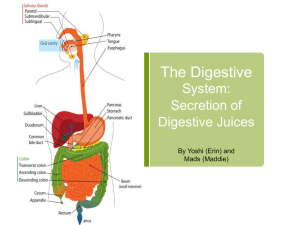
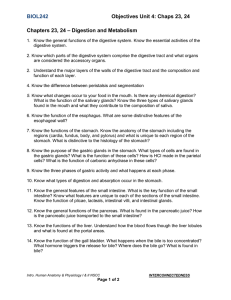
— The Digestive Chapter 25 System 25-1
advertisement

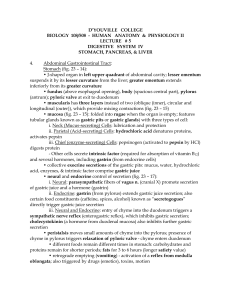
Chapter 25— The Digestive System 25-1 Ch. 25 Study Guide 1. Critically read 25.3 (stomach), 25.4 (liver, gallbladder, and pancreas), 25.5 (small intestine); pp. 977-995 2. Comprehend Terminology (those in bold) 3. Study-- Figure questions, Think About It questions, and Before You Go On (sectionending) questions 4. Do end-of-chapter questions: – Testing Your Recall— 1-4, 6, 9, 10, 15-17 – True or False– 1, 3-10 – Testing Your Comprehension– 2, 5 25-2 I. Stomach (25.3)— A. Introduction and gross anatomy 25-3 § Introduction-- the stomach 1. Location/size-– Upper left abdominal cavity— – Volume– 50 mL when empty and 1-2 L after a typical meal. 2. Functions– – Primarily as a food ____________ organ – Liquefies the food and begins the chemical digestion of proteins and fat – End result: Chyme– 25-4 § Gross Anatomy (stomach) 1. Lesser curvature— 2. Greater curvature— 3. Four regions— Fig. 25.12 a-b A. Cardiac region (cardia)– inside the cardiac orifice B. Fundic region (fundus)— C. Body (corpus)– inferior to the cardiac orifice; greatest part of the organ D. Pyroric region– narrower pouch at the inferior; subdivided into antrum and pyloric canal 25-5 25-6 Figure 25.12b 25-7 I. Stomach— B. Cell types and their secretions 25-8 § The stomach wall • Structures from the outermost layer: 1. Three muscle layers– muscularis externa 2. Gastric rugae– Wrinkles formed by mucosa and submucosa 3. Gastric pits– depressions in mucosa • Lined with ____________ epithelium • Tubular glands (cardiac, pyloric, and gastric glands) open into the pits • Cell types– Addressed shortly . . . • Fig. 25.13 a-b 25-9 Gastric/pyloric glands of the gastric pits (next slide) 25-10 Tubular glands differ depending on areas. 2 § Cell types of the tubular glands 1. Mucous cells– secrete mucus, predominate in the cardiac and pyloric glands 2. Regenerative (stem) cells– in the base of the pit and neck of the gland; function— 3. Parietal cells– mostly in the upper half of the gastric gland; secrete hydrochloric acid and intrinsic factor 4. Chief cells– most numerous and only in gastric glands; secrete chymosin and lipase in infancy; _________________ later on 5. Enteroendocrine cells– G cells included 25-12 § Gastric secretions--HCl • 2-3 L of gastric juice per day--mainly water, HCl, and pepsin 1. HCl – by parietal cells: Fig. 25.14 - – CO2 + water (CAH) H2CO3 HCO3 + H+ – Chloride shift--HCO3 exchanges for chloride ions (Cl ) from the blood plasma – Alkaline tide– during digestion, high-pH blood 2. Functions of HCl: – Activates enzymes— – Kills ingested bacteria – Converts Fe(3+) to Fe(2+) 25-13 Chloride shift CAH 25-14 § Gastric secretions— Intrinsic factor 1. Secreted by-- parietal cells 2. Chemistry--Glycoprotein 3. Function– essential to the absorption of ______________ by the small intestine 4. Disorder– pernicious anemia 5. Treatment– injection of vitamin B12 or take vitamin B12 and intrinsic factor orally 25-15 § Gastric secretions--Pepsin 1. Chief cells secrete a zymogens (inactive proteins) called pepsinogen 2. Pepsinogen pepsin (by HCl) 3. Functions of the pepsin— A. Digests proteins: B. Autocatalytic effect of pepsin: – Once pepsin is formed, pepsin can converts pepsinogen into MORE pepsin. Fig. 25.15 25-16 Pepsin has two functions #1 and #2 below (as shown); HCl has function #3 What are functions 1-3, respectively? 