Chapter15 The Special Senses
advertisement

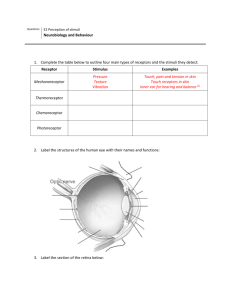
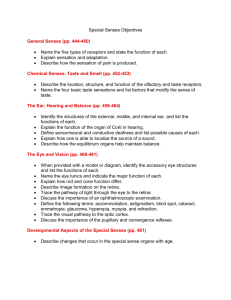
Chapter15 The Special Senses Introduction to Sensory Receptors: Receptor Classification • Receptor distribution • Special senses receptors • located within head • specialized, complex sense organs • five special senses – gustation (taste) – olfaction (smell) – vision (sight) – hearing (audition) – equilibrium (balance and acceleration) Introduction to Sensory Receptors: Receptor Classification • Stimulus origin – Exteroceptors • detect stimuli from external environment • receptors in the skin, special senses, membranes lining – Interoceptors • detect stimuli in internal organs • primarily stretch receptors in smooth muscle walls • mostly unaware of these sensations • also temperature, pressure, chemical changes, perceived pain – Proprioceptors • detect body and limb movements • muscles, tendons, and joints Receptor Classification • Modality of stimulus – Thermoreceptors • respond to changes in temperature • present in both skin and hypothalamus – Photoreceptors • located in the eye • detect changes in light intensity, color, movement – Mechanoreceptors • respond to touch, pressure, vibration, and stretch • most cutaneous receptors and ear – Baroreceptors • detect changes in stretch or distension • involved in regulation of blood pressure – Nocioceptors • respond to painful stimuli Tactile Receptors (Figure 16.3) Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. Unencapsulated tactile receptors Tactile disc Free nerve ending Encapsulated tactile receptors Tactile corpuscle End bulb Bulbous corpuscle Root hair plexus Lamellated corpuscle The General Senses: Referred Pain • Referred pain – Sensory nerve signals from certain viscera • not perceived as originating from organ • perceived as originating from dermatomes of skin – Same ascending tracts within spinal cord • house cutaneous and visceral sensory neurons – Sensory cortex unable to differentiate actual and false stimuli – Stimulus localized incorrectly Source of Referred Pain (Figure 16.4) Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. Posterior root ganglion Nociceptors in skin (pain receptors) Sensory pathway to brain Sympathetic trunk ganglion Sensory axons Spinal cord Gray ramus White ramus Nociceptors in wall of cecum and appendix Somatic sensory Visceral sensory The General Senses: Referred Pain Clinical View: Phantom Pain – – – – – – Sensation associated with removed body part Occurs following amputation of a limb Experience of pain from removed part Stimulation of sensory neuron pathway on remaining portion Cell body still alive Pain sometimes quite severe Olfaction and Gustation—Olfaction: The Sense of Smell • Olfactory organs – Organs of smell • Olfactory receptor cells – Olfactory hairs • unmyelinated extensions projecting from dendrites • house receptor proteins for detecting specific odorant molecule – Olfactory nerve (CN I) – Olfactory bulbs • terminal ends of olfactory tracts • inferior to the frontal lobes of the brain – Olfactory tracts • project directly to primary olfactory cortex in temporal lobe • projects to hypothalamus, amygdala, and other regions Olfactory Organs (Figure 16.6) Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. Olfactory tract Olfactory bulb Mitral cell Tufted cell Olfactory bulb Olfactory nerves (receptor cells) Nasal conchae Cribriform plate Olfactory glomerulus Olfactory nerves in cribriform foramen Olfactory gland Lamina propria Basal cell Supporting cell Olfactory receptor cell Cribriform plate of ethmoid bone Olfactory epithelium Olfactory epithelium in nasal cavity Mucus layer Axon Cell body Dendrite Olfactory hairs Odor molecules Olfactory Pathway to the Cerebrum The sensory neurons within the olfactory organ are stimulated by chemicals in the air. Axons leaving the olfactory epithelium collect into 20 or more bundles that penetrate the cribriform plate of the ethmoid. Olfactory organ The first synapse occurs in the olfactory bulb, which is located just superior to the cribriform plate. Axons leaving the olfactory bulb travel along the olfactory tract to reach the olfactory cortex, the hypothalamus, and portions of the limbic system. The distribution of olfactory information to the limbic system and hypothalamus explains the profound emotional and behavioral responses, as well as the memories, that can be triggered by certain smells. Cribriform plate of ethmoid Olfactory epithelium Superior nasal concha Figure 15.1 1 Olfaction and