Presentation Slides -T Nesman (pdf)
advertisement

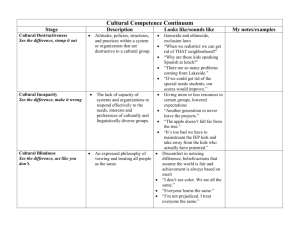
Teresa M. Nesman, Ph.D. November 30, 2012 Department of Child and Family Studies College of Behavioral and Community Sciences, USF Culture definitions are developed for different purposes, emphasizing different aspects of life. (Kao, Hsu, & Clark, 2004) ◦ Traits, abilities, and habits that signify membership in a society Volksgeist or the "spirit of the folk” - cultural traits are shaped by ancestral history & physical environment; include language, literature, religion, the arts, customs, & folklore (Herder, 1769) “Complex whole”- includes knowledge, belief, art, morals, law, custom, & any other capabilities & habits acquired by man as a member of society" (Tylor, 1958 [1871]) ◦ Shared behavior, lifestyle, and meanings: “Customs, beliefs, values, knowledge, and skills that guide a people’s behavior along shared paths” (Linton, 1947) “Means by which a local population maintains itself in an ecosystem” (Rappaport, 1968 [1980]) “Pattern of meanings embodied in symbols…by means of which men communicate, perpetuate, & develop their knowledge about and attitudes toward life" (Geertz 1973) Culture Culture Culture Culture Culture Culture Culture is is is is is is is general and specific shared learned symbolic adaptive and mal-adaptive integrated dynamic Everyone “has” culture Sense of self Group membership- individualism vs. collectivism Communication & language Relationships View of time Values & norms Beliefs & attitudes Mental processes & learning styles Work styles & practices Dress & appearance Food & eating habits Art & aesthetics Stately & Clark, 2003 Culture is often invisible to people until they find themselves in cross-cultural situations ◦ Since one is born into a culture, one experiences that culture as always already there, part of the world that one sees, not as a way of seeing the world (Steeves & Kahn, 1995, p. 183). Culture influences most, if not all aspects of human social interactions Self Actualization Esteem and Identity Love and Belonging Safety and Security Physiologic (e.g., Food, Water) Maslow’s Hierarchy Of Human Needs (Cross, Bazron, Dennis, & Isaacs, 1989) Culture influences health behaviors and expectations. Typical week’s groceries in Germany : $500.07 Typical week’s groceries in China : $155.06 Typical week’s groceries in Chad : $1.62 Life trajectories and health status are impacted by culture: ◦ ◦ ◦ ◦ Lifestyles Help-seeking behaviors Values/beliefs/norms of families & individuals Values/beliefs/norms of service systems Lack of cultural compatibility between health care organizations and clients reduces access to appropriate services and can result in: ◦ Misdiagnoses (Fabrega, Ulrich, & Mezzich, 1993; Kilgus, Pumariega, & Cuffe, 1995; Malgady & Constantino, 1998; U.S. DHHS, 2001; Yeh et al., 2002) ◦ Mistrust and low utilization of services (Snowden, 1998; Takeuchi, Sue, & Yeh, 1995; Theriot, Segal, & Cowsert, 2003; U.S. DHHS, 2001) (Hernandez & Nesman, et al., 2006) Understanding Cultural Influences in Yourself and Others What was in your “back yard” when you were a child? What did your kitchen look like? What was in it? Who spent most time in it? What were common foods you ate? When & where did you eat? How did you learn to read? Who helped you? What was a common saying related to health, hygiene, or well-being? What did your parent(s)/caregivers do when you were sick with a cold? Cultural Competence: What is it and Why is It Important? Culturally Diverse Contexts Individual In context of FAMILY In context of CULTURALLY DIVERSE ENVIRONMENT Process of becoming adapted to a new culture, either within the natural culture or among strangers, at home or in a foreign land. Process of learning to adjust. Involves re-orientation of thinking, feeling, and communicating. The force that moves a culture learner across a continuum from a state of no understanding of, or even hostility to, a new culture to a near total understanding. Moving from mono-culturism to bi- or multiculturism. What seems to be right, logical, sensible, important, or obvious to a person in one culture may seem wrong, irrational, silly, unimportant, or confusing to someone in another culture. Differences between cultures are too often perceived as threatening or bothersome and are described in negative terms. Most people take their own language for granted until they encounter another language. Understanding another culture requires personal experience and time spent interacting with members of that cultural group. Stereotyping is most likely to occur in the absence of frequent contact with people from other