25-17 § Gastric digestion and absorption 1. Digestion— – Partially digest protein, starch, and fat – Most digestion and absorption occurs in the ________________ 2. Absorption— – Not significant amount – Absorb aspirin, some lipid-soluble drugs, and little alcohol 25-18 I. Stomach— C. Protection of the stomach 25-19 § protection of the stomach • 3 ways to protect against harsh acidic and enzymatic environment (Fig. x) 1. Mucous coat– thick, and alkaline mucus 2. Epithelial cell replacement– cells live 3-6 days; replaced by new cells in the gastric pits 3. ____________ — prevents gastric juice from seeping between them to damage CT of the lamina propria or beyond 25-20 Mucus coating LUMEN Passage prevented Impermeable to HCI Tight junction Cells lining gastric mucosa (including those lining gastric pits and glands) Submucosa 25-21 § peptic ulcer 1. Definition– erosion in the wall of digestive tract caused by pepsin and HCl 2. Locations– duodenum most common, also in _______________________ 3. Causes– mucosal defense is compromised; hypersecretion of acid/pepsin, Helicobacter pylori (bacterium), smoking, use of aspirin 4. Treatments-- Cimetidine (H2 blocker on parietal cells); antibiotics against Helicobacter (better) Fig. 25.16 a-b 25-22 Normal Peptic ulcer 25-23 I. Stomach— D. Regulation of the gastric function 25-24 § Regulation of Gastric function • Three phases— overlap each other and all three can occur simultaneously 1. Cephalic phase– being controlled by the brain 2. Gastric phase– being controlled by the stomach 3. Intestinal phase– being controlled by the small intestine 25-25 § Regulation of Gastric function • The cephalic phase– the stomach responds to sight, smell, taste, or thought of food. • Details– A. mental inputs converge on the hypothalamus, to the medulla oblongata B. vagus nerve fibers from medulla innervate the stomach to stimulate gastric activity. • Fig. 25.17 25-26 25-27 § Regulation of Gastric function • The gastric phase– swallowed food activate gastric activity Details– Presence of food/proteins A. Stretching– via a long vagovagal reflex and a short myenteric reflex B. Through chemicals—Ach, gastrin, histamin – On parietal cells (by Ach, gastrin, histamin)- to secrete HCl – On chief cells (by Ach and gastrin)– pepsinogen – Digested protein: stimulates the G cells secrete even more gastrin Fig. 25.17 b and 25.18 25-28 & Ach 25-29 Fig. 25.18– Feedback control of gastric secretion. (+ feedback) 25-30 § Regulation of Gastric function • The intestinal– duodenum responds to _______ and moderates gastric activity Details– • Initially enhances gastric secretion • Soon, acid and semidigested fats trigger the enterogastric reflex– to: – Inhibit vagal nuclei – Stimulate sympathetic neurons – Secretin and cholecystokinin inhibit gastric activity Fig. 25.17c 25-31 _ 25-32 II. 25.4— A. The liver 25-33 § Gross anatomy Location– inferior to the diaphragm … The body’s largest organ— Functions– Fig. x Four lobes— right, left, quadrate, and caudate lobes 5. Other important terminology– falciform ligament, round ligament; bare area, porta hepatis Fig. 25.19 1. 2. 3. 4. 