Human Reproduction Biology
advertisement

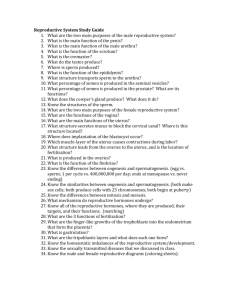
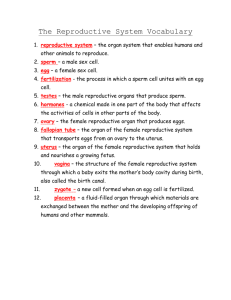
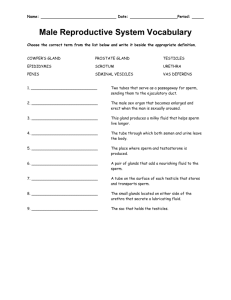
Human Reproduction Biology The Reproductive System The reproductive system functions in the production, support, and transport of sex cells (egg and sperm), as well as the production of sex hormones. Reproduction Overview A. Asexual reproduction – One parent makes identical babies (clones) B. Sexual reproduction – fusion of _gametes (sex cells)_ of two parents to form a _zygote (fertilized egg) 1. Fertilization – fusion of egg and sperm Reproduction Overview 2. Human reproduction – includes a. Formation of gametes (process of meiosis) b. Preparation for pregnancy c. Sexual Intercourse d. Fertilization which leads to pregnancy e. Lactation (milk production) 3. All coordinated by hormones of anterior pituitary (in brain) and the gonads (ovaries/testes) **Primary sex organs** Male Reproductive System-side view glans (AKA: Cowper’s gland) A. Functions: to produce sperm and deliver them to the female reproductive tract. Male Reproductive System-front view Male Reproductive System MALE REPRODUCTIVE STRUCTURES: 1. TESTIS: Primary male sex organs which produce sperm cells and the male sex hormone testosterone. Made up of highly coiled tubes called seminiferous tubules. 2. SCROTUM: Houses and protects testes by maintaining optimal temperature for sperm production. Male Reproductive System 3. SEMINIFEROUS TUBULES: Sperm production and transport of sperm to the epididymis. If stretched out will equal 20 feet. 4. EPIDIDYMIS: stores and matures sperm (gain motility). Male Reproductive System 5. VAS DEFERENS: Tube that carries sperm away from the epididymis 6. EJACULATORY DUCT: Transports sperm from the vas deferens to the urethra. This duct passes through the prostate gland. Male Reproductive System Production of sperm: is called Spermatogenesis Male Reproductive System 1. Happens in seminiferous tubules of testes. Spermatogonia ("stem cells") divide by mitosis - half undergo meiosis and mature to sperm cells (1 to 4 cells, this takes TWO months!) Male Reproductive System 2. Sperm consists of head, nucleus, midpiece and tail. SPERM CELLS: up to 350 million produced per day HEAD portion contains enzymes (to penetrate the egg’s outer layer) and a Nucleus with DNA. MIDPIECE: Contains mitochondria for energy. FLAGELLUM: Movement Size: 0.002 inches or 0.05mm Male Reproductive System 3. Scrotum –skin covered bag which contains testes a. Testes descend through inguinal canals 2 months before birth (inguinal hernia – part of intestines bulge through the inguinal canal and become stuck this could lead to surgery) b. Maintains temperature 2°C (3.5°F) below body temp. . Male Reproductive System D. Sperm Transport 1. From testes to epididymis (in scrotum) for storage & maturation (they remain here until they are released from the body). 2. To vas deferens (sperm duct) from scrotum to abdominal cavity peristaltic contractions move it along. 3. To ejaculatory duct which passes through the prostate gland. 4. To urethra through penis and out of body (urethra also for urine, a muscle located at the base of the bladder prevents urine and sperm from mixing.) Male Reproductive System E. Semen production: 1. Per ejaculate 300-400 million sperm plus secretions of accessory glands. Sperm makes up only about 2-% (If male produces <40 million sperm per ejaculate sterile) . (Note: only about 50 or so sperm make it alive to where the egg is waiting for it. 60% are usually deformed in some way. But, only one is needed to fertilize the egg) 2.Seminal vesicles empty into the vas deferens a mucus-like fluid that contains : *about 60% fructose (fruit sugar) for fuel. *bases to balance pH *hormones to stimulate contractions of female reproductive organs to move sperm toward the ova Male Reproductive System 3. Prostate gland--thin, milky, alkaline secretion which will neutralize the acid of other seminal fluids and the female's vagina. Male Reproductive System 4. BULBOURETHRAL GLANDS: (aka the Cowper’s gland). clear, alkaline fluid to neutralize urethra and lubricates the glans part of the penis (Note: there could be sperm in this fluid and therefore “pulling out” before ejaculation doesn’t work effectively as a form of