Gustation—Olfaction: The Sense of Smell • Detecting smells – Deep breathing • helps facilitate mixing of air in superior nasal cavity • helps diffusion of odor molecules into mucus layer Olfactory pathway action potential propagated through axon of olfactory receptor cells causes release of neurotransmitter from terminal ends of axon propagates signals through olfactory pathways sensory information reaches cerebral cortex, allowing for conscious smell hypothalamus, controlling visceral reactions amygdala, odor recognition and emotional association Smell adaptation ion channels altered once receptors stimulated interferes with subsequent receptor potentials adaptation to odors occurring rapidly Olfaction and Gustation—Gustation: The Sense of Taste • Gustation – Sense of taste – From molecules we eat and drink – Gustatory cells • taste receptors housed in specialized organs, taste buds – Involves mechanoreceptors and thermoreceptors • provide information about texture and temperature • Papillae and taste buds of the tongue – Papillae, epithelial and connective tissue elevations – On dorsal tongue surface Taste buds have appearance of an onion contain numerous taste receptors, gustatory cells Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. Root of tongue have 7 to 10 day life span enclosed by supporting cells basal cells, constantly replacing gustatory cells declining taste after age 50 reduction in gustatory cell replacement and number of taste buds Body of tongue Apex of tongue Epithelium Epithelium Filiform papilla Taste bud Fungiform papilla (a) Dorsal surface of tongue Taste bud Epithelium Foliate papilla Vallate Papilla and Taste Bud (Figure 16.7b-c) Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. Epithelium Stratified squamous epithelium of tongue surface Gustatory cell Gustatory microvillus Taste pore Supporting cell (b) Vallate papilla Sensory nerve Basal cell (c) Taste bud Olfaction and Gustation—Gustation: The Sense of Taste Gustatory discrimination and physiology of taste • Five basic taste sensations – Sweet • produced by organic compounds, e.g., sugar or artificial sweeteners – Salt • produced by metal ions, e.g., Na+ and K+ – Sour • associated with acids, e.g., vinegar – Bitter • produced by alkaloids, e.g., unsweetened chocolate – Umami • taste related to amino acids to produce meaty flavor Olfaction and Gustation—Gustation: The Sense of Taste • Gustatory discrimination and physiology of taste – Gustatory pathway (continued) • stimulates sensory neuron to convey information to brain – CN VII and CN IX • reaches medulla • triggers increased salivation and stomach secretions • triggers gag or vomiting in response to noxious stimuli • relayed to thalamus • then relayed to gustatory cortex for conscious taste • ability to taste heavily dependent on olfactory sense – e.g., food tasting bland during a cold • taste from info from gustatory and olfactory receptors External Anatomy of the Eye and Surrounding Accessory Structures (Figure 16.9a) Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. Eyebrow Eyelashes Superior eyelid Lacrimal caruncle Pupil Medial palpebral commissure Palpebral fissure Iris Lateral palpebral commissure Sclera (covered by ocular conjunctiva) Inferior eyelid (a) © The McGraw-Hill Companies, Inc./JW Ramsey, photographer • External accessory structures of the eye – Eyebrows • curved rows of thick, short hairs • prevent sweat from dripping into open eyes – Eyelashes • extend from margins of eyelids • prevent large objects coming into contact with eye – Eyelids • formed by fibrous core (tarsal plate) • tarsal glands sebaceous glands – produce secretion to prevent tear overflow – keep eyelids from adhering • ciliary glands – form secretory products – contribute to gritty material around eyelids after waking Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. Sagittal plane Levator palpebrae superioris muscle External Anatomy of the Eye and Surrounding Accessory Structures (Figure 16.9b) Eyebrow Orbicularis oculi muscle Conjunctival fornix Ocular conjunctiva Palpebral conjunctiva Tarsal plate Eyelashes Pupil Lens Iris aCornea Palpebral fissure Eyelid Tarsal glands Orbital fat Orbicularis oculi muscle (b) Visual Receptors: Accessory Structures of the Eye • Conjunctiva – – – – Specialized stratified squamous epithelium Continuous lining over external anterior eye Continuous lining over internal surface of eyeli Contains numerous goblet cells • lubricate and moisten the eye – Contains many blood vessels • supply nutrients to avascular