY, BEAUTIFUL, and SHIFT, expressed as ejection fraction (top panel) and
the effect of heart rate reduction with ivabradine on prognosis in SHIFT, BEAUTIFUL (patients with heart rate ≥70 bpm), and SIGNIFY, expressed as
absolute risk reduction in primary composite outcomes (bottom panel). CAD, coronary artery disease; CV, cardiovascular; HF, heart failure; LVSD,
left ventricular systolic dysfunction; MI, myocardial infarction.
Page 4 of 5
The SIGNIFY results show that elevated resting heart rate is just a
risk marker in stable CAD, and not a risk factor. Indeed, the increased
heart rate in the SIGNIFY population cannot have been generated by
an impairment of LV function, as described for heart failure. While it is
unclear as to why these patients have elevated resting heart rate
(≥70 bpm), it may well be that this is what the body requires for
proper coronary function and its further reduction is irrelevant for
prognosis but relevant for symptom improvement. Elevated heart
rate certainly has a number of other pathophysiological effects,
notably in the vascular system,32 and correlates with other cardiovascular risk factors such as atherogenic blood lipid profile, blood
glucose, insulin levels, and obesity.29,33,34 These associations probably contribute to its role as a marker of CAD.
Conclusion
The results of the SIGNIFY trial have added to our knowledge of the
role of heart rate in cardiovascular disease. Elevated heart rate is an
important risk factor for ventricular remodelling in heart failure,
and therefore for a poor prognosis in that setting. On the other
hand, in cardiovascular disease without LV dysfunction or overt
heart failure, increased heart rate is determinant of symptoms, and
appears to be a marker of other processes that influence the development of MI (e.g. diabetes and smoking). This merits further exploration by meta-analysis in the ivabradine trials. The SIGNIFY and
SHIFT results are set to lead to a better understanding of the interaction between elevated heart rate and LV function.
Funding
The role of heart rate in coronary
artery disease
In stable CAD, heart rate is a well-established determinant of ischaemia. In line with experimental data, clinical results indicate that elevations of heart rate during physical or emotional stress induce
ischaemia and angina.24 Consistent with this, heart rate reduction is
a recognized strategy for the prevention of ischaemia and therefore
of angina symptoms. Heart rate reduction with ivabradine has been
demonstrated to improve angina symptoms,25,26 since it reduces
both resting heart rate and on exercise, which is when ischaemia is
most likely to occur. In line with this, a heart rate of 55–60 bpm is currently recommended for optimal anti-anginal efficacy of b-blockers
and ivabradine in stable CAD.27,28 Furthermore, experimental and
clinical data suggested that heart rate may be involved in the progression of atherosclerosis and plaque rupture leading to MI.29,30 This was
the underlying rationale for the SIGNIFY study. The results confirm
the symptomatic benefit of ivabradine, as shown by an improvement
in angina class, but do not show a prognostic benefit (Figure 1)
opening the question of whether heart rate under these conditions
is a risk marker or merely an epiphenomenon of an underlying pathophysiological process. Interestingly, even the ‘hypothetical’ prognostic benefits of b-blockers in stable CAD patients have been
extrapolated by rather old studies on patients with MI, but never
demonstrated in stable CAD, in contrast with the well-accepted
prognostic impact on heart failure. In line with the SIGNIFY results,
registry data suggest that there is no prognostic benefit of b-blockers
in the stable coronary population.31
K.F. is an NIHR senior investigator supported by the NIHR Biomedical
Research Unit at the Royal Brompton Hospital.
Conflict of interest: none declared.
References
1. Fox K, Ford I, Steg PG, Tardif JC, Tendera M, Ferrari R. Ivabradine in stable coronary
artery disease without clinical heart failure. N Engl J Med 2014;371:1091 –1099.
2. Swedberg K, Komajda M, Böhm M, Borer J, Ford I, Dubost-Brama A, Lerebours G,
Tavazzi L. Ivabradine and outcomes in chronic heart failure (SHIFT): a randomised
placebo-controlled trial. Lancet 2010;376:875 –885.
3. Fox K, Ford I, Steg PG, Tardif JC, Tendera M, Ferrari R. Rationale, design, and baseline
characteristics of the Study assessInG the morbidity-mortality beNefits of the If inhibitor ivabradine in patients with coronarY artery disease (SIGNIFY trial): a randomized, double-blind, placebo-controlled trial of ivabradine in patients with stable
coronary artery disease without clinical heart failure. Am Heart J 2013;166:654 –661.