cultures. Understanding another culture is a continuous and not a discrete process. Culture is negotiated whenever two or more groups come in contact. “The acquisition of awareness, knowledge and skills needed to function effectively in a pluralistic democratic society (e.g., ability to communicate, interact, negotiate, and intervene on behalf of clients from diverse backgrounds)” (Stately & Clark, 2003) “The ability of individuals and systems to respond respectfully and effectively to people of all cultures, races, ethnic backgrounds, sexual orientations, and faiths or religions in a manner that recognizes, affirms, and values the work of the individuals, families, tribes, and communities and protects the dignity of each.” (Child Welfare League of America, 2002) Individual level- engage in actions or create conditions that maximize the optimal development of clients and client systems Organizational and societal level- develop theories, practices, policies, and organizational structures that are responsive to all groups (Stately & Clark, 2003) Cultural Destructiveness Cultural Incapacity Cultural Blindness Cultural Pre-Competence Cultural Competence Advanced Cultural Competence (Cross, Bazron, Dennis, & Isaacs, 1989) Cultural destructiveness: assumes one race or culture is superior to another, e.g. social or medical experiments without knowledge or consent Cultural incapacity: unconscious bias, paternalistic posture, may support segregation, disproportionately applies resources (Cross, Bazron, Dennis, & Isaacs, 1989) Cultural blindness: believes ethnicity or race makes no difference, views self as unbiased yet is ethnocentric in service delivery, views minorities as culturally deprived, encourages assimilation Cultural pre-competence: commitment to civil rights, realizes weaknesses and makes attempts to improve, hires staff that match the service population but may be only token efforts (Cross, Bazron, Dennis, & Isaacs, 1989) Basic cultural competence: accepts and respects difference, continuously self-assesses, adapts service models, seeks advise and input from minority communities and includes informal supports Advanced cultural competence: holds culture in high esteem, seeks to add to knowledge base, advocates continuously for cultural competence across service systems (Cross, Bazron, Dennis, & Isaacs, 1989) Accept: Learn: ALERT Model Explain: for Service Providers Respect: Train: Accept the family’s beliefs, values, & practices, even if you don’t agree Learn about the culture of the community and the individual families you serve; ask questions rather than assuming you know Explain to families why you need information, why time & appointments are important, & how their child will benefit Respect the family’s cultural ideas, beliefs, values & practices. Find culturally appropriate ways to show respect Support & elicit the participation of families in the education & training of providers Multi-Cultural Panel Discussion on HelpSeeking Behavior How does the family talk about illness? What questions are asked of a person who doesn’t feel well? Who in the family decides what to do for a sick family member? Where or who does the family go to for help outside the home? What kind of help is sought? What kind of service provider is most often contacted? What do family members believe about the help they will get at a medical facility? Where do they go in emergencies? How do families talk about insurance, financial, or legal status? How do families address any literacy or linguistic challenges? What are the most difficult barriers to accessing medical services for someone from your background? What is the worst situation you’ve ever seen that limited access to services for someone from your background? What is the best situation you’ve seen that facilitated access to services for someone from your background? Increasing Access to Services for Culturally Diverse Families: Organizational Cultural Competence “A set of congruent behaviors, attitudes, and policies that come together in an agency that enables employees to work effectively in cross-cultural situations.” (Cross, Bazron, Dennis, & Isaacs, 1989) “A culturally competent program possesses the skills and abilities to work effectively with diverse populations. This is demonstrated by serving particular subgroups of the larger population in a way that understands, is relevant to and respects the unique features, cultural beliefs, language and lifestyles within these populations” (Amherst H. Wilder Foundation, 2002) Increasing Accessibility of Mental Health Services to Culturally/Linguistically Diverse Populations Definition: Within a framework of addressing