Digestive System Chapter 24
advertisement

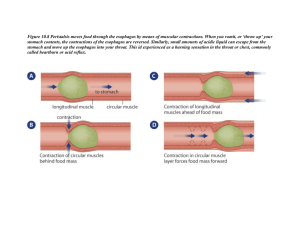
Chapter 24 Digestive System Digestive Tract top to bottom Buccal cavity - between teeth and cheeks Oral cavity - inside the arch of teeth Fauces - opening of oral cavity into pharynx Pharynx - ‘throat’ … in particular the oropharynx Esophagus - muscular tube leading from pharynx to stomach Digestive tract... Stomach Small Intestine (3 regions) duodenum jejunum ileum Large Intestine colon rectum anus Accessory Digestive Glands Salivary - moisten & lubricate food, begin digestion of carbohydrates Liver - secretes bile for emulsifying fat (bile stored in gall bladder (g.b. not actually a gland, no secretions of its own ) Pancreas - production of several digestive enzymes which are secreted into duodenum Wall of Digestive Tract (a generalized description) • Serosa - outer layer of connective tissue surrounding the gut • Muscularis - smooth muscle layers arranged both circularly and longitudinally • Submucosa - thick connective tissue layer with glands, blood vessels, nerves and other components • Mucosa - innermost layer - lined with stratified squamous or simple columnar epithelium (mucous epithelium), a loose connective tissue layer (lamina propria) and a thin layer of muscle (muscularis) Beginning Digestion Ingestion - taking in food, usually by mouth Mastication - chewing. Tearing, crushing food with teeth Deglutition - swallowing… a single lump of food is referred to as a bolus Muscular Movement of Food Propulsion of food through the digestive system occurs by regular, pulse-like muscle contractions called peristalsis Mixing/Grinding muscle contractions occur in stomach these are referred to as segmental contractions Rugae - muscular ridges in the wall of the stomach help with the grinding process But first... Mastication - chewing of food with teeth Humans are diphytodont (2 sets of teeth) 32 adult teeth & 20 deciduous (baby) teeth Heterodont - different types of teeth specialized for different tasks Crown (outer layer) of enamel, hardest material in body Dentin - layer chemically similar to bone but no internal cells Pulp cavity - containing blood vessels & nerves Salivary Glands 3 pairs Secretory cells can be either serous (watery secretion) rich in digestive enzymes (amylase) or mucous (mucoid secretion) for lubrication Parotid -located in front of the ear, serous glands producing primarily serous saliva. Duct opens near upper M2 Submandibular - located under the jaw these glands are roughly equal serous & mucous. Duct under tongue near frenulum. Gleek! Sublingual - located under tongue, mixed but primarily mucous secretion. No obvious duct, rather several openings Digestion begins Chemical breakdown of carbohydrates begins in the mouth with the enzyme Salivary Amylase Food travels down esophagus below the laryngopharynx carried along by peristalsis Entry into esophagus controlled by upper esophageal sphincter Lower esophageal sphincter (cardiac sphincter) at connection of esophagus to stomach keeps digestive juices of the stomach from reaching into the esophagus Histology of Esophagus Lining - stratified squamous epithelium - multi-layered because this takes a lot of wear & tear, lots of swallowing & some assault from gastric juices at lower end. Thick muscularis mucosa to propel food by peristalsis You can actually swallow food while standing on your head TAA - tell Wally Schirra’s astronaut & martini story Anatomy of Stomach 4 major regions Cardiac portion - where esophagus enters Fundus - enlarged swelling at upper end (above cardiac region) Body below the funds, makes up about 1/2 of the total area Pyloric region - the funnel shaped lower end where the stomach joins the duodenum (first part of small intestine) Pyloric Sphincter - ring of muscle at the base of the pylorus regulates the flow of material out of the stomach Stomach Lined with simple columnar epithelium (this lining continues for the remainder of the digestive tract) Tunica Muscularis arranged in 3 layers: Longitudinal layer – outermost layer Circular layer – middle layer Oblique layer – innermost layer Circular layer also forms a sphincter at the lower end of the stomach: Pyloric Sphincter – regulates flow of food out of stomach Digestion Carbohydrate digestion, which began in mouth (salivary amylase) is temporarily halted in stomach Protein digestion begins in stomach Food mixes with gastric juices to form chyme Stomach Mucosa Surface of mucosa (internal lining of stomach) arranged in gastric pits Gastric pits contain: Mucous cells – produce mucous (protective) Enteroendrocrine cells – produce hormone gastrin (regulate) Parietal Cells – secrete hydrochloric acid (HCl) Chief Cells – secrete pepsinogen Activation of pepsin for protein digestion Parietal cells Chief cells HCl Pepsinogen Q: Why not secrete active pepsin? A: It would digest stomach lining if it had nothing else to work on! Pepsin digestion of proteins Movie Break Ulcers! Small Intestine Histology of Duodenum (fig 24.11) four tunics: serosa, muscularis, submucosa & mucosa (out to in) Mucosal lining arranged in circular folds (increases