4. Fox K, Ford I, Steg PG, Tendera M, Ferrari R. Ivabradine for patients with stable coronary artery disease and left-ventricular systolic dysfunction (BEAUTIFUL): a randomised, double-blind, placebo-controlled trial. Lancet 2008;372:807 –816.
5. Fox K, Ford I, Steg PG, Tendera M, Robertson M, Ferrari R. Relationship between
ivabradine treatment and cardiovascular outcomes in patients with stable coronary
artery disease and left ventricular systolic dysfunction with limiting angina: a subgroup analysis of the randomized, controlled BEAUTIFUL trial. Eur Heart J 2009;
30:2337 –2345.
6. Fox K, Komajda M, Ford I, Robertson M, Bohm M, Borer JS, Steg PG, Tavazzi L,
Tendera M, Ferrari R, Swedberg K. Effect of ivabradine in patients with leftventricular systolic dysfunction: a pooled analysis of individual patient data from
the BEAUTIFUL and SHIFT trials. Eur Heart J 2013;34:2263 –2270.
7. Ceconi C, Freedman SB, Tardif JC, Hildebrandt P, McDonagh T, Gueret P,
Parrinello G, Robertson M, Steg PG, Tendera M, Ford I, Fox K, Ferrari R. Effect of
heart rate reduction by ivabradine on left ventricular remodeling in the echocardiographic substudy of BEAUTIFUL. Int J Cardiol 2011;146:408 – 414.
8. Harris P. Role of arterial pressure in the oedema of heart disease. Lancet 1988;1:
1036 –1038.
9. Bohm M, Swedberg K, Komajda M, Borer JS, Ford I, Dubost-Brama A, Lerebours G,
Tavazzi L. Heart rate as a risk factor in chronic heart failure (SHIFT): the association
Downloaded from http://eurheartj.oxfordjournals.org/ by guest on September 30, 2016
patients with preserved LV function, but was associated with an 80%
increase in patients with LV dysfunction (i.e. 18% per 10 bpm).18
In the experimental setting, pure heart rate reduction with ivabradine improved cardiac function by significantly decreasing LV systolic
diameter, increasing fractional shortening, and preservation of
cardiac output.16,19 This was associated with a positive impact on
LV morphology with reduced collagen density and increased capillary
density.16 Similar cardiac benefits were also observed in experimental post-MI remodelling,20,21 including normalization of biomarkers
relevant to heart failure, such as circulating norepinephrine, brain
natriuretic peptide, as well as inflammatory cytokines, with preservation of cardiac energy metabolism, which is profoundly depleted
during heart failure.19
Reversal of cardiac remodelling with ivabradine has also been confirmed in the setting of clinical LV dysfunction. In an echocardiographic sub-study of 400 participants in the SHIFT trial,22 ivabradine
was found to significantly improve LV end diastolic volume index
(27.9 + 18.9 with ivabradine vs. 21.8 + 19.0 mL/m2 with placebo,
P ¼ 0.002) and LVEF (+2.4 + 7.7% vs. 20.1 + 8.0%, P , 0.001).
Moreover, patients with the largest relative reduction in LV volumes
on treatment had the lowest primary event rates, implying that
heart rate reduction with ivabradine breaks the vicious circle, and
modifies disease progression in heart failure. A similar favourable
impact of ivabradine on LV remodelling has also been reported in
CAD patients with LV dysfunction7 and in post-MI patients.23 It
follows that, today, elevated heart rate is considered as an independent risk factor in heart failure with LV dysfunction.
R. Ferrari and K.M. Fox
Page 5 of 5
The role of heart rate from SHIFT to SIGNIFY
10.
11.
12.
13.
14.
15.
16.
18.
19.
20.
21.
22.
23.
24.
25.
26.
27.
28.
29.
30.
31.
32.
33.
34.
daily life in patients with stable coronary artery disease. J Am Coll Cardiol 1992;20:
1092 –1098.
Borer JS, Fox K, Jaillon P, Lerebours G. Antianginal and antiischemic effects of ivabradine, an I(f) inhibitor, in stable angina: a randomized, double-blind, multicentered,
placebo-controlled trial. Circulation 2003;107:817 –823.
