I. A. B. C.
advertisement

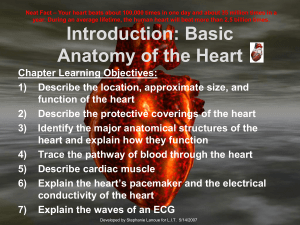
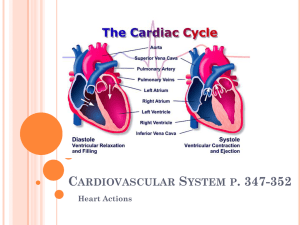
1 Anatomy & Physiology 34B Chapter 18 - The Heart I. Overview A. Location of the Heart B. Circulatory Routes Through the Heart C. Conduction System of the Heart D. Heart Sounds E. Cardiac Cycle F. Cardiac Output G. Differences in Fetal Circulation II. Location & General Description of the Heart A. The heart is located in the thoracic cavity between the lungs in the _______________, about 2/3 left of the midline B. Heart functions include 1. Right (_____________) side pumps oxygen poor blood to the lungs for oxygenation 2. Left (___________) side pumps oxygen & nutrient rich blood to the body tissues A. The 4 chambered, muscular heart is about the size of a fist 1. Its ______ is pointed downward & resting on the diaphragm 2. Its ______ is the large superior end where the vessels attach C. The parietal _____________ is a sac that encloses and holds the heart in place. 1. The pericardium consists of a tough outer ________ pericardium and inner _________ pericardium. 2. Serous pericardium is composed of a ____________ layer and a ________ layer, and produces serous (pericardial) fluid 3. Between the parietal and visceral layers is the pericardial ________, a potential space filled with serous fluid that reduces friction between the membranes. 4. _________________ is an inflammation of the pericardium. Associated bleeding into the pericardial cavity compresses the heart (cardiac tamponade) and can be lethal. D. Heart Wall - has 3 layers 1. ____cardium (visceral pericardium) - outermost heart wall consisting of mesothelium and connective tissue. 2. 3. ____cardium - middle layer of heart wall composed of cardiac muscle tissue. 4. _____________ is an inflammation of the endocardium, usually due to bacterial infection ____cardium - innermost heart wall consisting of endothelium and areolar connective tissue. 2 III. Heart Chambers & Valves A. Four chambers include 2 upper atria and 2 lower ventricles 1. L. & R. _______ have thin muscle walls a. ____________ muscles make atria surfaces rough b. The _________ is an earlike appendage on surface of the atrium that increases atrial volume. c. An interatrial _____ separates L. & R. atria; the fossa ovalis (remnant of fetal foramen ovale) is found in this septum d. Both atria contract simultaneously and empty blood into the ventricles though atrioventricular (___) valves (R.= __________; L. = _________ or mitral) e. These valves are secured via chordae _________ tendons attached to _________ muscle outgrowths of the trabeculae carneae myocardium in the ventricles 2. L. & R. ___________ have thicker walls a. Internal surface is wrinkled due to trabeculae ________ (myocardium covered by ______cardium) b. c. _____ ventricle wall is thickest, to pump blood throughout body. d. An interventricular ________ separates the ventricles. Both ventricles contract simultaneously, pushing blood through semilunar (___) valves (L. = ________; R. = ___________) into the aorta & pulmonary artery IV. Circulation - pathway of blood through the heart to lungs & body A. ___________ Circulation progresses in the following sequence: 1. ___________ blood from lungs returns to heart via _________ veins. 2. Pulmonary veins feed blood into the left __________. 3. Contraction of L. atrium pushes blood through the ________ valve into the L. 4. ___________ Contraction of L. ventricle pushes blood through the aortic semilunar valve into the _________ (largest artery in the body), which then feeds blood to: 5. Arteries arterioles capillaries, from which ___ is delivered to body tissues and ____ is picked up. 6. Deoxygenated blood flows from capillaries venules veins and returns to heart via the superior & inferior ______ _________ (largest veins in body). B. ___________________ Circulation 1. Deoxygenated blood, high in ____, is delivered to the R. ________ (via superior & inferior vena cava). 2. Contraction of R. atrium pushes blood through the ___cuspid valve into R. _____________. 3 3. Contraction of R. ventricle pushes blood through the pulmonary semilunar valve into the ____________ trunk, which branches into L. & R. pulmonary arteries that take blood to _______. 4. In lungs, blood flows through arteries arterioles capillaries where blood releases ____ and picks up ____. 