birth control) Male Reproductive System F. Penis 1. The shaft ends in expanded tip, called the glans. Foreskin may cover the glans -- It is removed during circumcision (infections may occur if secretions are retained in this area) 2. Cavernous bodies--3 cylinders of erectile tissue with large blood vessels which fill during an erection. Male Reproductive System G. MALE REPRODUCTIVE HORMONES: 1. Puberty – sexual maturation. Begins at 12-13 years of age. 2. Testosterone: secreted during fetal development and shortly after birth. The production nearly stops until puberty - At puberty it promotes growth and … a. Primary sex characteristics– these are required for reproduction they are: making sperm, getting and maintaining an erection, and ejaculation. b. Secondary sex characteristics—these are not necessary for reproduction they are: deep voice, facial/body hair, broad chest, increased muscle mass. QUIZ time over the male’s system Female Reproductive System-side view Fallopian tube Ovary Uterus Cervix Urinary bladder Rectum Pubic bone Vagina Urethra d. Clitoris e. Labia minora f. Labia majora Female Reproductive System-front view Female Reproductive System A. Functions 1. Produce Ova (eggs) 2. Receive the penis and sperm 3. House and nourish the embryo (it is called this until the 8th week then it is called a fetus.) 4. Nourish the infant with milk Female Reproductive System B. Regulation of system Regulated by the Menstrual cycle Female Reproductive System A. FEMALE REPRODUCTIVE STRUCTURES: The primary sex organs are the ovaries. 1. OVARIES: Produce eggs and the sex hormones estrogen and progesterone. Female Reproductive System 2. FALLOPIAN TUBES: (aka oviduct tubes) The Fallopian tube expands to form a funnel shape with fingerlike extensions called fimbriae, which encircle each ovary and help direct the ovum (egg) into the Fallopian tube. • Main functions: site of fertilization and transport of ova to the uterus. Female Reproductive System 3. UTERUS: Where implantation and development of fetus takes place. Composed of three layers myometrium, perimetrium, and endometrium (some of this layer is lost during menstruation.) • Opening to the uterus is called the cervix. Female Reproductive System 4. Vagina: receives sperm and is the birth canal. 5. Cervix: entrance from vagina to the uterus Female Reproductive System All of the external structure are called the Vulva 1. Labia minora (inner) and Labia majora (outer) folds of skin. (protects the vaginal and urthral openings) 2. Clitoris -- similar to glans in male; center of sexual stimulation. 3. Hymen-- tissue that Urethra may partially block the vagina Clitoris 4. Urethra (not part of Labia minora the reproductive Labia majora tract)-- in front of vaginal opening; urinary passage Vagina Female Reproductive System D. Ova production and Female Hormones 1. Ovaries (primary female sex organ) produce and contain eggs in various stages of maturation 2. Oogonia (egg stem cells) are surrounded by follicle cells (where the eggs grow and mature). All eggs are produced before birth! However, only about 400 eggs will mature and have the ability to be fertilized. Note: “oo” means egg in latin Female Reproductive System 3. OOGENESIS: primary oocytes grow and begin meiotic division, then halt until puberty -then a few follicles develop each month due to the hormone FSH. Female Reproductive System 4. Ovulation -- mature follicle ruptures due to FSH and LH stimulation and ejects ovum into the pelvic cavity. 5. Follicle turns into the corpus luteum (yellow body) which secretes progesterone and estrogen which prepare uterus for pregnancy. Female Reproductive System Hormones functions: Control egg production, sexual function, and secondary sex characteristics. Female’s hormones: 1. Gonadotrophin Releasing Hormone (GnRH): the release of this hormone starts puberty. Female Reproductive System 2. Estrogen: At puberty, the ovaries secrete higher amounts which stimulate the growth and development of female primary sex characteristics and accessory organs. Estrogen and progesterone also develop and maintain female secondary sex characteristics such as increase in fat deposits, broadening of hips, and breast development. Female Reproductive System 3. Follicle Stimulating Hormone (FSH): stimulates the ovary to respond to estrogen and progesterone and initiates oogenesis. 