Systolic Heart failure treatment with
the If inhibitor ivabradine Trial
Michel Komajda
on behalf of the
Investigators
Disclosures
SHIFT Executive Committee members received
fees, research grants, or both from Servier, as well
as fees for speaking or consulting from other major
cardiovascular pharmaceutical companies
Background
Elevated heart rate is associated with poor outcome in a
number of cardiovascular conditions including heart failure
Heart rate remains elevated in many heart failure patients
despite treatment by beta-blockers
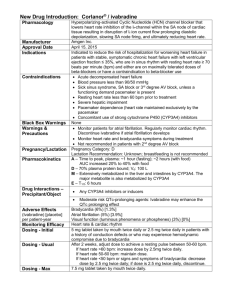
Ivabradine is a novel heart rate-lowering agent acting by
inhibiting the If current in the sino-atrial node
We hypothesized that the addition of ivabradine to
recommended therapy would be beneficial in heart failure
patients with elevated heart rate
Primary objective
To evaluate whether the If inhibitor ivabradine
improves cardiovascular outcomes
in patients with
1. Moderate to severe chronic heart failure
2. Left ventricular ejection fraction 35%
3. Heart rate 70 bpm and
4. Recommended therapy
Multinational study
Europe
Germany
Greece
Ireland
Italy
The Netherlands
Belgium
Denmark
Finland
France
Portugal
Spain
Sweden
Turkey
UK
Bulgaria
Czech Republic
Estonia
Hungary
Latvia
Lithuania
Norway
Poland
Romania
Russia
Slovakia
Slovenia
Ukraine
North America
Canada
South America
Argentina
Brazil
Chili
Asia
China
Hong Kong
India
South Korea
Malaysia
6505 patients, 37 countries, 677 centres
Australia
Study organisation
Executive Committee
M. Komajda co-chair, K. Swedberg co-chair
M. Böhm, J. Borer, I. Ford, L. Tavazzi
Steering Committee
Argentina:
S. Perrone
Australia:
H. Krum
Belgium: W. Van Mieghem
Brazil:
E. Bocchi
Bulgaria:
T. Katova
Canada:
P. Liu
Chile:
J. Jalil
China:
D. Hu
Czech Republic: J. Vitovec
Denmark:
L. Køber
Estonia:
T. Uuetoa
Finland:
M. Niemelä
France:
G. Jondeau
Germany:
K. Werdan
Greece: D. Kremastinos
Hong-Kong:
C. Yu
Hungary:
K. Tóth
India:
D. S. Rao
Ireland:
K. Mc Donald
Italy:
M. Metra
Latvia:
J. Jirgenson†
A. Erglis
Lithuania: A. Kavoliuniene
Malaysia:
K. Sim
The Netherlands: A. Voors
Norway:
K. Dickstein
Poland:
G. Opolski
Portugal: L. Providência
Romania:
D. Ionescu
Russia: G. Aroutiounov
Slovakia:
R. Hatala
Slovenia:
M. Sebestjen
South Korea:
B. Oh
Spain:
F. Avilés
Sweden: R. Willenheimer
Turkey:
A. Oto
United Kingdom:M. Cowie
Ukraine: O. Parkhomenko
Study organisation
Data Monitoring Committee
Endpoint Validation Committee
J.L. Lopez Sendon, chair
P. Poole-Wilson, chair († March 2009)
M. Alings
S. Pocock, chair (April 2009)
K. Dickstein
J-Y. Le Heuzey
A. Gavazzi
M. Nieminen
J.R. Gonzalez-Juanatey
J. Camm (April 2009)
E. Lopez de Sa
P. Ponikowski
Inclusion criteria
18 years
Class II to IV NYHA heart failure
Ischaemic/non-ischaemic aetiology
LV systolic dysfunction (EF 35%)
Heart rate 70 bpm
Sinus rhythm
Documented hospital admission for worsening heart failure
12 months
Swedberg K, et al. Eur J Heart Fail. 2010;12:75-81.
Study design
Ivabradine 5 mg bid
Ivabradine 7.5/5/2.5 mg bid according to
HR and tolerability
Screening
7 to 30 days
Matching placebo, bid
D0
D14
D28
3.5 years
Swedberg K, et al. Eur J Heart Fail. 2010;12:75-81.
M4
Every 4 months
Study endpoints
Primary composite endpoint
Cardiovascular death
Hospitalization for worsening heart failure
Other endpoints
All-cause / CV / HF death
All-cause / CV / HF hospitalization
Composite of CV death, hospitalization for HF or non-fatal MI
NYHA class / Patient & Physician Global Assessment
In total population and in patients with at least 50% target dose of beta-blockers
Swedberg K, et al. Eur J Heart Fail. 2010;12:75-81.