sclera – Contains abundant nerve endings – Does not cover surface of cornea Visual Receptors: Accessory Structures of the Eye Clinical View: Conjunctivitis – – – – Most common nontraumatic eye complaint Inflammation and reddening of the conjunctiva Due to viral infection, bacterial infection, allergens, chemicals, irritants Trachoma • chronic, contagious form of conjunctivitis • caused by Chlamydia trachomatis • common cause of neonatal blindness in developing countries • newborn affected as passes through birth canal • inflammatory process causing scarring and thickening of conjunctiva Visual Receptors: Accessory Structures of the Eye • Lacrimal apparatus – – – – Produces, collects, and drains lacrimal fluid from eye Reduces friction from eyelid movement Cleanses and moistens eye surface Helps prevent bacterial infection • through action of antibacterial enzyme, lysozyme – Lacrimal gland • located in superolateral depression of orbit • continuously produces lacrimal fluid • washed over eyes by blinking eyelids – Nasolacrimal duct • receives fluid from lacrimal sac • drains fluid into lateral side of nasal cavity – mixes with mucus Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. Lacrimal puncta Lacrimal gland (orbital part) Lacrimal caruncle 1 Lacrimal canaliculi Lacrimal gland (palpebral part) 2 Lacrimal sac 3 Lacrimal Apparatus (Figure 16.10) 4 Nasolacrimal duct 5 Nasal cavity Nostril 1 Lacrimal fluid (tears) is produced in the lacrimal gland. 2 Lacrimal fluid is dispersed across eye surface when we blink. 3 Lacrimal fluid enters the lacrimal puncta, drains into the lacrimal canaliculi, and collects in the lacrimal sac. 4 Lacrimal fluid from the lacrimal sac drains through the nasolacrimal duct. 5 Lacrimal fluid enters the nasal cavity. Visual Receptors: Eye Structure • Characteristics – Almost spherical organ – Mostly receding into skull orbit – Orbital fat • cushions posterior and lateral eye • provides support and protection Visual Receptors: Eye Structure • Fibrous tunic – External layer of the eye wall – Composed of posterior sclera and anterior cornea – Sclera • the “white” of the eye • composed of dense irregular connective tissue • provides eye shape • protects eye’s internal components • attachment site for extrinsic eye muscles – Cornea • convex transparent structure • contains no blood vessels • convex shape refracting light rays coming into the eye Visual Receptors: Eye Structure • Vascular tunic – Middle layer of eye wall – Also called uvea – Houses • extensive blood vessels, lymph vessels – Three regions choroid ciliary body Choroid • most extensive posterior region • houses vast capillaries supporting the retina • cells filled with pigment from melanocytes • pigment absorbing extraneous light iris Visual Receptors: Eye Structure • Ciliary body: Ciliary muscles • suspensory ligaments extending from muscle to lens • contraction changing tension on ligaments, altering lens shape Ciliary processes • contain capillaries secreting aqueous humor • Iris most anterior region colored portion of the eye composed of two layers of pigment-forming cells two groups smooth muscle fibers vascular and nervous structures • Pupil black opening at center of iris pupil size controlled by two smooth muscle layers controls amount of light entering the eye Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. Pupillary constriction Pupillary dilation Bright light Low light Pupil Diameter (Figure 16.12) Sphincter pupillae contracts (parasympathetic innervation) Dilator pupillae contracts (sympathetic innervation) Visual Receptors: Eye Structure • Retina – Internal layer of eye wall – Outer pigmented layer and inner neural layer – Pigmented layer • internal to choroid and attached to it • provides vitamin A for photoreceptors (light-detecting cells) • light rays passing through inner layer absorbed here – Inner neural layer • houses photoreceptors (rods and cones) and associated neurons • responsible for absorbing light rays • converts into nerve signals transmitted to brain Visual Receptors: Eye Structure • Retina (continued) – Optic disc • contains no photoreceptors • where ganglion axons exit toward brain • commonly termed the blind spot – Macula lutea • rounded, yellowish region lateral to optic disc • contains fovea centralis, depressed pit – highest proportion of cones and few rods – area of sharpest vision A photograph of the retinal surface, taken through the cornea, pupil, and lens of the right eye Optic disc (blind spot) Fovea Macula lutea Central retinal