Reproduction & Development I. Background/Reminder Information
advertisement

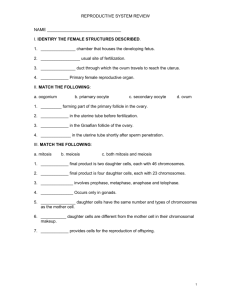
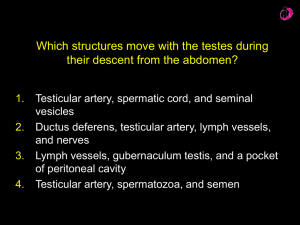
Reproduction & Development I. Background/Reminder Information Human somatic cells have 23 pairs of chromosomes. Chromosomes are pieces of DNA with specific genes on them. For example, maybe a gene that codes for eye color is located on chromosome 5. In every human's DNA, that eye color gene will be located in the same spot on chromosome 5. There are different variants of genes called alleles; for example, this gene that codes for eye color might have two different alleles: brown and blue. Which variant/s you ended up with depends on what you inherited from your mom & dad. Which brings me to the next point: your cells' nuclei have two of each chromosome number... two of chromosome 5, for example. That's because you got a copy from mom and a copy from dad. So, if mom gave you the blue variant and dad gave you the brown variant, you'd have one of each allele for the eye color gene at chromosome 5. So, your cells' nuclei each have 46 chromosomes because they have 23 pairs of chromosomes. When you have offspring, you will donate ONE chromosome from each of your chromosome pairs. For example, if you have the blue allele from mom's chromosome 5 eye color gene and the brown allele from dad's chromosome 5 eye color gene, you can only pass one of them on to your offspring. So you will pass on a total of 23 unpaired chromosomes to your offspring, and the other 23 will come from your mate. If you are a female, those 23 unpaired chromosomes will be held in an egg. If you are a male, they will be held in a sperm. Egg and sperm (gametes) have half of the genetic material of somatic cells, and they have one copy of every gene and chromosome (instead of two copies). The process of meiosis produces gametes (what do we call cell division of somatic cells?). An overview of meiosis: A cell with the full suite of 23 chromosome pairs makes a copy of each chromosome. Now the cell has 2 identical copies of each of mom's chromosomes and 2 identical copies of each of dad's chromosomes. That means there are now four copies of each chromosome (2 of mom's, 2 of dad's). The cell divides, creating 2 daughter cells with 2 copies of each chromosome. Each of those daughter cells divides, and the outcome is 4 separate cells with one copy of each chromosome. Each gamete is genetically unique, because before all the divisions, some of mom's and dad's genes swapped alleles ("crossing over"). Also, each gamete got a mixture of mom's chromosomes and dad's ("independent assortment"). So, for example, maybe one gamete got chromosome #5 from mom but chromosome #7 from dad. Anyway, now you have 4 genetically unique gametes with 23 unpaired chromosomes. If you are a male, one of your lucky sperm will donate those chromosomes to an egg, who has the matching 23. The result will be a cell with 23 pairs of chromosomes, and it will start to divide and become your offspring. Somatic cells are called diploid, because they have 2 of each chromosome. Gametes are called haploid, because they have 1 of each. (PS, a real example is the beta-Hemoglobin gene, which is on Chromosome 11) Males II. Spermatogenesis- making sperm. This occurs in the seminiferous tubules, beginning around age 14 and continuing throughout the life of a male. Immature sperm are sent to the epididymis for "finishing" and storage, then to the ductus deferens for storage. >A. Early spermatogenesis: Undifferentiated stem cells (spermatogonia) line the outer portion of the seminiferous tubules. The replicate by mitosis, sending one of the daughter cells up toward the lumen of the tubule. As the daughter cell migrates toward the lumen, it undergoes meiosis to produce 4 immature sperm. >B. Sperm differentiation/maturation: spermiogenesis. Each of the immature sperm will spend the next few weeks maturing and specializing into lean, mean, swimming machines. During this time, excess cytoplasm will be shed. The nucleus condenses. An acrosomal vessicle (similar to a lysosome) becomes a specialized, enzyme-filled structure (acrosome) that will rest "above" the nucleus. The head of a sperm is composed of the acrosome and the nucleus. The significance of the enzymes will be revealed when we consider fertilization. Microtubules lengthen away from the head, pushing the cytoplasm out and becoming a flagellum, which is called the tail. Mitochondria gather around the microtubules at the base of the nucleus. This area of mitochondria is called the midpiece. All other structures are shed. The spermatozoan is pushed to the epididymis and then to the ductus deferens. It will be immobile until it is ejected and mixes with seminal secretions. Until then, it will be suspended in a nutrient-rich fluid of the ductus deferens. >C. Sustentacular cells-In the seminiferous tubules, aid the development of sperm. How? Among other things: >>Maintain a blood-testis barrier (which cells do this in the brain?)