Chronic gastritis
advertisement

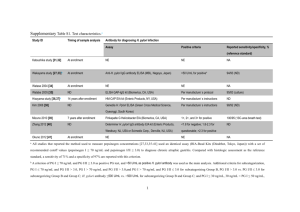
Pathological aspects of esophagus and stomach-III (Chronic Gastritis) Dr.Ashraf A.Fatah Deyab Assistant Professor of Pathology Pathological aspects of esophagus and stomach-III (Objectives) I. Discuss Chronic Gastritis II. Enlist the common causative agents in various age groups III. Explain the pathogenesis and pathology of Chronic Gastritis IV. Enlist clinical features Suggested reading: Robbin’s Basic Pathology, 8th Ed. Page-588-589 & 591-597 I. Discuss Chronic Gastritis- Definition Frequent disorders of the stomach in all taken biopsies. The term gastritis is used to denote inflammation associated with mucosal injury. Gastritis is mostly a histological term that needs biopsy to be confirmed. Gastritis is usually due to infectious agents (such as Helicobacter pylori) and autoimmune and hypersensitivity reactions. Anatomical site II. Common causative agents of Chronic Gastritis Infectious agents (Bacterial “bacillus Helicobacter pylori=90%”, parasitic, fungal, viral “CMV” infection). Autoimmune diseases. atrophic gastritis(10%) Hypersensitivity reactions.- rare Direct injurious agent (chemical or drugs, chemotherapy, radiation, alcohol etc..) chronic irritants (tobacco, caffeine) & secondary to other systemic diseases, malignancy& stresses. Others Less common etiologies (elderly, chronic bile reflux, mechanical injury- uremia, GVHD ). Chronic Gastritis- types 1- H.pylori gastritis= 90% 2. Autoimmune gastritis= 10% 3. Eosinophilic gastritis 4. Lymphocytic gastritis. 5. Granulomatous Gastritis Reactive gastropathy. Chronic gastritis Two major types: 1. Autoimmune gastritis (in association with pernicious anemia) Type A gastritis Also k/a fundic type 2. Chronic active (H.pylori) gastritis Type B gastritis Also k/a antral type 7 HELICOBACTER PYLORI GASTRITIS Most common cause of gastritis – H.pylori. Spiral-shaped or curved bacilli gram negativefacilitate its passage through the mucus layer of H. pylori has revolutionized understanding of chronic gastritis (90% of causes). 50% worldwide affected, most common bacterial infection in human. It was believed lifestyle factors, such as stress and diet types (spicy, acidic, fatty meals). H. pylori infection = found to be a\w increased risk of gastric cancer. discovery H.pylori gastritis Epidemiology High prevalence (USA) is a\w Poverty. Household crowding. Limited education. residence in rural areas. Age group: In high-prevalence area - Infection Acquired in childhood and then persists for decades. Transmission: - - not well defined. humans are the only known host Oral-oral, fecal-oral, and environmental spread . III. H. PYLORI GASTRITIS- Pathogenesis Started as Localized antral gastritis with ability to spread to form Pangastritis (cardia, body, fundus) H.pylori: features are linked to virulence: 1) Flagella& 2) Adhesion: enhance motility & invasion of mucosa (foveolar cells surface). 3) Urease: generate acid from endogenous ammonia from urea& there elevates local gastric PH. 4) Toxins: such as cytotoxin-associated gene A (Cag A)-in 50% of bacteria , that may also be involved in ulcer or cancer H.Pylori infection>> Increased acid production> overcome gastro-duodenal defense protective mechanism III. H. PYLORI GASTRITIS- Pathogenesis Helicobacter pylori can cause damage by (1) Secreting urease, protease, and phospholipases. (2) Attracting neutrophils that release myeloperoxidase. (3) Promoting thrombotic occlusion of capillaries, leading to ischemic damage of the epithelium III. H.pylori gastritis- morphology Predominantly antral gastritis with increase risk of DU is increased in antral gastritis. Pangastritis: then gastritis progresses to involve the gastric body, fundus& cardia. (mechanism may be due??): Host gene encode certin cytokines or influenced by Genetic variation among H. pylori strains Pangastritis: a\w 1) Multifocal atrophy – not a\w with perniciuos anemia. 