Patients and follow-up
7411 screened
6558 randomized
3268 to ivabradine
Excluded: 27
3290 to placebo
Excluded: 26
3241 analysed
3264 analysed
2 lost to follow-up
1 lost to follow-up
Median study duration: 22.9 months; maximum: 41.7 months
Baseline characteristics
Ivabradine
3241
Placebo
3264
60.7
60.1
Male, %
76
77
Ischaemic aetiology, %
68
67
NYHA II, %
49
49
NYHA III/IV, %
51
51
Previous MI, %
56
56
Diabetes, %
30
31
Hypertension, %
67
66
Mean age, y
Baseline characteristics
Ivabradine
3241
Placebo
3264
Mean heart rate, bpm
80
80
Mean LVEF, %
29
29
Mean SBP, mm Hg
122
121
Mean DBP, mm Hg
76
76
eGFR, mL/min/1.73 m2
75
75
Chronic HF background treatment
Patients (%)
100
90
89
90
91
91
84
Ivabradine
83
80
Placebo
70
61
59
60
50
40
30
22
22
20
10
3
4
0
Beta-blockers ACEIs and/or
ARBs
Diuretics
Aldosterone
antagonists
Digitalis
ICD/CRT
Background
beta-blocker treatment
Patients (%)
100
90
89
Ivabradine
89
Placebo
80
70
60
56
56
50
40
30
26
26
20
10
0
BB at
randomization
At least 50%
Target daily dose
target daily dose
Mean heart rate reduction
Mean ivabradine dose: 6.4 mg bid at 1 month
Heart rate (bpm)
6.5 mg bid at 1 year
90
Ivabradine
Placebo
80
80
75
75
70
67
64
60
50
0
2 weeks
1
4
8
12
16
Months
20
24
28
32
Primary composite endpoint
Ivabradine n=793 (14.5%PY)
Placebo n=937 (17.7%PY)
HR = 0.82 [95% CI 0.75-0.90] p<0.0001
Cumulative frequency (%)
40
Ivabradine
Placebo
- 18%
30
20
10
0
0
6
12
18
Months
24
30
Hospitalization for heart failure
Ivabradine n=514 (9.4%PY)
Cumulative frequency (%)
Placebo n=672 (12.7%PY)
HR = 0.74 [95% CI 0.66-0.83] p<0.0001
30
Ivabradine
Placebo
- 26%
20
10
0
0
6
12
18
Months
24
30
Cardiovascular death
Ivabradine n=449 (7.5%PY)
Cumulative frequency (%)
Placebo n=491 (8.3%PY)
HR = 0.91
p=0.128
18
24
30
Ivabradine
Placebo
20
10
0
0
6
12
Months
30
Effect of ivabradine on outcomes
Endpoints
Hazard ratio
95% CI
p value
Primary composite endpoint
0.82
[0.75;0.90]
p<0.0001
All-cause death
0.90
[0.80;1.02]
p=0.092
Death from HF
0.74
[0.58;0.94]
p=0.014
Hospitalisation for any cause
0.89
[0.82;0.96]
p=0.003
Hospitalisation for CV reason
0.85
[0.78;0.92]
p=0.0002
CV death/hospitalisation for HF
or non-fatal MI
0.82
[0.74;0.89]
p<0.0001
Effect of ivabradine in
prespecified subgroups
Test for interaction
Age
<65 years
≥65 years
Sex
Male
Female
Beta-blockers
No
Yes
Aetiology of heart failure
Non-ischaemic
Ischaemic
NYHA class
NYHA class II
NYHA class III or IV
Diabetes
No
Yes
Hypertension
No
Yes
Baseline heart rate
p=0.029
<77 bpm
≥77 bpm
0.5
1.0
Hazard ratio
Favours ivabradine
1.5
Favours placebo
Patients with at least 50% BB
target dose (n=3181)
Ivabradine
Primary composite
endpoint
Cardiovascular death
Hospitalisation for
worsening HF
Placebo
330
362
(11.9 PY)
(13.3 PY)
176
175
(5.9 PY)
(5.9 PY)
213
260
(7.7 PY)
(9.6 PY)
Hazard ratio
p value
0.90
ns
1.00
ns
0.81
p=0.021
0.5
1.0
Hazard ratio
Favours ivabradine
1.5
Favours placebo
NYHA class changes
Patients (%)
68
70
70
p=0.0003
60
Ivabradine
50
Placebo
40
30
28
24
20
10
5
6
0
Improvement
Stability
Worsening
Incidence of selected adverse
events (N = 6492)
Patients with an event
Ivabradine
Placebo
p value
N=3232, % (n)
N=3260, % (n)
All serious adverse events
45% (1450)
48% (1553)
0.025
All adverse events
75% (2439)
74% (2423)
0.303
Heart failure
25% (804)
29% (937)
0.0005
Symptomatic bradycardia
5% (150)
1% (32)
<0.0001
Asymptomatic bradycardia
6% (184)
1% (48)
<0.0001
Atrial fibrillation
9% (306)
8% (251)
0.012
Phosphenes
3% (89)
1% (17)
<0.0001
Blurred vision
1% (17)
<1% (7)
0.042
Conclusion
Heart failure with systolic dysfunction and elevated heart rate
is associated with poor outcomes (primary composite endpoint
in the placebo group is 18%/year)
Ivabradine reduced CV mortality or heart failure hospitalization
by 18% (p<0.0001). The absolute risk reduction was 4.2%
This beneficial effect was mainly driven by a favourable effect
on heart failure death/hospital admission (RRR 26%)
Overall, treatment with ivabradine was safe and well tolerated
Clinical implications
The addition of ivabradine to recommended
therapy significantly reduces death and
hospitalisations related to heart failure in patients
with heart rate 70 bpm
The NNT for 1 year to prevent …
One primary endpoint is 26
One hospitalization for heart failure is 27
Available now online from Lancet
http://www.lancet.com published online August 29, 2010
DOI:10.1016/S0140-6736(10)61198-1
Acknowledgements
6505 patients from 37 countries
677 centres
More than 700 investigators and staff
Study supported by
Learn more about SHIFT on Monday 30 August
during the Clinical Trial Update II (14h13, Stockholm, Zone K)