- Why on Earth? To make sure the right concentration of hormones, nutrients, etc. is maintained to support spermatogenesis & spermiogenesis AND to protect the genetically unique sperm (with unique antigens) from WBC! >>Stimulate spermatogenesis and spermiogenesis under the influence of testosterone and FSH >>Provide nutrition to the developing sperm >> Dispose of sloughed cytoplasm >>Secrete inhibin when sperm production rates increase. Inhibin is a hormone that inhibits the release of FSH (see below). So, sustentacular cells play a role in regulating the rate of sperm production. >D. Hormones >>1. The Gn-RH --> FSH, LH--> Testosterone system GnRH is secreted from the hypothalamus. It travels to the adenohypophysis (how does it get there?). GnRH stimulates the release of FSH and LH from the adenohypophysis. >FSH- Stimulates sustentacular cells (therefore spermatogenesis and spermiogenesis) >LH- Stimulates the release of androgens (testosterone) from a population of endocrine cells in the testes, interstitial cells >>Testosterone- stimulates sustentacular cells (therefore spermatogenesis and spermiogenesis) (We know testosterone also has other effects, like the maintenance of secondary sexual characteristics) >>2. Inhibin- secreted by sustentacular cells when sperm production is very high. Inhibits FSH secretion, perhaps by inhibiting GnRH secretion. >H. Sending sperm on its way: Male glands & Semen- during ejaculation, sperm that have been stored in the ductus deferens are propelled into the urethra. At the same time, the bulbourethral gland, seminal vessicles and prostate gland release secretions. Each gland secretes different products. Together, semen is composed of: HCO3-, fructose (feeds the sperm), prostaglandins (encourages uterine contractions to help sperm along), antibiotics, and mucous. Females III. OogenesisUnlike males, females make all of their eggs before they are born. The eggs are stored in the ovaries, and each month one egg (occasionally two) gets picked for possible fertilization. >A. Before a female is born, stem cells ("oogonia") in her developing ovaries produce daughter cells by mitosis. The daughter cells ("primary oocytes") begin meiosis. However, they do not complete meiosis. In these cells, each chromosome is copied, and the chromosomes start to organize themselves as if they were about to undergo meiosis. Then they stop, and remain in a state of "arrested development" until puberty. About 2 million primary oocytes are produced before birth. As you grow toward puberty, most will degenerate. By the time you hit puberty and start to let some of them continue meiosis, there are about 400,000 left. They are stored in the ovaries in the "egg nest." >B. Once a female hits puberty, one of the primary oocytes will be chosen each month to be available for fertilization. When a primary oocyte is chosen, it will resume meiosis. Recall that this primary oocyte had stopped meiosis before birth. Now that it's been picked, it will begin where it left off. Recall that meiosis includes two episodes of cell division, so that 4 gametes are produced. Once the primary oocyte is picked, it will undergo the first division. When the cell divides, however, virtually all the cytoplasm gets hogged by one of the daughter cells, so we get one huge cell and one tiny cell. The huge cell will go on to be the oocyte, or egg. The tiny cell is called a polar body, and degenerates. The runts always get the short end of the stick, don't they! During this time, the oocyte is travelling in the ovary, escorted by a group of cells called follicle cells. When it is ready, it will be ejected from the ovary into the fallopian (uterine) tube. If sperm are in the fallopian tube, this is where fertilization will occur. Only if fertilization occurs will the oocyte complete meiosis. Again, in this final division a polar body is produced and degenerates. We'll consider what happens when fertilization doesn't occur next. IV. Ovarian and Uterine Cycles- Describes what's going on in the ovaries and uterus when. The activities of the ovaries and uterus are coordinated, and they run in cycles of about 28 days. We will consider them separately, but keep in mind that the events of the ovaries and uterus are simultaneous and coordinated. >A. Ovarian cycle- Events in the ovary (use Fig. 28-16 and 28-26a-d to follow along) >>1. Follicular Phase- Day 1-14 A primary oocyte is chosen from the egg nest. When this occurs, cells surrounding the oocyte begin to divide. The daughter cells surround the oocyte with a sphere-like structure of cells called the follicle. These follicular cells will direct the maturation of the oocyte, and make sure that the uterus is prepared for pregnancy should this oocyte get fertilized. FSH is the dominant pituitary hormone of the Follicular Phase, and directs the development of the follicle. The follicle cells: >>>a. produce a thick layer of glycoproteins around the oocyte. This covering of glycoproteins is called the Zona Pellucida. >>>b. produce estrogen, which is released into the blood. Estrogen encourages the uterus to build a nice thick uterine wall. >>>c. secrete a fluid into the interior of the follicle, so that the follicle cells make up the outer "wall" of the sphere, and the sphere is filled