LAB #14
advertisement

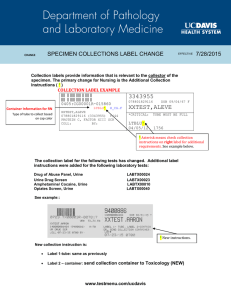
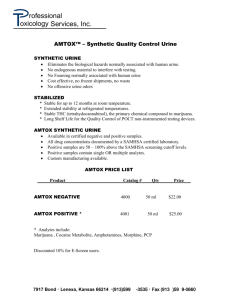
Biology 242 – Lab LAB #14 (14th/19 Lab Sessions for Winter Quarter, 2008) TOPICS TO BE COVERED: »Physiology of the Urinary System »Urinalysis »Recognition of Abnormal Findings on Microscopic Exam (Kodachrome slide series) DESIRED OUTCOMES: After completing the activities described for this lab session, students should: »Be able to define glomerular filtration, tubular reabsorption, and tubular secretion. »Be able to describe the normal physical characteristics of urine. »Recognize normal and abnormal urine constituents. »Know the steps of performing a Urinalysis: Gross, Biochemical, and Microscopic »Be able to describe how urinalysis reagent test strips (“dip sticks”) work. »Recognize a urine refractometer and explain its application and functioning. »Define several urinary conditions including utilizing proper, specific terminology. MATERIALS NEEDED: »500-ml urine cups w/lids »Refractometers »Canisters of Chem-Strip 9 reagent test strips »Urine centrifuge »BioHazard disposal container »Chart of Urinalysis: Microscopic Findings »15 ml urine test tubes w/lids »Grease pencils for labeling test-tubes »Yellow Urinalysis Form sheets »Set of Kodachrome Slides: Urinalysis Activity #1: Physiology of the Urinary System The kidneys maintain the chemical balance of body fluids by removing metabolic wastes, excess water, and electrolytes from the blood plasma. Three physiological processes occur in the nephrons to produce urine: glomerular filtration, tubular reabsorption, and tubular secretion. These processes occur rapidly, efficiently, and with huge volumes involved: the kidneys filter 25% of the body’s blood each minute, producing on average 125 ml/min of filtrate. Of the approximately 180 liters of filtrate that is formed by the glomeruli per day, 99% of this fluid is reabsorbed, but this eventually still results in the production of an average daily output of 1.8 liters of urine per day. The composition of urine can change on a daily basis depending on one’s metabolic rate and urinary output. Water accounts for about 95% of the volume of urine. The other 5% contains excess water-soluble vitamins, drugs, electrolytes, and nitrogenous wastes (urea, uric acid, creatinine). The yellow color is imparted by urochrome, a yellow, amorphous pigment molecule produced during the breakdown of hemoglobin. Here is a summary of the major steps in urine production: Step 1: Glomerular filtration produces a filtrate resembling blood plasma, but containing few plasma proteins. This filtrate has the same solute concentration as plasma or interstitial fluid. Step 2: In the proximal convoluted tubule, 60 – 70% of the water and almost ALL of the dissolved nutrients are reabsorbed. The osmolarity of the tubular fluid remains unchanged. Step 3: In the PCT and descending loop of Henle, water moves into the surrounding interstitial fluid (and eventually into the peritubular + vasa recta capillaries to be returned to the blood) , leaving a small fluid volume (roughly 20% of the original filtrate) of highly concentrated tubular fluid. BIOLOGY 251 – LAB #14 – continued Page Two Step 4: The ascending limb is impermeable to water and solutes. The tubular cells actively pump sodium and chloride ions out of the tubular fluid. Because only sodium and chloride ions are removed, urea now accounts for a higher proportion of the solutes in the tubular fluid. Step 5: The final composition and concentration of the tubular fluid are determined by the events under way in the DCT and the collecting ducts. These segments are impermeable to solutes, but ions can be actively transported into or out of the filtrate under the control of the hormones such as aldosterone. Step 6: The concentration of urine is controlled by variations in the water permeabilities of the DCT and the collecting ducts. These segments are impermeable to water unless exposed to antidiuretic hormone (ADH). In the absence of ADH, no water reabsorption occurs, and the individual produces a large volume of dilute urine. At high concentration of ADH, the collecting ducts become freely permeable to water, and the individual produces a small volume of highly concentrate urine. Activity #2: Urinalysis For hundreds of years, health care providers have recognized the utility of urinalysis as a diagnostic tool. Historically, the urine was evaluated for color, translucency, odor, and taste (yes: TASTE!!) Today, while these physical characteristics are still examined (except, thankfully, taste), we also utilize urinalysis reagent test strips to test for the presence of various chemicals in the urine. Abnormal readings, while not necessarily diagnostic of a specific condition, can give the provider a wealth of information about the state of a patient’s renal function and overall health. There are three main parts to the Urinalysis: I. Physical Observation of Urine Sample, II. Biochemical Evaluation of Urine Sample, and III. Microscopic Exam of Urine Sample. (These are noted on the yellow