5. Oxygenated blood then returns to the heart via venules pulmonary _______. C. ___________ Circulation - blood supply to & from heart tissue 1. Coronary (atrioventricular) ______ - external groove between atria and ventricles; contains L. & R. coronary arteries 2. Coronary __________ emerge from the base of the aorta and deliver oxygenated blood to heart tissues. a. ______ coronary artery (in coronary sulcus) branches into 1) Anterior ______________ (widow maker) artery passes down the anterior interventricular sulcus, delivering blood to the left ventricle walls 2) _____________ artery passes around the heart in the left atrioventricular sulcus b. ______ coronary artery (in coronary sulcus) branches into 1) __________ interventricular artery passes through the posterior interventricular sulcus 2) ____________ artery on the lateral right ventricle 3. Coronary ______ take deoxygenated, high CO2 blood away from heart tissues. a. b. Coronary _______ - largest vein on posterior surface of heart; empties into R. atrium Blood is brought to the coronary sinus primarily by the 1) _____ cardiac vein (near L. anterior interventricular art.) 2) _________ cardiac vein (near post. interventricular art.) 4. ___________ of a coronary artery due to cholesterol plaque or blood clot can lead to a. _________ – loss of blood flow (oxygen) to the affected area b. __________ pectoris – pain or heaviness in the chest, often accompanied by radiating pain into the jaw &/or left arm c. Myocardial __________ - heart attack and possible death 5. Coronary artery _____________ can be alleviated by a. Coronary __________ surgery in which blood vessels are grafted onto the heart to bypass the blocked artery b. Balloon ____________ in which a catheter is inserted into the blocked artery and a balloon inflated to compress the blockage. V. _________ System of the Heart - consists of interconnected strands of specialized cardiac muscle/nerve tissue that conducts electrical impulses through the heart, coordinating contractions. Components A. Cardiac muscle relies almost entirely on aerobic cellular respiration; the cells are connected end to end by _____________ _______ with the following features 4 1) Interdigitating _______ of the plasma membrane that interlock the cells together 2) ___________ & fascia adherans junctions that prevent the cells from pulling apart during contractions 3) _____ junctions – protein channels that allow Ca2+ ions (electrical impulses) to flow freely from cell to cell B. Sinoatrial (___) node - the “_________;” sets HR at 70-80 bpm 1) Found in R. _____ posterior wall, inferior to superior vena cava 2) Initiates the cardiac cycle by producing an electrical impulse that spreads over both _______, causing contraction 3) Atria ___________ an instant after receiving the impulse from the SA node (ventricles are relaxed = __________) 4) The impulse then passes along the ____________ pathway to C. Atrioventricular (___) node - in the lower interatrial septum between the atrium and ventricle; it passes impulse to D. Atrioventricular bundle (bundle of ___) - extends from AV node into interventricular septum; this passes impulse to E. L. & R. ________ _________ - extensions of AV bundle down the L. & R. sides of the septum; these pass impulse to F. __________ fibers - extend from the branches into the ventricular walls; Impulses through C, D, & E cause ventricular contraction (called ________) G. An electrocardiogram (____) records the electrical impulses through the heart as waves labeled P, Q, R, S, T: 1. 2. 3. ___ wave = SA node depolarization, which causes atrial contraction 4. 5. ___ wave = ventricular repolarization, which causes ventricular relaxation 6. ____ interval (from end of T wave to beginning of P wave) - time in which the ventricles are relaxing and filling with blood. 7. Note: atrial ______________ also occurs, but the small wave is obscured by the QRS complex. 8. Heart rate (___) is timed from the peak of one P wave to the next P wave a. Normal resting HR is about ___-___ beats per minute (bpm) b. _________cardia is a resting HR of _____ bpm or more c. _________cardia is a HR of less than ___ bpm 9. _____ complex = ventricular depolarization, which causes ventricular contraction _____ segment (from end of P wave to beginning of Q wave) represents the AV node delay (between SA node and AV node depolarization) ____ segment (from end of S wave to beginning of T wave) - time in which ventricles are contracting and emptying. EKGs can be used to ____________ abnormal heart rates, arrhythmias, and damaged heart muscle 5 VI. Physiology of Heart Electrical Activity A. ______ rhythm – normal heart rate is 70-80 bpm, triggered by the __ node; vagus nerves inhibit myocytes at rest to maintain this rate B. Damage to the SA node can cause other nodal tissues (e.g., AV node) to set the heart rate at a slower 40-60 bpm (________ rhythm) C. Any abnormal cardiac rhythm is called _______________; such as 1. Atrial ________ - impulse waves circulate within the atrial myocardium; result is rapid atrial contractions (200 bpm) 2. Heart ________ – atria contract regularly, but the ventricles occasionally fail to be stimulated to contract after atrial contraction; due to a damaged conduction system 3. Ventricular __________ - ventricles contract rapidly in a weak, uncoordinated manner; caused by a damaged conduction system; can result in death if not corrected quickly D. Cardiac muscle cells can contract without input from the _______ system. The two types of cardiac cells are autorhythmic cells and contractile myocytes 1. ____________ cells, such as those found in heart nodal tissue, initiate action potentials (and heart beats) in the following sequence a. __________ potential begins at –60 mV