artery and vein emerging from center of optic disc Figure 15.14 2 Structure and Organization of the Retina (Figure 16.13a-b) Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. Choroid Rod Cone Pigmented layer Retina Sclera Choroid Optic disc Photoreceptor cells Horizontal cell Bipolar cells Retina Amacrine cell Neural layer Ganglion cells Axons of ganglion cells to optic nerve Incoming light Nerve signal response to light through retina Optic nerve Fovea centralis (b) (a) Anatomy of the Internal Eye (Figure 16.11a) Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. Fibrous tunic Sclera Cornea Vascular tunic Iris Ciliary body Choroid Retina Pigmented layer Neural layer (a) Visual Receptors: Eye Structure Clinical View: Detached Retina – – – – – – Occurs when outer pigmented and inner neural layers separate May result from head trauma Increased risk in diabetics and nearsighted individuals Results in nutrient deprivation in inner neural layer Symptoms of “floaters” and “curtain” in affected eye Symptoms of flashes of light, decreased vision Visual Receptors: Eye Structure Clinical View: Macular Degeneration – Physical deterioration of macula lutea – Leading cause of blindness in developed countries – May be associated with • diabetes, ocular infection, hypertension, eye trauma – Loss of visual acuity in center of visual field – Diminished color perception and “floaters” Visual Receptors: Eye Structure • Lens – Strong deformable transparent structure – Composed of precisely arranged layers of cells • have lost their organelles • filled completely by crystallin protein – Focuses incoming light onto the retina – Suspensory ligaments • transmit tension enabling lens to change shape – Ciliary muscles • when relaxed, ciliary body moved posteriorly • tension of suspensory ligaments increases causes lens to flattendefault position for the lens view distant objects • opposite process initiated for close objects • contraction of muscle, moves ciliary body anteriorly • reduces suspensory ligaments’ tension lens more spherical • process termed accommodation Visual Receptors: Eye Structure Clinical View: Cataracts – – – – – Small opacities within the lens Usually as a result of aging Difficulty focusing on close objects Reduced visual clarity and reduced color intensity Needs to be removed when interferes with normal activities Normal eye Eye with cataract Figure 15.18 3 Visual Receptors: Eye Structure • Cavities of the eye – Posterior cavity • posterior to lens and anterior to retina • occupied by vitreous humor – transparent, gelatinous fluid between lens and retina – helps maintain eye shape and supports retina – transmits light from lens to retina – Anterior cavity • anterior to lens and posterior to cornea – Aqueous humor • fluid in anterior chamber • filtrate of blood plasma resembling cerebrospinal fluid • produced by ciliary processes • provides nutrients and oxygen to lens and cornea Clinical View: Glaucoma – Characterized by increased intraocular pressure Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. Anterior cavity Anterior chamber Posterior chamber Posterior cavity Aqueous Humor: Secretion and Reabsorption (Figure 16.16) Iris Cornea Lens Pupil 2 Anterior chamber Suspensory ligaments Posterior chamber 3 Anterior cavity (contains aqueous humor) 1 Scleral venous sinus Angle Posterior cavity (contains vitreous humor) Ciliary processes 1 Aqueous humor is secreted by the ciliary processes into the posterior chamber. 2 Aqueous humor moves from the posterior chamber, through the pupil, to the anterior chamber. 3 Excess aqueous humor is resorbed via the scleral venous sinus. Anatomy of the Internal Eye (Figure 16.11b) Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. Ora serrata Central artery of Central retina vein of retina Ciliary muscle Ciliary process Ciliary body Suspensory ligaments Limbus Scleral venous sinus CN II (optic) Lens Iris Cornea Optic disc Pupil Fovea centralis Posterior cavity Retina Choroid Sclera (b) Anterior chamber Posterior chamber Anterior cavity Visual Receptors: Eye Structure Clinical View: Functional Visual Impairments – Emmetropia, normal vision • parallel rays of light focused exactly on retina – Hyperopia • trouble seeing up close (far-sighted) • only convergent rays from distant points brought to focus • eyeball too short • focus posterior to retina • corrective convex lens – Astigmatism • unequal focusing • due to unequal curvatures in one or more refractive surfaces Visual Receptors: Eye Structure Clinical View: Functional Visual