mental health disparities in a community, the level of a human service organization’s/system’s cultural competence can be described as the degree of compatibility and adaptability between the cultural/linguistic characteristics of a community’s population AND the way the organization’s combined policies and structures/processes work together to impede and/or facilitate access, availability and utilization of needed services/supports (Hernandez,& Nesman, 2006). Degree of compatibility defines level of organizational/systemic cultural competence Community Context Cultural/Linguistic characteristics of a community’s population(s) Compatibility Outcomes: Reducing mental health disparities Organization’s/System’s Infrastructure Domain/ Functions Direct Service Domain/ Functions Hernandez, M., & Nesman, T. (2006). Cultural/Linguistic characteristics of a community’s population(s) Compatibility Cultural View of Health History Language Characteristics Resource Characteristics Strength Characteristics Needs Characteristics An organization’s/system’s combined policies, structures and processes Hernandez, M., & Nesman, T. (2006). Compatible Organizational Strategies Infrastructure Domain • Organizational Values • Policies/Procedures/ Governance • Planning/Monitoring/ Evaluation • Communication Compatibility between the • Human Resources infrastructure and direct Development service functions of an • Community & organization Consumer Participation • Facilitation of a Broad Service Array • Organizational Infrastructure/ Supports- language, technology, etc. Direct Service Domain Access The ability to enter, navigate, and exit appropriate services and supports Utilization Availability Appropriate rates of use of needed mental health services Services and supports exist in sufficient range and capacity to meet the needs of the population Hernandez, M., & Nesman, T. (2006). Specific behaviors, knowledge, attitudes, policies, and procedures that demonstrate: Acceptance, respect, regard, flexibility, knowledge about culture and ethnicity • Working effectively when faced with cultural differences including: Responding effectively, linguistic competence, improving access to and quality of care for underserved • Congruence across system components/levels: Policies and procedures that enable effective work in cross/multi-cultural situations at all organizational levels • Self-assessment and quality assurance • On-going development of knowledge, resources, and service models: Knowledge and skills to use appropriate assessment and treatment methods • (Cross, Bazron, Dennis, & Isaacs, 1989) Organizational Cultural Competence: Assessment of Progress Awareness of one’s own and others’ culture (beliefs, values, assumptions), and one’s own prejudices & stereotypes Knowledge about and sensitivity to diverse clients being served (e.g., epidemiology, social context, resources, etc.) Developing appropriate service strategies and techniques (e.g. cross-cultural communication skills, openness, flexibility & adaptability, knowing when interpretation is needed, etc.) (Seeleman, Suurmond, & Stronks, 2009; Stately & Clark, 2003; Suh, 2004; ) Acknowledgement of culture Ongoing assessment ◦ Observable behaviors & attitudes demonstrate acceptance, respect, regard, flexibility, & knowledge about communities served. ◦ Policies, procedures, & documents demonstrate acceptance, respect, regard, flexibility, & knowledge about communities served. ◦ Ongoing self-assessment of cross-cultural relations ◦ Ongoing quality assurance (Cross, Bazron, Dennis, & Isaacs, 1989; Harper, Hernandez, Nesman, Mowery, Worthington, & Isaacs, 2006) Responsiveness to cross-cultural dynamics Cultural knowledge development ◦ Organization recognizes and responds effectively to cross-cultural issues that impact access to care ◦ Linguistic adaptations meet client needs ◦ Organization facilitates equal access to and utilization of quality care ◦ Ongoing development of knowledge about characteristics of communities served ◦ Ongoing assessment of organizational compatibility with the communities served (Cross, Bazron, Dennis, & Isaacs, 1989; Harper, Hernandez, Nesman, et al., 2006) Adaptation for compatibility ◦ Adaptations are made to policies and procedures to increase compatibility with community characteristics ◦ Input and feedback is regularly sought from community members & clients ◦ Infrastructure supports the delivery of compatible & effective direct services ◦ Outcomes are meaningful to providers, families, & community members (quality of life, satisfaction with services, treatment effectiveness, costs effectiveness, etc.) (Cross, Bazron, Dennis, & Isaacs, 