Lecture 5-214.ppt
advertisement

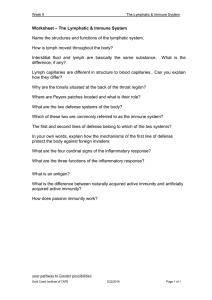
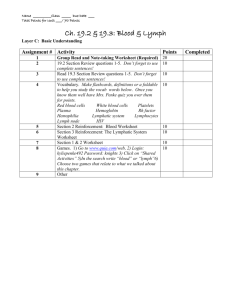
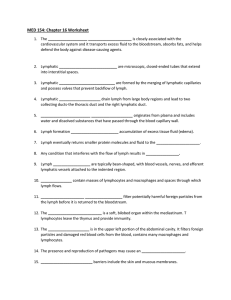
The Lymphatic System Introduction The ability to ward off pathogens that produce disease is called resistance Introduction Lack of resistance is called susceptibility Lymphatic System Consist of; lymph (fluid) lymphatic vessels lymphatic organs and tissues bone marrow Lymphatic System 1. Functions; Drain interstitial fluid Lymphatic System 2. Return leaked plasma proteins to the blood Lymphatic System 3. Protects against invasion by nonspecific defenses and specific immune responses Lymphatic Circulation Interstitial fluid drains into lymphatic capillaries thus forming lymph Lymphatic Circulation Lymph capillaries merge to form larger vessels, called lymphatic vessels Lymphatic Circulation Convey lymph into and out of structures called lymph nodes Lymphatic Capillaries Lymphatic capillaries are found everywhere except; 1. Avascular tissue Lymphatic Capillaries 2. CNS Lymphatic Capillaries 3. Portions of the spleen Lymphatic Capillaries 4. Red bone marrow Lymphatic Capillaries Lacteal – lymphatic capillary in the villus of the small intestine which transport fats Lymph Trunk and Ducts 1. 2. Thoracic Duct Right Lymphatic Duct Thoracic Duct Main collecting duct of the lymphatic system Thoracic Duct Receives lymph from the left side of the head, neck, and chest, the left upper extremity and the entire body below the ribs Thoracic Duct It drains lymph into venous blood via the left subclavian vein Right Lymphatic Duct Drains lymph from the upper right side of the body Right Lymphatic Duct It drains lymph into venous blood via the right subclavian vein Flow of Lymph 1. Fluid flows from arteries and blood capillaries to interstitial spaces (interstitial fluid) Flow of Lymph 2. To lymph capillaries (lymph) Flow of Lymph 3. To lymphatic vessels Flow of Lymph 4. To lymph trunks Flow of Lymph 5.To the thoracic duct or right lymphatic duct Flow of Lymph 6. To the subclavian veins (blood) Lymphatic Organs and Tissues Lymphatic organs are classified as primary or secondary Primary Lymphatic Organs Red bone marrow Thymus gland Secondary Lymphatic Organs Lymph nodes Spleen Lymphatic nodules Thymus Gland Lies between the sternum and the heart Thymus Gland Functions in immunity as the site of T cell maturation Thymus Gland Large in the infant and after puberty it is replaced by adipose and areolar connective tissue Lymph Nodes Are encapsulated oval structures located along lymphatic vessels Lymph Nodes Contain T cells, macrophages, follicular dendritic cells, B cells, and plasma cells Lymph Nodes Lymph enters nodes through afferent lymphatic vessels and is filtered to remove damage cells and microorganisms Lymph Nodes Exits through efferent lymphatic vessel Lymph Nodes Foreign substances filtered by the lymph nodes are trapped by nodal reticular fibers Lymph Nodes Macrophages destroys foreign substances by phagocytosis Lymph Nodes Lymphocytes bring about the destruction of others by immune response Lymph Nodes Site of proliferation of plasma cells (from B cells) and T cells Plasma cells make antibodies Spleen Largest mass of lymphatic tissue in the body Spleen Located between the stomach and diaphragm Spleen Made up of white and red pulp White Pulp Lymphatic Tissue White Pulp Its T lymphocytes directly attack and destroy antigens in blood White Pulp Its B lymphocytes develop into antibody producing plasma cells, and the antibodies inactivate antigens in blood White Pulp Macrophages destroy antigens in blood by phagocytosis Red Pulp 1. 2. Consists of; Venous sinuses Splenic cords Red Pulp Venous sinuses are filled with blood Red Pulp 1. 2. 3. 4. 