Impairments (continued) – Myopia • trouble seeing faraway objects (near-sighted) • only rays close to eye focus on retina • eyeball too long • focus anterior to retina in vitreous body • corrective concave lens – Presbyopia • age-related change • lens less able to become spherical • reading close-up words difficult • corrective convex lens – Can be treated with various surgical techniques The shape of the eye and the site at which light is focused for three conditions Enmetropia, or normal vision Emmetropia Myopia, or nearsighted vision Myopia Diverging lens In the normal healthy eye, when the ciliary muscle is relaxed and the lens is flattened, the image of a distant object will be focused on the retina’s surface. This condition is called emmetropia (emmetro-, proper + opia, vision), or normal vision. If the eyeball is too deep or the resting curvature of the lens is too great, the image of a distant object is projected in front of the retina. Such individuals are said to be nearsighted because vision at close range is clear but distant objects are blurry and out of focus. Their condition is more formally termed myopia (myein, to shut + ops, eye). Myopia can be treated by placing a diverging lens in front of the eye. Diverging lenses have at least one concave surface and spread the light rays apart as if the object were closer to the viewer. Hyperopia, or farsighted vision Hyperopia If the eyeball is too shallow or the lens is too flat, hyperopia results. The ciliary muscle must contract to focus even a distant object on the retina, and at close range the lens cannot provide enough refraction to focus an image on the retina. Individuals with this problem are said to be farsighted, because they can see distant objects most clearly. Hyperopia can be corrected by placing a converging lens in front of the eye. Converging lenses have at least one convex surface and provide the additional refraction needed to bring nearby objects into focus. Figure 15.17 Lens Shape in Far Vision and Near Vision (Figure 16.15) Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. Ciliary muscles contract, moving ciliary body closer to the lens. Ciliary muscles relaxed Lens flattened Suspensory ligaments taut (a) Lens shape for distant vision Lens thickened, more spherical Suspensory ligaments relaxed (b) Lens shape for near vision (accommodation) Visual Receptors: Physiology of Vision Photoreceptors • Rods – – – – – More numerous than cones Primarily located in peripheral regions of neural layer Especially important in dim light Detect movement well but have poor sharpness Cannot distinguish color • Cones – – – – – Less numerous than rods Activated by high-intensity light Provide precise visual sharpness and color recognition Primarily located in fovea centralis Subdivided into three types of cones red blue green • each best detecting different wavelengths Absorption Wavelengths (Figure 16.19) Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. Blue cones 420 nm Rods 500 nm Green cones 531 nm Percent of cone response 100 Red cones 558 nm 80 60 40 20 400 500 600 Wavelength (nm) 700 Visual Receptors: Physiology of Vision Clinical View: Color Blindness – X-linked recessive condition more common in males – Absence or deficit in one type of cone cell – Red and green most commonly affected • results in difficulty distinguishing red and green – Dark adaptation • return of sensitivity to low light levels after bright light • cones initially nonfunctional in low light • rods still bleached from bright light conditions • may take 20 to 30 minutes to see well Visual Receptors: Visual Pathways • Pathway characteristics – Optic nerve • formed from converged ganglionic axons • project from each eye • converge at the optic chiasm anterior to pituitary gland • medial axons crossing to opposite side of brain • lateral regions remaining on same side – Optic tracts • extend laterally from optic chiasm • composite of axons originating from both eyes • The ear Ear Structure – Detects sound and movements of the head – Signals transmitted via vestibulocochlear nerve (CN VIII) – Partitioned into external, middle, and inner ear The ear’s three anatomical regions: the external ear, the middle ear, and the inner ear External Ear Middle Ear Inner Ear The visible portion of the ear; collects and directs sound waves toward the middle ear An air-filled chamber; is connected to the nasopharynx by the auditory tube Site of sensory organs for hearing and equilibrium; receives amplified sound waves from the middle ear Elastic