with fluid. The oocyte gets pushed to one side of the interior sphere, with a thin layer of cells around it. Imagine that you have a balloon. The walls of the balloon represent the outer follicle cells of the follicle. Now, take a marble, put it inside the balloon and tape it to the interior wall of the balloon (easier if you have the fingers of a stick figure). The marble represents the oocyte, and the tape represents the layer of cells surrounding the oocyte. Now fill the balloon with water, and viola! you have a fake follicle or a really painful water balloon fight ahead of you. The fluid-filled cavity of the follicle is called the antrum, and the cells surrounding the oocyte are collectively referred to as the corona radiata. What's the point? Well, once the oocyte is mature and the follicle is ready, the follicle will bulge against the side of the ovary adjacent to the fallopian tube. It will then open up and expel the oocyte, complete with fluid and corona radiata, into the fallopian tube. This is ovulation, day 14 and the end of the follicular phase. >>2. Luteal Phase- Days 14-28. LH is the dominant pituitary hormone of the Luteal Phase. After expelling the oocyte and corona radiata, the remaining follicle cells expand and form a temporary endocrine gland, the Corpus Luteum. As we shall see in the Uterine cycle, these follicle cells are still looking after the oocyte! What great nannies! The Corpus Luteum secretes progesterone and some estrogen, which will prepare the uterus for pregnancy (we'll see how soon). If no pregnancy occurs, the Corpus Luteum starts to degenerate about 10-14 days later. The cycle is complete! >B. Uterine (Menstrus) Cycle- Events in the uterus(use Figs. 28-20 and 28-26 to follow along) There are three phases: >Phase 1: "Menses" Day 1-7 Uterine Wall Shed >Phase 2: "Proliferative" Day 7-14 Uterine Wall Rebuilt >Phase 3: "Secretory" Day 14-28 Uterus prepares for pregnancy *Let's start with Phase 3, Day 14, the day the oocyte was released into the fallopian tube. >>1. Secretory Phase- the beginning of this phase corresponds with ovulation, Day 14. If sperm enter the fallopian tube while the oocyte is making its way down to the uterus, the oocyte could be fertilized. If so, the uterus needs to be prepared to support a developing embryo. Remember that after ovulation, the follicle cells remaining in the ovary become a Corpus Luteum and secrete progesterone. Progesterone from the CL encourages the uterus to prepare in case the newly released oocyte is fertilized. The walls of the uterus get very thick, and uterine gland cells secrete a nutritious "soup" into the uterus. Growth of blood vessels into the wall of the uterus is supported. Why? Well, if the oocyte is fertilized, the embryo will get nutrients from this "soup" for a while, and will burrow itself into the wall of the uterus. If the oocyte is not fertilized, the CL will degenerate, progesterone levels will drop, and uterine growth/secretion will decline (dramatic drop around Day 28). Thus will begin... >>2. Menses- This begins on Day 1, the day a new primary oocyte is fledged from the egg nest of the ovary. In the uterine walls, the arteries are tightly constricted. The outer layer of uterine wall is deprived of O2 and dies. It is sloughed off. In the process, underlying blood vessels are exposed and bleed into the uterus. Menses lasts until about Day 7. >>3. Proliferation Phase Remember that during Day 1-7, while the uterine lining has been shedding, a follicle has been developing in the ovary and producing more and more estrogen. Around Day 7, estrogen levels have increased enough to end menses and support the rebuilding of the uterine wall. The proliferation phase lasts until about Day 14. At this time, the uterine wall is sufficiently rebuilt. The new oocyte will be released into the fallopian tube, and a new Corpus Luteum will start producing progesterone and thus begin the Secretory Phase. >C. Hormones >>GnRH from the hypothalamus is released on Day 1 and its release increases in frequency through Day 14, when it spikes. >>GnRH, as you know, stimulates the release of FSH and LH. Like GnRH, FSH and LH spike around Day 14, the day the oocyte is released into the fallopian tube. The spike in FSH and LH is thought to cause rupturing of the follicle (ovulation). >>FSH stimulates follicle development. The follicle secretes estrogen. >>>Estrogen supports rebuilding of the uterine wall. >>LH stimulates the formation of the Corpus Luteum. The Corpus Luteum secretes progesterone. >>>Progesterone supports secretion by uterine glands. It also inhibits GnRH release, which drops way down during the secretory phase. Because of this drop, FSH and LH also drop. The drop in LH causes the Corpus Luteum to eventually deteriorate (full deterioration by Day 28). But, if the oocyte is fertilized, the embryo will secrete an LH-mimick. This will keep the Corpus Luteum in tact, and progesterone levels will stay elevated so the uterus will continue to make the nutrient soup for the developing embryo. Eventually, the embryo will make connections with mom's blood vessels, and the soup will no longer be needed.