Urinalysis Form you will be given in Lab.) I. Physical Observations of Urine Sample Characteristic Volume Color Turbidity Specific gravity Other (ie: Odor) Observation ____________________________________________ ____________________________________________ ____________________________________________ ____________________________________________ ____________________________________________ ▪Volumes in excess of 2 liters (polyuria) or less than 500 ml per day (oligouria) are considered abnormal. A urine output of 50 ml per day or less is termed anuria. The volume of a single urine sample is variable depending on an individual’s hydration status and fluid intake. ▪The color of urine varies from clear to amber. Urochrome is a by-product of hemoglobin catabolism that gives urine its yellowish color. Color also varies because of ingested food. Vitamin supplements, certain drugs, and the amount of solutes also influence the urine’s color. A dark-red or brown color indicates blood in the urine. ▪Turbidity, or cloudiness, is related to the amount of solids in the urine. Contributing factors include bacteria, mucus, cell casts, crystals, and epithelial cells. To describe your observation of the turbidity of the urine sample, use descriptive words such as “clear”, “clouded”, “hazy”, and so on. ▪Specific gravity is the ratio of the weight of a volume of a substance to the weight of an equal volume of distilled water. The specific gravity of water is 1.000. Urine contains a given amount of solutes and solids which directly affect its specific gravity. The amount of fluids ingested affects the volume of urine excreted and therefore the amount of solutes and solids per given volume. A high fluid intake results in more frequent urination of a more dilute urine containing fewer solutes and solids per given volume and therefore leads to a lower BIOLOGY 251 – LAB #14 – continued Page Three specific gravity. A low fluid intake results in less frequent urination of a more concentrated urine with a higher specific gravity. Normal constituents of urine include water, urea, creatinine, the ions: sodium, chloride, potassium, sulfates, phosphates, and ammonium salts. Excessively concentrated urine results in the crystallization of solutes, usually salts, into insoluble stones called renal calculi or kidney stones. The average specific gravity for a random sample should fall between 1.001 and l.030. (You will be instructed as to how to use the instrument called the refractometer to measure your urine sample’s specific gravity.) ▪Freshly voided urine has no odor. As chemical breakdown of substances occurs, the sample hay acquire an ammonia odor. Odor serves a s a diagnostic tool for freshly voided urine. Starvation causes the body to break down fats and produce ketones that give urine a fruity or acetone-like smell. Individual with diabetes mellitus often produce sweet-smelling urine. To smell the sample, place it approximately 12 in. from your face and “wave” your hand over the sample toward your nose. II. Biochemical Evaluation of Urine Sample Substance Leukocytes pH Glucose Protein Ketones Nitrites Bilirubin Urobilinogen Erythrocytes Hemoglobin Remark(s) _______________________________________ _______________________________________ _______________________________________ _______________________________________ _______________________________________ _______________________________________ _______________________________________ _______________________________________ _______________________________________ _______________________________________ Dip sticks are a fast, inexpensive method of determining the chemical composition of urine. Chemstrips is a popular brand used for this test. These sticks contain nine testing squares and are used to give a very informative evaluation of the urine’s chemical content. 1. Dispense 15 ml of your urine sample into the Urine test tube; place the tube in the test-tube rack. 2. Swirl your sample in the test tube before introducing the Chemstrip. 3. Holding a Chemstrip by the end that does not have any test squares, immerse all the squares into the urine and then withdraw it. (Note: just a short exposure to the urine is sufficient; do NOT leave the Chemstrip in tube for a long time.) 4. lay the strip on a clean, dry paper towel to absorb any excess urine that may form droplets on the Chemstrip. 5. Reading of the tests varies from immediately to 2 minutes. Use the color chart grid on the canister to interpret the test results. 