2)Intestinal metaplasia 3) Increase risk of gastric ca. Gastrin- either Normal to decreased H.pylori gastritis- morphology Endoscopy: Gastritis( erythematous): 1) Localized Antral or 2) Pan-gastritis (+\-) Atrophic Gastric biopsy : 1) Dense chronic inflammatory infiltrate (lamina propria, Intraepithelial + Cross the BM ) + neutrphils+ pit abscesses+Subepithelial plasma cells+ glands destructionfibrosis +intestinal metaplasia Lymphoid aggregates with germinal centers H.pylori infection\colonies demonstrate in mucosa H.pylori may be found in gastric mucosa in Barrett’s . Chronic Atrophic Gastritis with intestinal metaplasia IV. Chronic Gastritis- clinical features Asymptomatic or Symptomatic: mild but more persistent. Nausea and upper abdominal discomfort, +\vomiting. Sequelae of H.pylori infection: Peptic ulcer, adenocarcinoma.) Investigations: (1) Urease test (2) breath test (3) H.pylori Ag – fecal test (4) Antibodies 5) PCR (6) Gastric biopsy histopathology . (7) Endoscopy (8) Antibodies to parietal cells Chronic gastritis- Other types AUTOIMMUNE GASTRITIS 10% of cases of chronic gastritis, typically spare the Antrum, mainly affect body& fundus. characterized by: • (1) Antibodies to parietal cells , intrinsic factor - found in serum & gastric secretion • (2) Reduced serum pepsinogen I conc. • (3) Antral endocrine cells hyperplasia. hypergastrinemia (4) Vitamin B12 deficiency (5) Defective gastric acid secretion (achlorhydria) AUTOIMMUNE pathogenesis Loss of Parietal cell (Ab. Damage)> reduce acid production & IF-this lead to enhance>> (1) Gastrin secretion + hypergastrinemia & hyperplasia. (2) IF lead to >> B12 deficiency. (3) Low acid > reduction PG1 (chief loss among parietal cell destruction) AUTOIMMUNE GASTRITIS Body& fundus involved Diffuse body mucosal damage& atrophy. Loss of parietal cells mucosa with rugal lost loss of acid & intrinsic factors secretion Lymph, MQ, plasma Neutrophils cells. Lymphoid aggregates Intestinal ,metaplasia endocrine hyperplasia AUTOIMMUNE GASTRITISclinical features Slow onset, variable progressive gastric atrophy, anemia – in a few patients. Median age for diagnosis 60 years old. F >M. A\W others autoimmune diseases , grave’s, DM-1, myasthenia gravis, ect.. Vit B12 deficiency, tongue – Atrophic glossitis , smooth +Megaloblastosis+ neurologic Chronic autoimmune gastritis Complications 1. Achlorhydria* 2. Hypergastrinemia* ➱ 3. Loss of acid (HCl) production results in Increased levels of gastrin (loss of negative feedback) Macrocytic anemia* Due to lack of intrinsic factor causing vitamin B12 deficiency. Increased risk for gastric adenocarcinoma** Increased risk for gastric carcinoid (why?). 4. 5. 21 Eosinophilic Gastritis. Tissue damage a\w dense infiltrates of eosinophils in the mucosa and muscularis, usually in Antral or pyloric region. Associate with: 1) GI eosinophilia. 2) Peripheral eosinophilia with increased serum IgE levels 3) Allergic reactions 4) Parasitic infections 5) H. pylori infection Lymphocytic gastritis Lymphocytic gastritis: nonspecific symptoms, idiopathic. 40% of cases a\w celiac disease (suggesting immune-mediated pathogenesis). Histologically-l limited to body marked increase in number of Intraepithelial of T lymphocytes. Lymphocytic gastritis Granulomatous gastritis: Gastritis contains granulomas, or aggregates of epithelioid histiocytes (tissue macrophages). a\w(: (1) Crohn disease 1st most common, (2) 2nd Sarcoidosis. (3) Infections by mycobacteria. fungi , CMV, and H. pylori Granulomatous gastritis Reactive Gastropathy Gastropathy: defined as epithelial cell damage and regeneration without associated inflammation. Gastropathy foveolar hyperplasia, glandular regenerative changes, and mucosal edema. Neutrophils are not abundant. Causes : irritants such as chemical or drugs (eg, NSAID and alcohol), bile reflux., and mucosal trauma. Endoscopy shows- watermelon stomach. Reactive Gastropathy – watermelon endoscopy appearance Reactive Gastropathy Antral reactive mucosa Dilated capillaries containing fibrin thrombi. MAJOR ASPECTS OF H.pylori ( TYPE A) & Autoimmune ( TYPE B) GASTRITIS FEATURE TYPE A GASTRITIS TYPE B GASTRITIS DISTRIBUTION Fundus, diffuse Pyloric antrum, focal GASTRIC SECRETION Reduced* Noramal or + or - ANTIBODIES TO PARIETAL CELLS Yes* No OTHER AUTOIMMUNE DISEASES Yes* No VITAMIN B12 Low* Normal PERNICIOUS ANEMIA + - GASTRIN Increased* Normal ANTIBODIES TO H PYLORI - + INCIDENCE Less common More common CANCER RISK Increased* Increased* 28 The end