5. Splenic cords consist of; RBCs Macrophages Lymphocytes Plasma cells granulocytes Red Pulp Macrophages remove deffective RBCs, WBCs, and platelets Red Pulp Stores blood platelets Lymphatic Nodules Oval-shaped concentrations of lymphatic tissue Lymphatic Nodules Scattered throughout the mucous membranes lining the GI tract, respiratory airways, urinary tract, and reproductive tract Peyer’s patches Lymphatic nodules in the ileum of the small intestine Tonsils Multiple aggregations of large lymphatic nodules at the junction of the oral cavity and the pharynx Tonsils 1. 2. 3. Include; Pharyngeal Palatine Lingual tonsils Tonsils Participate in immune responses by producing lymphocytes and antibodies Nonspecific Resistance to Disease Involves a 1. First line of Defense 2. Second line of Defense First Line of Defense Involves 1. Mechanical Protection 2. Chemical Protection Mechanical Protection Include 1. Epidermis layer of the skin Mechanical Protection 2. Mucous membranes in the nose and trachea Mechanical Protection 3. Lacrimal apparatus Mechanical Protection 4. Saliva Mechanical Protection 5. Mucus Mechanical Protection 6. Cilia Mechanical Protection 7. Epiglottis Mechanical Protection 8. Flow of urine Mechanical Protection 9. Defecation Mechanical Protection 10. Vomiting Chemical Protection 1. The skin produces sebum, which has a low pH Chemical Protection 2. Lysozyme in sweat has antimicrobial properties Chemical Protection 3. Gastric juice in the stomach has a low pH Chemical Protection 4. Vaginal acidic secretions are also Second Line of Defense Involves 1. Antimicrobial proteins 2. Phagocytic and natural killer cells 3. Inflammation 4. Fever Antimicrobial Proteins 1. 2. Interferons Complement System Interferons Body cells infected with viruses produce proteins called interferons (IFNs) Interferons IFN diffuses to uninfected cells and binds to surface receptors Interferons This induces uninfected cells to synthesize antiviral proteins that inhibit viral replication Complement System A group of 20 proteins present in blood plasma and on cell membranes Complement System When activated, these proteins enhance immune, allergic, and inflammatory reactions Natural Killer Cells Lymphocytes that lack the membrane molecules that identify T and B cells Natural Killer Cells Can kill a variety of infectious microbes and some tumor cells Natural Killer Cells Sometime release perforins that insert into the plasma membrane of a microbe and make the membrane leaky so that cytolysis occurs Natural Killer Cells Sometimes they bind to a target cell and inflict damage by direct contact Phagocytes Neutrophils and macrophages Inflammation Four symptoms 1. Redness 2. Pain 3. Heat 4. Swelling Inflammation Three stages 1. Vasodilation and increased permeability Inflammation 2. Emigration of phagocytes from the blood into interstitial fluid Inflammation 3. Tissue Repair Inflammation Vasodilation and increased permeability are responsible for heat, redness, and swelling Inflammation Pain results from injury to neurons and from toxic chemicals released by microbes Fever When macrophages respond to an infection, they release interleukin -1 Fever Interleukin-1 stimulates the hypothalamus to initiate a fever Fever Inhibits some microbial growth and speeds up body reactions that aid repair Major Histocompatibility Complex Antigens Unique to each person’s body cells Major Histocompatibility Complex Antigens All cells except rbc display MHC class I antigens Major Histocompatibility Complex Antigens Antigen presenting cells (macrophages) also display MHC class II antigens Pathways of Antigen Processing For an immune response to occur, B and T cells must recognize that a foreign antigen is present Pathways of Antigen Processing Antigens are chemical substances that are recognized as foreign by antigen receptors when introduced into the body Pathways of Antigen Processing The body contains millions of different T and B cells each capable of responding to a specific antigen Cell-Mediated Immunity Refers to destruction of antigens by T cells Cell-Mediated Immunity