Tardif JC, Ford I, Tendera M, Bourassa MG, Fox K. Efficacy of ivabradine, a new selective I(f) inhibitor, compared with atenolol in patients with chronic stable
angina. Eur Heart J 2005;26:2529 – 2536.
Fihn SD, Gardin JM, Abrams J, Berra K, Blankenship JC, Dallas AP, Douglas PS,
Foody JM, Gerber TC, Hinderliter AL, King SB 3rd, Kligfield PD, Krumholz HM,
Kwong RY, Lim MJ, Linderbaum JA, Mack MJ, Munger MA, Prager RL, Sabik JF,
Shaw LJ, Sikkema JD, Smith CR Jr, Smith SC Jr, Spertus JA, Williams SV,
Anderson JL. 2012 ACCF/AHA/ACP/AATS/PCNA/SCAI/STS guideline for the diagnosis and management of patients with stable ischemic heart disease: a report of the
American College of Cardiology Foundation/American Heart Association task force
on practice guidelines, and the American College of Physicians, American Association for Thoracic Surgery, Preventive Cardiovascular Nurses Association,
Society for Cardiovascular Angiography and Interventions, and Society of Thoracic
Surgeons. Circulation 2012;126:e354–e471.
Montalescot G, Sechtem U, Achenbach S, Andreotti F, Arden C, Budaj A,
Bugiardini R, Crea F, Cuisset T, Di MC, Ferreira JR, Gersh BJ, Gitt AK, Hulot JS,
Marx N, Opie LH, Pfisterer M, Prescott E, Ruschitzka F, Sabate M, Senior R,
Taggart DP, van der Wall EE, Vrints CJ, Zamorano JL, Achenbach S,
Baumgartner H, Bax JJ, Bueno H, Dean V, Deaton C, Erol C, Fagard R, Ferrari R,
Hasdai D, Hoes AW, Kirchhof P, Knuuti J, Kolh P, Lancellotti P, Linhart A,
Nihoyannopoulos P, Piepoli MF, Ponikowski P, Sirnes PA, Tamargo JL, Tendera M,
Torbicki A, Wijns W, Windecker S, Knuuti J, Valgimigli M, Bueno H, Claeys MJ,
Donner-Banzhoff N, Erol C, Frank H, Funck-Brentano C, Gaemperli O,
Gonzalez-Juanatey JR, Hamilos M, Hasdai D, Husted S, James SK, Kervinen K,
Kolh P, Kristensen SD, Lancellotti P, Maggioni AP, Piepoli MF, Pries AR, Romeo F,
Ryden L, Simoons ML, Sirnes PA, Steg PG, Timmis A, Wijns W, Windecker S,
Yildirir A, Zamorano JL. 2013 ESC guidelines on the management of stable coronary
artery disease: The Task Force on the management of stable coronary artery disease
of the European Society of Cardiology. Eur Heart J 2013;34:2949 –3003.
Fox K, Borer JS, Camm AJ, Danchin N, Ferrari R, Lopez Sendon JL, Steg PG, Tardif JC,
Tavazzi L, Tendera M. Resting heart rate in cardiovascular disease. J Am Coll Cardiol
2007;50:823 –830.
Fox KM, Ferrari R. Heart rate: a forgotten link in coronary artery disease? Nat Rev
Cardiol 2011;8:369 – 379.
Bangalore S, Steg G, Deedwania P, Crowley K, Eagle KA, Goto S, Ohman EM,
Cannon CP, Smith SC, Zeymer U, Hoffman EB, Messerli FH, Bhatt DL. Beta-blocker
use and clinical outcomes in stable outpatients with and without coronary artery
disease. JAMA 2012;308:1340 – 1349.
Custodis F, Schirmer SH, Baumhakel M, Heusch G, Bohm M, Laufs U. Vascular pathophysiology in response to increased heart rate. J Am Coll Cardiol 2010;56:1973 –1983.
Palatini P, Casiglia E, Pauletto P, Staessen J, Kaciroti N, Julius S. Relationship of tachycardia with high blood pressure and metabolic abnormalities: a study with mixture
analysis in three populations. Hypertension 1997;30:1267 –1273.