cartilages Auditory ossicles Semicircular canals Petrous part of temporal bone Auricle Facial nerve (VII) Vestibulocochlear nerve (VIII) Bony labyrinth Tympanic cavity To nasopharynx External acoustic meatus Tympanic membrane (tympanum or eardrum) Auditory tube (pharyngotympanic tube or Eustachian tube) Figure 15.4 1 Ear Structure • External ear – Auricle • funnel-shaped visible part of ear • skin-covered, elastic cartilage-supported structure • protects entry into ear and directs sound waves in – External acoustic meatus • bony tube extending slightly superiorly from lateral head – Tympanic membrane (eardrum) • partition between external and middle ear • vibrates when sound waves hit it • transmits sound wave energy into middle and inner ear • fine hairs guarding opening • cerumen, waxlike secretion of ceruminous glands – combines with dead sloughed cells to form earwax – may help impede growth of microorganisms Ear Structure • Middle ear – Contains air-filled tympanic cavity • sound transmitted through here via auditory ossicles – Bound medially by bony wall • houses oval window and round window • separates middle ear from inner ear – Auditory tube (Eustachian tube) • passage extending from middle ear into nasopharynx • has normally closed opening at connection to nasopharynx • allows pressure to equalize within middle ear Hearing and Equilibrium Receptors: Ear Structure • Auditory ossicles – – – – Three smallest bones of the body Amplify and transmit sound waves into inner ear Vibrate when sound waves strike tympanic membrane Malleus • attached to medial surface of tympanic membrane • resembles a hammer in shape – Incus • middle ossicle resembling an anvil – Stapes • resembles a stirrup • has disclike footplate fitting into oval window • marks lateral wall of inner ear Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. Temporal bone (petrous part) Middle Ear (Figure 16.25) Auditory ossicles Malleus Incus Stapes Oval window Stapedius Tensor tympani (cut) Tympanic membrane Round window External acoustic meatus Auditory tube Tympanic cavity Hearing and Equilibrium Receptors: Ear Structure Clinical View: Otitis Media – Infections of the middle ear – Most often experienced by young children • horizontal, short auditory tubes – Causative agent from respiratory infection • may spread from pharynx through auditory tube – Fluid accumulation in middle ear – Pressure, pain, sometimes reduced hearing – Evaluated with otoscope – May require myringotomy, surgical procedure Ear Structure • Inner ear – Bony labyrinth • spaces within the temporal bone • contains membrane-lined fluid-filled tubes • contains endolymph, similar to intracellular fluid – Three partitions of bony labyrinth • cochlea – houses cochlear duct – The organ of Corti, located in the cochlear duct, is the auditory organ. It contains about 20,000 hearing receptor cells and many supporting cells. • vestibule – contains two saclike, membranous parts • semicircular canal – membranous labyrinth here termed the semicircular ducts Inner Ear (Figure 16.26) Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. Membranous labyrinth (semicircular duct) Endolymph Bony labyrinth (semicircular canals) Perilymph Membranous labyrinth (semicircular ducts) Bone Bony labyrinth (semicircular canal) Cochlear branch of CN VIII Utricle Bony labyrinth (cochlea) Vestibule Saccule Apex of cochlea (contains helicotremma) Spiral organ Membranous labyrinth (cochlear duct) Endolymph Membranous labyrinth Bony labyrinth Ampullae Connection to cochlear duct Perilymph Spiral ganglion Membranous labyrinth (cochlear duct) Bony labyrinth (cochlea) Bone Hearing and Equilibrium Receptors: Physiology of Hearing Structures for hearing • Cochlea – Snail-shaped spiral chamber within bone of inner ear – Houses the spiral organ, responsible for hearing • Spiral organ – Within cochlear duct – Thick sensory epithelium consisting of hair cells and supporting cells – Hair cells • sensory receptors of inner ear for hearing • release neurotransmitter molecules to sensory neurons • covered on apical surface with long microvilli, stereocilia Hearing and Equilibrium Receptors: Physiology of Hearing • The pathway from sound wave to nerve signal – – – – – – – – Sound waves funneled by auricle of external ear Enter external acoustic meatus Make tympanic membranes vibrate Sound waves amplified- bones in middle ear Foot of stapes moving in oval window Transmits sound waves into pressure waves within inner ear Pressure waves continuing through perilymph Causes distortion of hair cells Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. External ear Pressure High pressure (loud) Middle ear Low pressure (less loud) Amplification in middle ear Amplitude Tectorial membrane Direction of sound waves Sound Waves Pathways Through the Ear (Figure 16.28) Auditory ossicles Malleus Incus Hair cell Stapes Cochlear branch of CN VIII Basilar membrane Oval window Scala vestibuli Helicotrema 2 3 Cochlear duct External acoustic meatus 5 1 Vestibular membrane 4 Spiral organ Basilar membrane Tympanic membrane Scala tympani Round window Auditory tube 2 Tympanic membrane vibration moves auditory ossicles; sound waves are amplified. 