1989; Harper, Hernandez, Nesman, et al., 2006) Avoid stereotyping- culture is not static, and varies by individuals and families, it’s not a single variable, it’s a dynamic process Attention to culture may be interpreted as intrusive or singling out as “different” (i.e., not normal, an outsider) Cultural assumptions may hinder practical understanding (e.g., access may be hindered by work hours rather than cultural beliefs) Medical terms can stigmatize- use culturally appropriate explanations & terms, ask “What do you call this problem?” Don’t assume that health goals are the same, ask “What matters most to you?” (Kleinman & Benson, 2006) More effective, holistic care for diverse patients Improved quality of life of patients Increased health care satisfaction Improved perception of health care providers Better adherence to prescribed treatments Personal & professional growth of health care providers Improved quality of care Improved provider-patient rapport Treatment effectiveness Cost effectiveness (increased adherence, reduced emergency care) Reduced disparities in health outcomes for diverse groups (Suh, 2004) Linking Refugee Children to Services in the Community What cross-cultural issues are identified? How has the organization developed knowledge about the population? How has the organization facilitated access to services? How does the organization determine its effectiveness in serving the population? Using a Cultural Competence Assessment Tool Cognitive Domain ___ Cultural awareness- appreciation and sensitivity to values, beliefs, lifeways, practices, & problem-solving strategies of clients ___ Cultural knowledge- learning about other cultures’ worldview, languages, & social contexts through cultural immersion or extensive training Affective Domain ___ Cultural sensitivity- intentional and affective perception of cultural diversity and respect for cultural differences (Suh, 2004) Behavioral Domain ___ Ability to conduct cultural and physical assessments & communicate cross-culturally to learn patients’ cultural beliefs, values, and practices & determine proper interventions Environmental Domain ___ Cultural encounter experience with patients of different cultural backgrounds, either in cultural immersion or international programs (Suh, 2004) Organizational Values _____ Cultural competence is incorporated into the organization’s mission statement _____ Staff is familiar with and understands cultural competence in the organization _____ Organizational leadership and staff say cultural competence is important Policies, Procedures, & Governance _____ Policies and procedures include cultural and linguistic competence. _____ Policies and procedures in the principal language of the client. _____ Administrators, the board of directors, and committees support culturally competent practices. _____ Proportional representation of diverse group members at all levels. Planning, Monitoring, & Evaluation _____ Baseline information on cultural groups is collected _____ Ongoing awareness of cultural group characteristics _____ Cultural competence plan is updated annually. _____ Cultural competence planning involves staff and clients. _____ Systematic collection of information about groups served and staff demographics. _____ Monitoring of access to and quality of services for all groups served. _____ Programs fit the cultural and historical aspects of communities and staff Communication _____ Leadership communicates with staff about cultural competence. _____ Community feedback is solicited and responded to. _____ Organization décor and written materials communicate a culture-affirming message. _____ Staff able to communicate effectively in ways that are easily understood by diverse audiences. _____Targeted outreach activities to communicate health care information in appropriate languages & literacy levels. Human Resource Development _____ Diverse staff recruited with knowledge of community served. _____ Diverse staff retained and promoted equitably. _____ Staff knowledgeable about federal and state statutes and regulations for cultural and linguistic competence. _____ Staff evaluated on cultural and linguistic competence for promotion. _____ Bilingual interpreters assessed for ability to accurately translate in health settings. Community and Consumer Participation _____ Organizational leadership and staff collaborate with clients and community members in developing culturally competent services. _____ Staff participates in cultural functions and community education activities. _____ The organization purchases goods and services from community-based and minority businesses. _____The organization values the opinions