Julius S, Palatini P, Nesbitt SD. Tachycardia: an important determinant of coronary
risk in hypertension. J Hypertens Suppl 1998;16:S9–15.
Downloaded from http://eurheartj.oxfordjournals.org/ by guest on September 30, 2016
17.
between heart rate and outcomes in a randomised placebo-controlled trial. Lancet
2010;376:886 –894.
Rao K, Fisher ML, Robinson S, Shorofsky S, Gottlieb SS. Effect of chronic changes in
heart rate on congestive heart failure. J Card Fail 2007;13:269 –274.
Shinbane JS, Wood MA, Jensen DN, Ellenbogen KA, Fitzpatrick AP, Scheinman MM.
Tachycardia-induced cardiomyopathy: a review of animal models and clinical studies.
J Am Coll Cardiol 1997;29:709–715.
Ferrari R. Ivabradine: heart rate and left ventricular function. Cardiology 2014;128:
226 –230.
Heusch G. Heart rate and heart failure. Not a simple relationship. Circ J 2011;75:
229 –236.
Logeart D, Gueffet JP, Rouzet F, Pousset F, Chavelas C, Solal AC, Jondeau G.
Heart rate per se impacts cardiac function in patients with systolic heart failure
and pacing: a pilot study. Eur J Heart Fail 2009;11:53– 57.
Thackray SD, Ghosh JM, Wright GA, Witte KK, Nikitin NP, Kaye GC, Clark AL,
Tweddel A, Cleland JG. The effect of altering heart rate on ventricular function in
patients with heart failure treated with beta-blockers. Am Heart J 2006;152:713.
Mulder P, Barbier S, Chagraoui A, Richard V, Henry JP, Lallemand F, Renet S,
Lerebours G, Mahlberg-Gaudin F, Thuillez C. Long-term heart rate reduction
induced by the selective I(f) current inhibitor ivabradine improves left ventricular
function and intrinsic myocardial structure in congestive heart failure. Circulation
2004;109:1674 –1679.
Fosbol EL, Seibaek M, Brendorp B, Moller DV, Thune JJ, Gislason GH,
Torp-Pedersen C, Kober L. Long-term prognostic importance of resting heart
rate in patients with left ventricular dysfunction in connection with either heart
failure or myocardial infarction: the DIAMOND study. Int J Cardiol 2010;140:
279 –286.
Seronde MF, Geha R, Puymirat E, Chaib A, Simon T, Berard L, Drouet E, Bataille V,
Danchin N, Schiele F. Discharge heart rate and mortality after acute myocardial
infarction. Am J Med 2014;127:954 –962.
Ceconi C, Comini L, Suffredini S, Stillitano F, Bouly M, Cerbai E, Mugelli A, Ferrari R.
Heart rate reduction with ivabradine prevents the global phenotype of left ventricular remodeling. Am J Physiol Heart Circ Physiol 2011;300:H366 –H373.
Dedkov EI, Zheng W, Christensen LP, Weiss RM, Mahlberg-Gaudin F, Tomanek RJ.
Preservation of coronary reserve by ivabradine-induced reduction in heart rate in
infarcted rats is associated with decrease in perivascular collagen. Am J Physiol
Heart Circ Physiol 2007;293:H590 –H598.
Milliez P, Messaoudi S, Nehme J, Rodriguez C, Samuel JL, Delcayre C. Beneficial
effects of delayed ivabradine treatment on cardiac anatomical and electrical remodeling in rat severe chronic heart failure. Am J Physiol Heart Circ Physiol 2009;296:
H435 –H441.
Tardif JC, O’Meara E, Komajda M, Bohm M, Borer JS, Ford I, Tavazzi L, Swedberg K.
Effects of selective heart rate reduction with ivabradine on left ventricular remodelling and function: results from the SHIFT echocardiography substudy. Eur Heart J
2011;32:2507 –2515.
Gerbaud E, Montaudon M, Chasseriaud W, Gilbert S, Cochet H, Pucheu Y,
Horovitz A, Bonnet J, Douard H, Coste P. Effect of ivabradine on left ventricular remodelling after reperfused myocardial infarction: a pilot study. Arch Cardiovasc Dis
2014;107:33–41.
Panza JA, Diodati JG, Callahan TS, Epstein SE, Quyyumi AA. Role of increases in heart
rate in determining the occurrence and frequency of myocardial ischemia during