4. Leutinizing Hormone (LH): gets the ovaries ready for egg production and causes ovulation at puberty. LH and FSH start the process of ovulation. Female Reproductive System 5. Progesterone: produced by the ovaries and prepares the lining of the uterus for pregnancy. 6. Testosterone: secreted by the pituitary gland causes a growth spurt at puberty and the growth of pubic hair and axillary hair. Female Reproductive System OVULATION: A surge of LH causes an egg to be released from the ovary and its follicle. The egg travels into the Fallopian tube where it either disintegrates (if not fertilized) or starts to mature (if fertilized) before going to the uterus. Female Reproductive System E. Ovum transport and pregnancy 1. After ovulation, ovum enters a fallopian tube (also called oviduct or uterine tube) a. It’s moved by muscular contractions and cilia. b. This is where fertilization occurs. (ectopic pregnancy = egg grows in the fallopian tubes) 2. Endometrium-- uterine lining which thickens in preparation for pregnancy. If egg is not fertilized, menstruation occurs. Female Reproductive System 3. Cervix lower part (neck) of uterus. Cancer detected here by a pap smear 4. Vagina -- internal tube, the birth canal; also receives the penis during intercourse. Female Reproductive System F. Menstural Cycle 28 day cycle that prepares the uterus for pregnancy 1. Begins at puberty (11-13 years): anterior pituitary secretes hormones FSH and LH 2. Ends at menopause (about 50 years) 3. Hormones use feedback mechanism between the reproductive system and the endocrine system Female Reproductive System Note: If an embryo becomes embedded in the uterine wall, the new glandular pockets will be stimulated to secrete hormones similar to progesterone/estrogen and the uterine lining will be maintained all through the pregnancy. Progesterone = stimulates the uterus to maintain its thickened lining and develop pockets that contains glands. Female Reproductive System Blood vessels grow in lining as it thickens Lining ready to receive an embryo 4-5 days after ovulation. If no embryo arrives, the blood vessels begin to break down. Blood cells from the lining pass through vagina during the menstrual period. Menstrual/ovarian cycles begin a new. Female Reproductive System Ovulation day 14-16: **Egg is able to stay alive 36-48 hours. **Sperm can live up to 72 hours in the female reproductive tract. Low levels of both estrogen/progesteron e signal onset of menstruation = also w/low levels of FSH, a new follicle will be stimulated to develop Female Reproductive System NOTE: After a women has a baby, it can be anywhere from 4-weeks to 3- months before her menstrual (bleeding) cycle reoccurs depending on if she is breast feeding or not. It doesn’t however, effect ovulation. She can still get pregnant. FERTILIZATION AND IMPLANTATION G. FERTILIZATION: Once an egg ruptures its follicle it has about 24 hours to be fertilized or it will die. Therefore sperm must be present in the Fallopian tube in order for fertilization to occur. Of the 100 to 305 million sperm released during ejaculation only about 50-100 will make it through the highly acidic environment of the vagina to the Fallopian tubes. When sperm meets the egg the enzymes in the head penetrate the egg and the sperm enters losing it’s tail and mid-section. Once inside no other sperm can penetrate the egg. Then the nucleus of the sperm with 23 chromosomes and the egg with 23 chromosomes form a zygote with 46 chromosomes. FERTILIZATION NOTE: A pregnancy test, using either urine or blood, tests for the presence of hCG (human chorionic gonadotropin) which is produced in the placenta) FERTILIZATION AND IMPLANTATION H. IMPLANTATION: The now fertilized zygote passes down the oviduct and begins mitosis (cell division resulting in cells exactly like the original cell.) On the 6th day the zygote reaches the uterus. The zygote is now surrounded by a hollow body of cells and is now called a blastocyst, which attaches to the lining of the uterus 7 to 8 days after fertilization. This process is called implantation. IMPLANTATION Quiz over Female Reproductive System IV. EMBRYONIC DEVELOPMENT A placenta is formed and is attached to the inside of the uterus. It unites the fetus to the