surface area) Inner mucosa is lined with villi – finger-like projections Villi (singular = villus) – contain lacteal of lymphatic system for absorption of fat. Also contain capillary network Surface of villi further divided into microvilli which further increase surface area forming a brush border Cell types in Duodenal Mucosa & Submucosa Absorptive Cells – produce digestive enzymes & absorb nutrients Goblet Cells – produce mucous (protective) Granular Cells – immune response to bacteria? Endocrine Cells – produce hormones that regulate digestion Crypts of Lieberkühn – site where above cell types originate Submucosa contains mucous glands called Brunner’s Glands (duodenal glands) which secrete a mucous that helps lubricate food bolus Jejunum & ileum Fewer Brunner’s Glands (mucous accini) – why? These two sections are major sites of absorption Lymph nodules called Peyer’s Patches numerous in mucosa & submucosa of ileum Overall structure similar to duodenum but a gradual narrowing is seen Ileocecal junction – connection between ileum & large intestine = ring of smooth muscle (sphincter) Colon (large intestine) Divisions of colon: Ascending – up right side of abdomen Transverse – across top of abdomen R L Descending – down left side Sigmoid – over to center and down to rectum Rectum & anus – storage of feces & exit Colon/Rectum Longitudinal muscle layer greatly reduced. Exists as bands of muscle called teniae coli. Most colon musculature is circular muscle Crypts of Lieberkühn exist but limited to mucous production Rectum – last reservoir for feces prior to anal canal Anal canal protected by stratified squamous epithelium Two sphincters control anal canal: Internal Sphincter - involuntary External Sphincter - voluntary (to a point) Colon/Rectum… Anal canal ridged with anal columns (folds) which contain an artery and vein These veins can become weakened forming a sac-like structure - hemorrhoids Hemorrhoids – often caused by poor diet straining too hard to void dense feces Sometimes occur during late pregnancy & childbirth due to increased abdominal pressures & straining Defecation may occur as a result of gastrocolic reflex ‘full stomach = GOTTA GO!’ (massive peristalsis) Liver Divided into sections called lobes (which are subdivided into lobules) Lobules are hexagonal and are composed of cords of simple cuboidal epithelium called hepatic cords Cords separated by two cavities Capillary sinusoids – capillaries of circulatory system Bile canaliculi – transport of bile Border of lobule = site of hepatic triad • branch of bile duct – collects bile from canaliculi • branch of hepatic artery – oxygenated blood • branch of portal vein – blood from stomach/intestine Bile Produced in liver lobules by hepatocytes (liver cells) Drains from bile canaliculi – bile duct – hepatic duct – cystic duct – gall blader Bile – drains from gall bladder into duodenum through the common bile duct … from liver into CBD from Common hepatic duct Bile emulsifies fat Movie Break! Gall Stones Other Liver Functions Produces blood proteins – fibrinogen, albumin, prothrombin Stores minerals – zinc, magnesium, iron, copper Stores vitamins A, D, E & K Stores glycogen ‘animal starch’ Nutrient conversion – fat to glucose, glucose to fat, protein to fat, proteins to glucose Detoxifies poisons including alcohol More functions of Liver Breaks down bilirubin (from hemoglobin) into biliverdin for secretion Von Kupffer’s Cells – part of mononuclear phagocytic system line the sinusoids Pancreas Elongated organ runing along curve of duodenum. Contains both endocrine and exocrine glands Endocrine portion in isolated spots called Islets of Langerhans produce insulin Exocrine portion – Acinar glands – secrete digestive enzymes which drain via pancreatic duct into the duodenum Cells along duct secrete bicarbonate ions which serve as a buffer to help neutralize stomach acid Examine Models! Final Thursday May 3 8:00 – 10:00 a.m. Phases (3) of Deglutition swallowing 1. Voluntary – a bolus (lump) of food is formed by jaw/tongue action and is pushed against the roof of the mouth. This action forces the bolus backward into the orpharynx Pharyngeal Phase of Swallowing 2. Pharyngeal Phase – touch activated receptors in oropharynx are triggered when contacted by food bolus. Cranial nerves V and IX signal swallowing center in medulla. Nerves V, IX, X and XI signal muscles in soft palate and pharynx. • soft palate lifts to seal entry to nasopharynx (nothing up your nose!) • pharynx rises to accept bolus • superior, middle and then inferior pharyngeal muscles contract to move bolus downward toward and then into esophagus • Epiglottis (flap closing larynx) pushed back/down so it covers larynx (don’t breathe your food!) Swallowing continues 3. Esophageal phase – moves food between pharynx & stomach peristaltic waves of the muscles in the esophageal wall cause bolus to proceed down length of esophagus. As one region contracts, the area immediately below relaxes this set of involuntary contractions is mediated by the intramural plexus (a network of nerve fibers) and by tactile receptors in the esophageal wall