of clients, & solicits feedback. _____Staff involved in community advocacy for social issues. Facilitation of a Broad Service Array _____Services are appropriate for community culture & incorporate strengths in all aspects of care. _____ Services are accessible, facilitate’ use, & provide for continuity of care. _____ Facilitates obtaining health education materials & other resources in appropriate languages. Organizational Resources _____Database systems, set up to support planning, monitoring, and evaluating services for diverse clients, including tracking disparities. _____Financial resources support cultural competence, such as diversity training or compensation for bilingual capacity. _____Communication resources support cultural and linguistic competence through appropriate technologies and staffing (e.g., interpreters, etc.). _____ Culturally/linguistically appropriate educational media, forms, literature, and service directories. Mission statement, other documents Website & other media Outreach activities Attendance records for meetings Meeting minutes Participant evaluation/satisfaction surveys Personnel files Clinical records; case records MIS data Opinion surveys Participant observation (journal) Interviews with staff; administrators; community members A developmental process: Cultural competence is a goal toward which professionals, agencies, and systems can strive; it can be learned & improved A continuum: Responses to cultural difference move back & forth along the continuum, varying for individuals, groups, points in time, & contexts An ongoing process: It is active, developmental, iterative, and aspirational rather than achieved http://rtckids.fmhi.usf.edu/ rtcpubs/CulturalCompetenc e/porch/default.cfm http://rtckids.fmhi.usf.edu/ rtcpubs/CulturalCompetenc e/services/default.cfm http://rtckids.fmhi.usf.edu /rtcpubs/CulturalCompete nce/protocol/default.cfm Betancourt, J.R., & Green, A.R. (2010). Linking cultural competence training to improved health outcomes: Perspectives from the field. Academic Medicine, 85, 4: 583-585. Callejas, L.M., Hernandez, M., Nesman, T., and Mowery, D. (2010). Creating a front porch in systems of care: Improving access to behavioral health services for diverse children and families. Evaluation and Program Planning 33,1:32-35. Cross, T., Bazron, B., Dennis, K., & Isaacs, M. (1989). Toward a culturally competent system of care: A monograph on effective services for minority children who are severely emotionally disturbed. Washington, DC: National Technical Assistance Center for Children’s Mental Health. Harper, M., Hernandez, M., Nesman, T., Mowery, D., and Worthington, J., Isaacs, M. (Eds.) (2006). Organizational Cultural Competence Assessment: A Review of Assessment Protocols (Making Children’s Mental Health Services Successful series, FMHI pub. No. 240-2). Tampa, FL: University of South Florida, Louis de la Parte Florida Mental Health Institute, Research & Training Center for Children’s Mental Health. Available: http://rtckids.fmhi.usf.edu/rtcpubs/CulturalCompetence /protocol/default.cfm Hernandez, M., Nesman, T., Isaacs, M., Callejas, L. M., & Mowery, D. (Eds.). (2006). Examining the research base supporting culturally competent children’s mental health services. Tampa, FL: USF, Louis de la Parte Florida Mental Health Institute, Research & Training Center for Children’s Mental Health. Hernandez, M., Nesman, T., Mowery, D., AcevedoPolakovich, I. D., and Callejas, L. M. (2009). Cultural competence: A review and conceptual model for psychiatric and mental health services. Psychiatric Services, 60, 8:1046-1050. Kleinman, A., & Benson, P. (2006). Anthropology in the clinic: The problem of cultural competency and how to fix it. PLOS Medicine 3, 10: 1673-1676. Seeleman, C., Suurmond, J., & Stronks, K. (2009). Cultural competence: A conceptual framework for teaching and learning. Medical Education 43: 229-237. Siegel, C., Davis-Chambers, E., Haugland, G., Bank, R., Aponte, C., & McCombs, H. (2000). Performance measures of cultural competency in mental health organizations. Administration and Policy in Mental Health 28, 2:91-106. Stately, A.L., & Clark, R.L. (2003). AIDS Project Los Angeles & United American Indian Involvement, Inc. Suh, E.E. (2004). The model of cultural competence through an evolutionary concept analysis. Journal of Transcultural Nursing 15: 93-102. U.S. Department of Health and Human Services [DHHS]. (1999). Mental health: A report of the Surgeon General. Rockville, MD: Author. World Health Organization. (2001). The World Health Report 2001. Mental Health: New Understanding, New Hope. France. http://www.who.int/entity/whr/2001/en/whr01_en.pdf