Three main steps Cell-Mediated Immunity 1. T cells recognize antigen fragments associated with MHC II class molecules on the surface of an antigen presenting cell (macrophage). Cell-Mediated Immunity Although CD8 cell receptors bind to the antigen associated with MHC class I molecules on the virus infected cell Cell-Mediated Immunity 2. A small number of T cells proliferate and differentiate into a clone of effector cells Cell-Mediated Immunity 2 continued … Clone of effector cells – a pop. of identical cells that can recognize the same antigen Cell-Mediated Immunity 3. Antigen (intruder) is eliminated Types of T Cells 1. 2. 3. Helper T (TH) cells Cytotoxic T (TC) cells Memory T cells Helper T cells T4 cells Helper T cells Display CD4 proteins Helper T cells Recognize antigen fragments associated with MHC-II molecules Helper T cells Secrete interleukin-2 which as a costimulator Helper T cells Proliferation of T cells requires costimulation Cytotoxic T cells Fight foreign invaders by killing the target cell Cytotoxic T cells Target cell – the cell that bears the same antigen that stimulated proliferation Cytotoxic T cells One killing mechanism uses perforin to cause cytolysis of the target cell. Cytotoxic T cells The second mechanism uses lymphotoxin to activate damaging enzymes within the target cells Cytotoxic T cells Main targets are virus infected cells Memory T cells Programmed to recognize the original invading antigen Antibody-Mediated Immunity Refers to destruction of antigens by antibodies Antibody-Mediated Immunity There are 4 steps Antibody-Mediated Immunity 1. An antigen binds to the surface of B cells Antibody-Mediated Immunity 2. Some antigen is taken into the B cell, broken down into peptide fragments and combined with the MHC-II self antigen, and moved to the B cell surface Antibody-Mediated Immunity 3. Hepler T cells recognize the antigen-MHC-II combination and secrete interleukins Antibody-Mediated Immunity The interleukins deliver the costimulation needed for B cell proliferation Antibody-Mediated Immunity 4. Some activated B cells become antibody-secretion plasma cells. Others become B cells Antibodies A protein that can combine specifically with the antigenic determinant on the antigen that triggered its production Antibodies 1. 2. 3. 4. 5. Five classes IgG IgA IgM IgD IgE IgG It binds to bacteria and viruses IgG It crosses the placenta until it can begin secreting its own. IgA It is in blood, breast milk, tears, saliva, and intestinal secretions. IgA Levels decrease during stress IgA Protects our mucous membranes against infections with bacteria and viruses IgM First antibody to be secreted by plasma cells after exposure to antigens IgM Antibodies to A and B red cell antigens are IgM IgM Cannot cross the placenta IgD Activate B cells IgE On the surface of mast cells and basophils IgE Involved in allergic reactions IgE When a person with pollen allergies inhales pollen, it combines with the IgE on their mast cells IgE Causes mast cells to release histamine AIDS A condition in which a person experiences infections as a result of the progressive destruction of cells by the humon immunodeficiency virus HIV The only documented transmissions are by way of blood, semen, vaginal secretions, and breast milk HIV A recent study in San Fran showed that 8% of their HIV-infected patients acquired it via oral sex HIV Form of a retrovirus with a protein coat HIV HIV enters CD4 positive T lymphocytes and macrophages where it sheds its protein coat HIV New HIV DNA is produced in the T cell along with new protein coats and then released HIV The T cells are ultimately destroyed HIV Progression to AIDS occurs because of reduced numbers of T cells and resulting immunodeficiency AIDS Person now susceptible to opportunistic infections HIV Treatment of HIV infection with reverse transcriptase inhibitors has shown to delay the progression of HIV infection to AIDS