uterus of the mother through the umbilical cord. This cord is made up of blood vessels. UMBILICAL CORD AND PLACENTA EMBRYONIC DEVELOPMENT EXCHANGE BETWEEN THE EMBYRO AND MOTHER: The blood supply of the mother and embryo do not mix. The nutrients and oxygen that the embryo needs are diffused from the mother’s blood vessels and taken in by the blood vessels of the embryo. Waste products from the embryo are diffused from the blood vessels in the umbilical cord to the mother’s blood vessels, where they are removed by the mother’s excretory system. A. FETAL DEVELOPMENT FETAL DEVELOPMENT INVOLVES 3 PROCESSES 1. Growth: increase in number of cells 2. Development: movement of cells in the embryo to develop into specific organs 3. Cellular differentiation: cells become specialized to perform specific tasks and functions. B. PERIODS OF PREGNANCY FIRST TRIMESTER (months 1 to 3): • Body systems begin to form • Woman may not realize she is pregnant • Embryo highly susceptible to external influences such as drugs, alcohol, and cigarette smoke; which increase likelihood of birth defects. • At 8 weeks all body systems are developed • Sex of fetus can be determined by appearance of male or female sex organs FIRST TRIMESTER (months 1 to 3) One Month weeks 4-7 Your baby is an embryo consisting of two layers of cells from which all her organs and body parts will develop. Two Months weeks 8-12 Your baby is now about the size of a kidney bean and is constantly moving. He has distinct, slightly webbed fingers. Three Months weeks 13-16 By now your baby is about 3 inches long and weighs nearly an ounce. Her tiny, unique fingerprints are now in place. http://www.babycenter.com/pregnancy-fetal-development-index PERIODS OF PREGNANCY SECOND TRIMESTER (months 4 to 6): • Growth primary focus • Rapid growth during 4th month • At 5 months fetus can survive outside the uterus but only with much medical assistance • Homeostasis not maintained by the body of the fetus • Immature lungs not able to provide a working respiratory rate SECOND TRIMESTER (months 4 to 6) Four Months weeks 17-20 Your baby is now about 5 inches long and weighs 5 ounces. His skeleton is starting to harden from rubbery cartilage to bone. Five Months weeks 21-24 Eyebrows and eyelids are now in place. Your baby would now be more than 10 inches long if you stretched out her legs. Six Months weeks 25-29 Your baby weighs about a pound and a half. His wrinkled skin is starting to smooth out as he puts on baby fat. http://www.babycenter.com/pregnancy-fetal-development-index PERIODS OF PREGNANCY THIRD TRIMESTER (months 7 to 9): • Weight of fetus doubles • Movement very common • Eyes open in 8th month • Rotates head to down position during the 9th month THIRD TRIMESTER ( months 7 to 9) Seven Months weeks 30-33 By now, your baby weighs about 3 pounds and is more than 15 inches long. She can open and close her eyes and follow a light. Eight Months weeks 34-37 Your baby now weighs about 4 3/4 pounds. His layers of fat are filling him out, making him rounder, and his lungs are well developed. Nine Months weeks 38-41 The average baby is more than 19 inches long and weighs nearly 7 pounds now, but babies vary widely in size at this stage http://www.babycenter.com/pregnancy-fetal-development-index Fraternal Twins 4 weeks 8 weeks 12 weeks 16 weeks Fraternal Twins 20 weeks 32 weeks 24 weeks 36 weeks BIRTH C. BIRTH: 3 stages 1. DILATION OF CERVIX: Labor begins with mild contractions of the uterine muscles – stimulated by the hormone oxytocin. These contractions open or dilate the cervix so the baby can pass through the vagina. Can last up to 24 hours. BIRTH 2. EXPLUSION OF BABY: Uterine and abdominal muscles work together to push the baby through the cervix into the birth canal or vagina. Can last 20 minutes to 1 hour. BIRTH 3. PLACENTAL STAGE: Placenta detaches from uterine wall and is expelled through the vagina. Contractions continue to prevent the mother from hemorrhaging or bleeding to death. V. Breasts: Mammary glands 1. Function --lactation (milk production) 2. During pregnancy estrogen and progesterone stimulate their growth 3. After child birth colostrum is produced (high protein substance that can increase immunity of the child, comes before the actual milk) 4. By 3rd day after birth prolactin (hormone) from anterior pituitary gland in the brain stimulates milk production. 