Senses Notes
advertisement

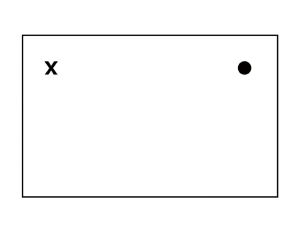
Definitions Pinna— Elastic cartilage Tympanic membrane— eardrum Ear ossicles— malleous, incus, stapes Two membranes in inner ear— oval window, round window Eustachian tube— connects ear to throat Function— equalize pressure Inner Ear Labyrinth Bony Cochlea: Hearing Vestibule: Balance Semicircular canals: Balance Membranous Lymphs Endolymph In membranous labyrinth Perilymph Space between membranous and bony labyrinth Hearing Organ of hearing: How we hear— happens within the cochlea Effect of Sound Waves on Cochlear Structures Hearing Process Waves move perilymph Perilymph moves vestibular membrane that moves endolymph Endolymph moves tectorial membrane which moves the hair cells Hair cells send impulse to nerves & the brain Sound waves leave through round window Auditory Function Vibrations produce sound waves Volume or loudness : number of hairs stimulated Pitch: Function of wave frequency Balance Static Evaluates position of head relative to gravity Detects linear acceleration and deceleration Kinetic Evaluates movements of head 3 semicircular canals Ampulla endolymph moves when head moves Semicircular Canals Contain fluid and hair Movement moves fluid & hairs Sends impulse to brain Ear Disorders Tinnitus Ringing, clicking, whistling in ear due to disorders in middle or inner ear Motion sickness Dysfunctions caused by stimulation of semicircular canals during motion Otitis Media Infections Earache Results in the middle ear from otitis media, dental abscesses, TMJ pain The Eye Structure of the Eye Layers and coats Fibrous Tunic: Outer Sclera—tough, white, outer portion; maintains shape, protects internal structures, provides muscle attachment point; continuous with cornea Cornea—transparent portion of anterior eye; avascular; bends & refracts light Vascular Tunic: Middle Choroid—middle layer; blood vessels & darkly pigmented Ciliary body—holds ciliary muscles (smooth) attached to lens w/ suspensory ligaments to control lens shape Lens- transparent; bioconvex Iris—colored, smooth muscle ring with the pupil in the middle; controls light entering pupil Structure of the Eye Continued Retina—Inner Retina-incomplete, innermost layer; nervous layer (contains neurons sensitive to light) Rods (black & white) Cones (color) Fovea Centralis/Macula lutea- where light is focused; see fine images (area of greatest acuity) Optic disc (no photoreceptor cells) AKA Blind Spot Cavities (compartments) in the Eye Anterior cavity—between the lens and cornea Filled with aqueous humor—clear, watery fluid Helps maintain intraocular pressure Glaucoma—too much intraocular pressure due to too much aqueous humor Posterior cavity—behind the lens and posterior portion of the eye Filled with vitreous humor—soft, gelatin-like substance Helps with intraocular pressure to prevent collapse Muscles of the Eye Extrinsic eye muscle— skeletal muscles that move the eyeball Intrinsic eye muscle— smooth muscles in the eye—involuntary Iris Ciliary body Accessory structures Eyebrows & eyelashes—keep some foreign particles out of eye Eyelids—help with lubrication Conjunctiva-mucus membrane lining the lid (AKA Pink eye (conjunctivitis); caused by an infection or irritation Closes from outside to in/ top to bottom Lacrimal Apparatus Lacrimal apparatus Lacrimal Gland: Produces tears to moisten, lubricate, wash Lacrimal Canaliculi Collects excess tears Punctum Lacrimal Sac Nasolacrimal duct Opens into nasal cavity Concept Review 1. 2. What are the 3 main layers of the eye? -sclera, choroid, retina What are the 3 accessory structures and describe their function? -eyebrows, eyelashes, & eyelids (protection & lubrication) 3. Where are tears formed and where do they go? -lacrimal gland, nasalacrimal duct How we see (4 main steps) Formation of Vision on the Retina 1. Refraction of light rays cornea, aqueous humor, lens, vitreous humor 2. Accommodation of lens Increase in curvature to achieve greater refraction on near objects Emmetropia: Normal resting condition of lens Far vision: 20 feet or more from eye Near Vision: Closer than 20 feet 3. Constriction of pupil Iris contracts to limit the amount of light that enters the eye How we see Continued… Formation of Vision on the Retina 4. Convergence of eyes Light must hit the same spot of the retina on both eyes to see only one object Both eyes are directed on the object at the same angle Single binocular vision —seeing one object with two eyes Eye Disorders Myopia: Nearsightedness Hyperopia: Farsightedness Degeneration of accommodation, corrected by reading glasses Astigmatism: Cornea or lens not uniformly curved Strabismus: Lack of parallelism of light paths through eyes Retinal detachment Clouding of lens Macular degeneration Increased intraocular pressure by aqueous humor buildup Cataract Can result in complete blindness Glaucoma Image focused behind retina Presbyopia Focal point too near lens, image focused in front of retina Common in older people, loss in acute vision Diabetes Dysfunction of peripheral circulation The Mouth Sense of Taste Specific sense organ– TASTE BUDS Located on projections of tongue called papillae Structure of a Taste Bud Gustatory cell—contain tiny, cilia-like gustatory hairs Taste pore—opening in the papillae that is bathed in saliva *The chemicals of food must dissolve in the saliva to stimulate the hairs to start an impulse.* Primary Tastes The Nose Sense of Smell Olfactory organs Sensory hairs Olfactory cells Olfactory nerves Olfactory bulb Olfactory tract Smelling Substance must be: Able to become a gas Water soluble or very small Lipid soluble (to get into membrane) Effects of Aging on the Special Senses Slight loss in ability to detect odors Decreased sense of taste Lenses of eyes lose flexibility Development of cataracts, macular degeneration, glaucoma, diabetic retinopathy Decline in visual acuity and color perception