MLAB 1227: C K B -M
advertisement

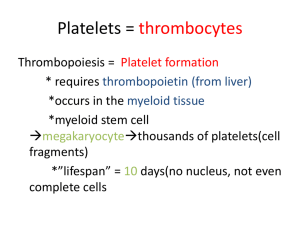
MLAB 1227: COAGULATION KERI BROPHY-MARTINEZ Overview of Hemostasis: Part Two FUNCTION OF Surveillance PLATELETS of blood vessel continuity Checks endothelial lining for gaps and breaks Fill-in small gaps caused by separation of endothelial cells Formation of primary hemostatic plug Surface for coagulation factors to make secondary hemostatic plug Aid in healing injured tissue FORMATION OF PRIMARY HEMOSTATIC PLUG Once the platelets “normal” environment is changed, they become activated or adhesive Stages of plug formation Adhesion Secretion Aggregation Stabilization STAGE 1: PLATELET ADHESION Platelets attach to non-platelet surfaces, such as collagen fibers in the subendothelium Platelets move from the blood vessels and into the tissues. Exposure to surfaces in the tissues causes them to bind Veins/venules- collagen Capillaries/arterioles- von Willebrand factor ( vWF) through the Glycoprotein Ib/IX receptor Results in a bridge formation, which triggers a shape change in the platelets Reversible No energy required PLATELET ACTIVATION Platelets undergo a shape change from disc to spiny sphere with projections Activation required for 1O hemostatic plug formation ++ Activation continues until Ca threshold met Platelets remain localized in injured area Key outcome- generate active GPllb/llla receptors to bind fibrinogen http://tiny.cc/abmhmw ACTIVATION Platelet shape change after exposure to agonist. Agonists include: ADP, Serotonin, collagen, thrombin STAGE 2: PLATELET SECRETION/ PLATELET RELEASE REACTION Secretion Requires ATP Provides a positive feedback by releasing more agonists to stimulate more plt receptors Release of Granule contents Causing vasoconstriction Release of ADP(agonist)= increased Ca+, plt release, increase in fibrinogen receptors Trigger a secondary aggregation which is irreversible WHAT’S IN A GRANULE? Granules consist mainly of: Alpha granules: Factor V, vWF, Fibrinogen, platelet factor 4, β-thromboglobulin Factor V: receptor on platelet surface for factor Xa & prothrombin PF4: heparin neutralizing factor, promotes wound healing Dense bodies: ATP, ADP, serotonin, Ca SIDE NOTE Heparin is used on patients who clot excessively. Endothelial cells make heparin-like molecules and expose them on their surface. PF4 binds these substances. Heparin can complex with bound PF4 and heparin will be neutralized. STAGE 3: PLATELET Chemical AGGREGATION changes cause platelets to aggregate and stick to one another Newly arriving platelets become activated by agonists Exposure of GPIIb/IIIa sites bind fibrinogen Fibrinogen + activated platelets serves as a bridge between two platelets Calcium must be present ADHESION & AGGREGATION http://www.platelet-research.org FINAL STAGE : STABILIZATION OF CLOT AKA: primary hemostatic plug formation Thrombus formation Platelets release Factor V Expose factor III (TF) Accelerating coagulation cascade Promote activation of clotting factors STAGES OF 1O PLUG FORMATION BLOOD CLOT COAGULATION SYSTEM Composed of 14 coagulation factors (serine proteases) which are interdependent (Factors I through XIII – there is no Factor VI – and PK and HMWK) ◦ ◦ ◦ ◦ Final product is fibrin mesh or clot which completely stops bleeding ◦ Inactive form of each is an enzyme precursor which is usually designated by a Roman numeral but also given a name – Ex. Factor I fibrinogen. Numbers correspond to order of discovery NOT order in cascade. Active forms are usually designated by the letter “a” after the Roman numeral and may also have a different name – Ex. Ia Fibrin Cofactors are needed for many reactions in the cascade – Ex. Calcium, platelet factor 3 (PF3) Each molecule must be present in sufficient quantity as well as functioning normally Secondary hemostasis Slow contraction or retraction and lysis of the clot occurs FIBRINOLYTIC SYSTEM Fibrin is a product formed during hemostasis, tissue repair or inflammation Fibrin plays a temporary role Once injury heals, the fibrin clot is lysed Plasminogen is converted to plasmin Plasmin enzymatically attacks the fibrin molecule producing fibrin degradation products (FDPs, sometimes called FSPs) that are cleared from the circulation by macrophages COAGULATION INHIBITION SYSTEM Provides balance and control of clotting mechanisms Natural inhibitors and anticoagulants circulate in the plasma to: Prevent clotting when it’s not needed Limit or localize the clotting that is needed Examples: Protein C and S, antithrombin III REFERENCES McKenzie, Shirlyn B., and J. Lynne. Williams. "Chapter 29." Clinical Laboratory Hematology. Boston: Pearson, 2010. Print. Platelet Research Laboratories. Platelet Function. Retrieved from http://www.plateletresearch.org/1/function_hemo.htm.