5. Advantages of breast feeding a. Bonding occurs between mother and child b. Nutritionally perfect c. Child gets antibodies from mother d. Enhances recovery of the uterus after birth 6. Breast cancer --most common kind (after lung cancer) VI. Birth Control If you are against conception (having kids)– and you are using no method of birth control, 90% of women become pregnant in 1 year A. Very effective #1. Abstinence-- NOT having SEX = 100% EFFECTIVE! http://www.fda.gov/Fdac/features/1997/babyguide2.pdf If you think, just once won’t hurt… VI. Birth Control 2. Oral contraceptives – “The Combination Pill” is 99.9% effective; it prevents Ovulation (pregnancy 25/100,000) “The Mini-pill” only contains one hormone, progestin (it thickens the cervical mucus and makes the uterus less receptive to the implantation of the egg. Recommended for women who are breast feeding) 3. The Patch - thin, beige, plastic patch that sticks to the skin. It is used to prevent pregnancy. A new patch is placed on the skin once a week for three weeks in a row, followed by a patch-free week. (pregnancy <1/100 per year) VI. Birth Control 4. Sterilization a) Male – vasectomy (tying the vas deferens) b) Female – tubal ligation (tying the fallopian tubes) 5. Abortion (Ending of the pregnancy) a) A miscarriage – 50-67% of all pregnancies end in this type of spontaneous abortion b) Therapeutic -- to save mother's life c) As birth control – VERY controversial !!! VI. Birth Control B. Somewhat effective 1. Condom -- prevents sperm from getting into the female body. 2. Diaphragm -- prevents sperm from entering uterus. VI. Birth Control C. Not too effective 1. Rhythm -- abstinence during the fertile period 2. Douche --flushes semen from vagina. VII. Sexually Transmitted Diseases What are they? •Diseases that spread from one person to another during sexual contact •STDs are a serious problem in the U.S., infecting millions of people each year and accounting for thousands of deaths. VII. Sexually Transmitted Diseases •STDs caused by bacteria include chlamydia, syphilis, and gonorrhea. •STDs caused by viruses include hepatitis B, genital herpes, genital warts, and HIV/AIDS. •STDs caused by parasites include vaginitis, public lice, trichomoniasis and scabies. How STD’s affect a baby. STDs can have many of the same consequences for pregnant women as women who are not pregnant. STDs can cause cervical and other cancers, chronic hepatitis, pelvic inflammatory disease, infertility, and other complications. Many STDs in women are silent; that is, without signs or symptoms. STDs can be passed from a pregnant woman to the baby before, during, or after the baby’s birth. Some STDs (like syphilis) cross the placenta and infect the baby while it is in the uterus (womb). Other STDs (like gonorrhea, chlamydia, hepatitis B, and genital herpes) can be transmitted from the mother to the baby during delivery as the baby passes through the birth canal. She should consider a C-section to protect the baby from being infected. HIV can cross the placenta during pregnancy, infect the baby during the birth process, and unlike most other STDs, can infect the baby through breastfeeding. How STD’s affect a baby. A pregnant woman with an STD may also have early onset of labor, premature rupture of the membranes surrounding the baby in the uterus, and uterine infection after delivery. The harmful effects of STDs in babies may include stillbirth (a baby that is born dead), low birth weight (less than five pounds), conjunctivitis (eye infection), pneumonia, neonatal sepsis (infection in the baby’s blood stream), neurologic damage, blindness, deafness, acute hepatitis, meningitis, chronic liver disease, and cirrhosis. Most of these problems can be prevented if the mother receives routine prenatal care, which includes screening tests for STDs starting early in pregnancy and repeated close to delivery, if necessary. Other problems can be treated if the infection is found at birth. What are the FACTS about STD’s? You are going to look at a list of STD’s and record the following: – Type of pathogen: Viral, Parasitic, or Bacterial. – Where it would be found in the body. – How you would contract the STD. – Symptoms you would experience if you have that STD.