25-34 PROD. & 25-35 25-36 § Microscopic anatomy 1. Lots tiny cylinders– hepatic lobules (each 2mm x 1mm) – Each hepatic lobule– central vein + radiating hepatic sinusoids + sheets of hepatocytes – Functions of hepatocytes and hepatic macrophages-- Fig. 25.20 a, c 25-37 Fig. 25.20a--The hepatic lobules Hepatic sinusoid Central vein Hepatic triad: 1-Branch of hepatic portal v. Stroma 2-Branch of Hepatic a. 3-Bile ductule (a) Bile canaliculi Hepatocytes 25-38 Hepatic macrophage Hepatocyte Endothelial cells Fenestration Sinusoid 25-39 § Microscopic anatomy 2. Stroma (C.T.)-- Among hepatic lobules – Hepatic triad– two blood vessels and a bile ductule – Blood circulation in the liver– blood vessels of a triad to the sinusoids, to the central vein, to right and left hepatic veins and to the _____________ before going back to the heart 25-40 § Bile 1. Color– yellow-green fluid 2. Secreted by— the liver; @ 1 liter per day 3. Components— bile acids, cholesterol, – – – – phospholipids (lecithin), neutral fats, minerals, bile pigments (major pigment is bilirubin) Bile acids (steroids) and lecithin aid in fat digestion and absorption _____% of bile acids are reabsorbed in the ileum and reused (called enterohepatic circulation) All others are wastes, destined in the feces Waste products too concentrated-- gallstones 25-41 II. 25.4— B. The gallbladder 25-42 § Gallbladder and bile flow 1. Gallbladder– (Fig. 25.21) – Location– on the underside of the liver – Dimension– 10 cm long – Pathway-- Its neck (cervix) leads into the ________ duct, which then joins the bile duct – Function– store and concentrate bile 25-43 1. Hepatic ducts Gallbladder: 3. Cystic duct Neck Body 2. Common hepatic duct 4. Bile duct Head Accessory pancreatic duct Pancreatic duct Duodenum Minor duodenal papilla 6. Hepatopancreatic sphincter 7. Major duodenal papilla 5. Hepatopancreatic ampulla Pancreas Duodenojejunal flexure Jejunum 25-44 § Gallbladder and bile flow 3. Bile’s pathway– (see also Fig. 25.21) – Bile canaliculi (between layers of hepatocytes) – Small bile ductules of the triads – – – – – Right and left hepatic ducts, converge to form The common hepatic duct Joins the cystic duct (of the gallbladder) Forms the bile duct Joins the pancreatic duct to become the hepatopancreatic ampulla – Terminates at the major duodenal papilla 25-45 II. 25.4— C. The pancreas 25-46 § The pancreas 1. Location– anterior/posterior (circle one) to the greater curvature of the stomach 2. Dimension– 12-15 cm long & 2.5 cm thick 3. Functions– both endocrine (1%; insulin + glucagon) and exocrine gland (99%; secretes pancreatic juice) – Pancreatic juice: alkaline mixture of water, enzymes, zymogens, sodium bicarbonate, ions – Path of pancreatic juice: through either main or accessory pancreatic ducts 25-47 § The exocrine secretions of the pancreas 1. Zymogens– trypsinogen, chymotrypsinogen, and procarboxypeptidase (all digest proteins) – Trypsinogen becomes ________ by enterokinase (from small intestine); an autocatalytic reac. – Trypsin also convert the other two zymogens into active forms 2. Other enzymes-- become fully active upon exposure to bile or ions in the intestines – What are they? Fig. 25.23 25-48 25-49 § Regulation of pancreatic secretion 1. Acetylcholine– (from vagus and enteric nerves in response to gastric phases); stimulates enzymes secretion and release 2. Cholecystokinin– (from duodenum and jejunum in response to fats); stimulates— – Discharge of bile into the duodenum – the secretion of pancreatic enzymes 3. Secretin– (same as #2; in response to acidity of chyme); stimulates the secretion of sodium bicarbonate from _____ 25-50