which send impulses via the vagus to medulla then back through vagus to muscles in the esophagus Stomach Regulation Three Phases Cephalic Phase Gastric Phase Intestinal Phase histamine analogs such as Tagamet® and Zantac® bind to histamine receptors on parietal but dofluid not Function – prepare stomach for arrival of food by increasing stimulate release of HCl. volume. Cephalic Phases Duration – short (minutes) These are competitive Triggered by smell, taste, texture and thoughts of food. inhibitors that function Mechanism – Neural, via preganglionic fibers in vaguslike synapsing something a ‘broken with nerve plexus in stomach. Stimulates stomach key’ cells Actions: • Parietal cells – release hydrochloric acid • Chief cells – release pepsinogen • Endocrine cells – release gastrin (hormone), which triggers further release of HCl & pepsinogen • Mast cells – release histamine triggering parietal cells to secrete even more HCl Gastric Phase Functions: Enhance secretion started in cephalic stage, homogenize and acidify chyme, initiate digestion of proteins by pepsin Duration: long (3-4 hours) Mechanisms: •Neural: short reflexes triggered by stimulation of stretch receptors as stomach fills stimulation of chemoreceptors as pH changes •Hormonal: stimulation of gastrin released from endocrine cells •Local: release of histamine by mast cells as stomach fills Actions: increased acid & pepsinogen produced, increased motility beginning of mixing waves of muscle contraction Intestinal Phase Function: control rate of chyme entry into duodenum Duration: long (hours) Mechanisms: Neural: short reflexes (enterogastric) triggered by distension of duodenum. Hormonal: (two components) 1. stimulation of cholecystokinikn (CCK), gastrointestinal inhibitory peptide (GIP), and secretin all released in response to presence of acid, carbohydrates & lipids 2. release of gastrin released in response to presence of undigested proteins Actions: inhibit production of gastric acid and pepsinogen (by feedback inhibition) and reduce motility of stomach Mixing of stomach contents Muscular contractions mix food with stomach secretions to form chyme Mixing Waves – peristaltic contractions about every 20 seconds from body toward pylorus Peristaltic waves – more powerful, less frequent, force chyme toward pyloric sphincter. Simultaneously push more solid materials back toward cardiac region to continue processing Stomach Emptying Generally 1 ½ - 2 ½ hours after entering stomach, materials leave via pyloric sphincter by actions of pyloric pumping Peristaltic contractions of pylorus forces a small volume of chyme through the pyloric sphincter – action repeats until stomach is empty of chyme Digestion of Carbohydrates begins in mouth with salivary amylase, reduces macromolecules to polysaccharides and a few disaccharides – temporarily halts in stomach continues in intestine with pancreatic amylase which reduces these molecules to disacharides. Disaccharides are broken down by enzymes (disaccharideases) on intestinal microvilli in the lining of the small intestine. these enzymes convert the disaccharides into monosaccharides Disaccharides include: lactose, sucrose, maltose, isomaltose enzymes that digest these are xxxase where xxx = sugar name prefix e.g. sucrose cleaved by sucrase Digestion of Lipids Begins with emulsification by bile in duodenum – this breaks the lipids into small droplets increasing surface area so enzymes will have more area to work Lipase secreted by pancreas converts triacylglycerols to free fatty acids and glycerol Digested lipids together with bile salts form microscopic droplets called micelles which are absorbed when they come in contact with the epithelium of the small intestine Transport of Lipids Once inside intestinal epithelium, free fatty acids combine with gylcerol to form triacylglycerol. Proteins (made in intestinal epithelium) attach to surface of lipid molecules and form a ‘package’ called chylomicrons Chylomicrons leave intestinal epithelium and enter lymph lacteal for transport to circulatory system These protein coats are necessary because lipids are insoluble in water (thus insoluble in blood) Classes of lipoproteins include: VLDL, LDL, and HDL very low density, low density and high density lipoproteins Excess lipid removal Excess lipids packaged as HDLs for transport to liver where they are recycled or disposed Why HDL as packaging for transport – increased solubility in blood makes for easier transport Digestion of Proteins Begins in stomach with pepsin – cuts proteins into short polypeptide chains and some dipeptides. (10% - 20% digestion by pepsin) Duodenum – pancreatic enzymes continue digestion (trypsin, chymotrypsin, & carboxypeptidase) into smaller pieces Intestinal lining – enzymes (aminopeptidase, peptidase) in microvilli continue processing into tri/dipeptides and amino acids Digested amino acids and small peptides carried into epithelium by active transport on carrier molecules (more peptides than amino acids) Once internal to epithelial cells the small peptides are cleaved by dipeptidases or tripeptidases into amino acids. Examine Models!