Document 15957538
advertisement
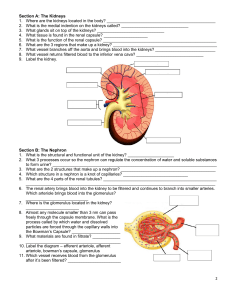
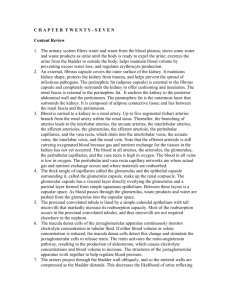
A. The general function of the urinary system is to maintain homeostasis by balancing the volume and chemical make up of the blood (thus Kidney has long term control of blood pressure) and elimination of wastes [toxins, nitrogenous wastes, and excess ions] 1. Kidneys 2. Ureters 3. Urinary Bladder 4. Urethra Long paired muscular tubes that drain each kidney and propel urine by peristalsis into the urinary bladder. Stretchy storage unit for urine, contracts to empty Urine exits body thru urethra, a narrow tube about 1.5 inches in females and 8 inches in males a. Collection and storage area for urine. b. Collapsed when empty. c. Longitudinal & circular smooth muscle d. Transitional epithelial tissue e. Internal sphincter and external sphincter 1. Located in lower back T12-L3, just under 12th rib 2. 7 lobes 3. Three layers of supportive tissue (renal capsule, adipose capsule, fibrous capsule) 4. Parts of K are cortex, medulla w/ Calyces (pyramids), renal pelvis, renal sinus and hilus Need to know (1) Juxtamedullary (2) Cortical Nephron c. Bowman’s capsule, Efferent Arteriole connects to Peritular Capillaries d. Filtration membrane in glomerulus (1) Pressure within Glomerulus produces filtrate (ions, glucose, water, amino acids) (2) 2 highly permeable membranes due to fenestrations, podacytes & thin basement membranes in glomerulus • Layer 1 is gomerular fenestrations of glomerular capillaries • Layer 2 is fusion of glomerlular & renal capsule basement membranes • Layer 3, the podacyte is visceral layer of renal capsule, has slit diaphragms (filter) between podacytes. Filtrate enters Bowman’s capsular space e. Cell types in nephron (how kidney works) (1) PCT cubodial epithelium w/ microvilli. Absorption from PCT to peritubular capill. (2) Loop of henle, thin segment is simple squamous for osmosis of H20 out and into blood; water follows Na+ from left side loop. (3) Collecting ducts are cuboidal/columnar w/ aquaporins inserted when ADH for [urine] (4) DCT lumen is ridged. M/B is enfolded, for secretion movement from blood to DCT(pH). (5) JG cells (JGA) BP sensors in arterioles, smooth muscle cells control diameter of As (6) Macula densa (JGA), chemoreceptors in DCT promote dilation or constriction of afferent Arteriole, as Renin is released eA is constricted, as are other BV of body = rise in BP. (7) Peritubular capillaries arise from efferent arteriole and surround PCT and other tubules, but are called vasa recta when long loops of henle dip down into medulla in juxtamedullary nephrons. (F) is removal of H2O which follows Na+ = [urine] f. Histology of kidney Tubules, PCT & DCT (no microvilli) Shows collecting duct Cortex of Kidney Pyramids and Renal Pelvis End of story: the Liquid that remains in tubules , leading to Collecting ducts = excess water and ions, waste & toxins is sterile Whooda guessed?