6. Record your data on the yellow Urinalysis Form. BE SURE to include UNITS where appropriate. ▪Leukocytes – White blood cells in the urine (pyuria) usually indicate an infection of the urinary tract. Problems can include cystitis, urethritis, or kidney infection. ▪The pH of normal urine ranges from 4.5 to 8.0. diet has a large effect on the pH of urine. High vegetable fiber diets result in a urine pH that tends to be alkaline; whereas, high protein diets result in an acidic pH. Be careful NOT to let urine from other squares drain onto the pH square, or false results may occur. ▪The presence of glucose in the urine, glucosuria, may indicate diabetes mellitus. This may also be the result of a very high-carbohydrate meal which produces a condition of glucose in the urine called temporary glucosuria. Production of epinephrine in response to stress results in the conversion of glycogen to glucose and its release from the liver. The elevated levels of glucose may then be secreted into the urine. ▪Usually the urine contains trace amount of proteins that may be too small for normal testing procedures to determine. Proteins are normally too large to pass through the endothelial-capsular membrane (aka: filtration membrane). Proteins in the urine, proteinuria, may occur as the result of increased blood pressure, increased BIOLOGY 251 – LAB #14 - continued Page Four permeability of the filtration membrane, or irritation of the tubules from bacterial toxins. Positive results are due to the presence of albumin, a plasma protein; when albumin is present in the urine, it is called albuminuria. ▪The presence of ketones in the urine (ketonuria as a result of ketoacidosis) may be the result of diabetes mellitus or a starvation diet, a very low carbohydrate diet, that causes the body to break down fats. ▪Nitrites in the urine indicate a possible urinary tract infection. ▪Bilirubin is a pigment in bile. When red blood cells are removed from the blood by the liver, the globin portion of the hemoglobin molecule is split off the molecule and the heme portion is converted to biliverdin. The bilibverdin is then converted to bilirubin which is a major pigment in bile. A high level of bilirubin in the urine is called bilirubinuria. ▪Urobilinogen is a by-product of the breakdown of bilirubin. Greater than trace levels in the urine may be due to infectious hepatitis, cirrhosis, congestive heart failure, or a variety of other diseases. ▪Erythrocytes and Hemoglobin – Erythrocytes (aka: Red blood cells) in the urine (hematuria) is usually an indication of an inflammation or infection of the urinary tract with leakage of blood into the urinary tract. Causes for red blood cells and hemoglobin in the urine can be a disease condition, irritation of the renal tubules from the formation of kidney stones, trauma such as a hard blow to the kidney, blood from menstrual flow, and possible tumor formation. Care should be taken in making sure the urine sample was not contaminated with menstrual blood from the vaginal area. When hemolysis of erythrocytes occurs, the hemoglobin molecules break down into their α and β polypeptide chains. These two chains are filtered by the kidneys and are excreted in the urine. If a large number of erythrocytes are being broken down in the circulation, the urine develops a dark-brown to reddish color. The presence of hemoglobin in the urine is called hemoglobinuria. III. Microscopic Examination of Urine Examination of the sediment of a centrifuged urine specimen reveals the solid components of the sample. This can be a valuable test to determine or confirm the presence of abnormal contents in the urine. A wide variety of solids occurs in urine including cells, casts, crystals, and mucus. 1. Cap your 15 ml test tube and, using the grease pencil, put your initials (or some distinguishing mark) on the cap. 2. Place your tube in the centrifuge opposite another tube so that the centrifuge remains in a balanced state. This step is very important for protection of the centrifuge. 3. Centrifuge the samples for 8 – 10 minutes. 4. At the sink, pour off the supernatant. At your workstation, use a Pasteur pipette to remove some of the sediment that has concentrated in the tapered bottom of the tube. Place one drop of this concentrated sediment on a microscope slide, and place a cover slip on top of the specimen. 5. Begin viewing the stained sediment under scanning power (10X). Look for epithelial cells, RBCs, WBCs, crystals, and microbes. A high number of bacteria usually indicates a urinary tract infection. Mucin threads and casts may also be see in the sediment. Mucin is a complex glycoprotein secreted by unicellular exocrine glands such as goblet cells. In water, mucin become mucus, a slimy coating that lubricates and protects the lining of the urinary tract. Casts are usually cylindrical and composed of proteins and cells. Crystals of the salts are also found in urine. Renal calculi or kidney stones consist of calcium oxalate, uric acid, and calcium phosphate crystals. They may form and lodge anywhere in the urinary tract and can cause intense pain. Compare the contents of your urine sample with the Figures on the charts made available in Lab today. 6. Dispose of all used paper towels and pipettes in the autoclave bag provided. Pour excess urine (in the collection cups and from the test tube) down the drain; then discard the cups and tubes into the BioHazard bag lined waste receptacle. Place glass microscope slides and cover slips in a beaker of 10% chlorine solultion. Perform an organized scan of your wet specimen and note presence of any significant findings on the yellow Urinalysis Form.