4 Pressure waves cause the vestibular membrane to move, resulting in pressure wave formation in theendolymphwithin the cochlear duct and displacement of a specific region of the basilar membrane. Hair cells in the spiral organ are distorted, initiating a nerve signal in the cochlear branch of CN VIII. 3 The stapes at the oval window generates pressure waves in the perilymph within the scala vestibuli. 5 Remaining pressure waves are transferred to the scala tympani and exit the inner ear via the round window. 1 Sound waves enter ear and cause the tympanic membrane to vibrate. Mechanisms of Equilibrium and Head Movement • Equilibrium Awareness and monitoring of head position- – Monitored by Vestibule and semicircular ducts – Information sent to brain to help keep our balance – Vestibule: macula and otolithic membrane Macula composed of layer of hair cells and supporting cells Otolithic membrane formed of gelatinous layer and otoliths- small masses of calcium carbonate crystals-positioned influenced by head position • Semicircular ducts – Semicircular canal • Detection of rotational movement • with head rotation, lagging of endolymph • pushes against cupula, causing bending of stereocilia • results in altered neurotransmitter release from hair cells • stimulation of sensory neurons • response primarily to changes in velocity Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. Semicircular ducts Ampullae Cupula Vestibular branch of CN VIII Ampulla (Figure 16.34) Cupula Endolymph Kinocilium Stereocilia Hair cell Crista ampullaris Vestibular branch of CN VIII Supporting cell Macula Structure (Figure 16.32b-c) Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. Otoliths Otolithic membrane Gelatin layer Kinocilium Stereocilia Hair cell Macula Supporting cells Vestibular branch of CN VIII (b) Macula Vestibular nerve branches (c) Hair cell Macula in Upright Head Position (Figure 16.33a) Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. Otoliths Gelatin layer Otolithic membrane Kinocilium Head upright Stereocilia Otolithic membrane Stereocilia parallel to kinocilium • Neurotransmitter released at regular interval • Steady rate of nerve signals are transmitted along vestibular branch of CN VIII Hair cell Standard nerve signal frequency Vestibular branch of CN VIII Supporting cell (a) Macula in upright head position Macula inAltered Head Position (Figure 16.33b) Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. Stereocilla bent toward kinocilium • Hair cells depolarize, increasing neurotransmitter release Head tilted upward • Increased nerve signal frequency along vestibular branch of CN VIII Excitation Stereocilia of hair cells bend. Otolithic membrane moves. Stereocilla bent away from kinocilium Gravitational force •Hair cells hyperpolarize, inhibiting neurotransmitter release Head tilted downward •Decreased nerve signal frequency along vestibular branch of CN VIII Inhibition (b) Macula in altered head position Function of the Crista Ampullaris (Figure 16.35) Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. Head still Head rotating Ampulla Section of ampulla filled with endolymph Ampulla Cupula being moved by the inertia of the endolymph Bending stereocilia Axons of vestibular branch of CN VIII Nerve signals sent to brain Physiology of the Ear • Sound waves – frequency – amplitude • Outer and middle ear – reception – increase & decrease sound • Cochlea – organ of hearing • sound ---> cochlear nerve ---> temporal lobe • Pitch transmission – frequency specific hairs • Loudness transmission – amplitude – more hairs stimulated Homeostasis Imbalances • Deafness – conduction deafness - hearing aid – sensorineural deafness • loud noise • damage organ of corti • Tinnitus – ringing in ears, clicking • Meniere’s Syndrome – arteriosclerosis – cranial nerve fluid pressure & “howling” • Motion Sickness – sensory input Figure 15.8 3