and rises to ________ (-40 mV) due to an influx of Na+ through Na+ If channels b. _______________ occurs at threshold as voltage-gated ____ channels open, and Ca2+ rushes into the cell from the ECF c. _____________ occurs at about 0 mV when __ channels open, causing K+ to move out of the cell. d. When repolarization is complete, K+ channels close and the ____________ potential begins again 2. __________ myocytes are stimulated by the autorhythmic cells and continue the action potential throughout the heart in the following manner a. ___ junctions transport Ca2+, Na+, and K+ from autorhythmic cell to contractile cell, triggering the opening of voltage-gated Na+ channels b. Depolarization occurs as ___ rushes into the cell, triggering the opening of voltagegated Ca2+ channels c. ____ moves into the cell and opens ligand-gated (ryanodine) Ca2+ channels in the sarcoplasmic reticulum (SR) d. Ca2+ from the ___ binds to troponin and triggers contraction as in skeletal muscle (recall the sliding filament theory) e. Repolarization occurs as ___ moves out of the cell through K+ channels and Ca2+ channels close f. ______________ of cells occurs as Ca2+ dissociates from troponin and is transported back into the SR via Ca2+-ATPase pump, and to the ECF via Na+-Ca2+ antiporters h. Resting Na+ and K+ concentrations are restored by the Na+/K+ ________ pump E. Autonomic neurotransmitters ________________ cardiac contractile force and heart rate 1. Cardiac muscle contraction force depends on the number of ________________ formed between myosin and actin, which depends upon how much Ca2+ is bound to troponin 2. Low cytosolic ______ concentrations result in fewer crossbridges and weaker cardiac contraction 6 3. ________________ and NE (sympathetic) bind to cardiac ____ adrenergic receptors, and activate cAMP, which a. Phosphorylates and opens voltage-gated _____ channels, resulting in stronger cardiac contraction b. cAMP binds to open ____ channels, so they remain open longer, speeding up depolarization and heart rate 4. The speed at which autorhythmic cells ______________ determines heart rate, and can be modified by altering cellular _____________ to ions a. Increased permeability to _____ and/or _____ during the pacemaker potential will speed depolarization and heart rate. b. Decreased Ca2+ permeability or increased _____ permeability will slow depolarization and heart rate 5. ___________________ (parasympathetic) stimulation slows heart rate by a. ACh binds to cardiac ____________ cholinergic receptors that influence Ca2+ and K+ channels in autorhythmic cells b. Increase in K+ permeability ________________ the cells c. Decrease in Ca2+ permeability slows the rate at which autorhythmic cells ___________ VII. Heart Sounds A. “Lub-dup” heart sounds are caused by the opening and closing of heart ________ 1. 2. The “lub” is caused by the closing of ____ valves, when the ventricles contract at ___________ The “dup” is caused by the closing of the __________ valves, when the ventricles relax at the beginning of ___________ B. Body areas at which the valves may be listened to are called valvular ______________ areas, and include: 1. 2. 3. 4. __________ valve - 2nd intercostal space right of sternum ___________ valve - left, 2nd intercostal space left of sternum _____________ valve – just right of the sternum in the 5th intercostal space _____________ valve – 5th intercostal space left of the sternum in line with the midclavicle. C. Heart ________ are caused by valve leakage or restriction and the turbulence of the blood as it passes through the heart. Four types of murmurs are: 1. Valvular ____________ - heart valves do not form a tight seal; causes a blowing sound after the valve closes 2. ___________ - walls surrounding a valve are roughened or constricted; stiffened valves don’t open properly; produces a “click” sound during ventricular systole 3. Mitral valve _______ - inherited weakness of valve collagen & chordae tendinae that allows blood backflow through valve into atrium during systole; detected by a click followed by a swish 4. ________ murmur - caused in children by the blood turbulence during heavy exercise; not serious 7 VIII. The _________________ (one contraction & relaxation) involves pressure changes in the heart and the way the pressure changes affect the heart valves and blood flow. The three phases include A. _____________ filling (in mid to late ventricular diastole) 1. Blood flows passively into atria, through open ____ valves, into ventricles 2. ____ contract (__ wave), forcing remaining blood into ventricles 3. End diastolic volume (___) in ventricles is about 130 mL B. Ventricular __________ 1. ____________ contraction – ventricles contract (____ wave) and interventricular pressure rises, closing AV valves; atria relax 2. Ventricular _________ – ventricular pressure forces SL valves open, blood is ejected into pulmonary trunk and aorta a. Each ventricle ejects a _______ volume of about 70 mL b. The blood remaining behind (60 mL) is the end diastolic volume (____). [SV = EDV-ESV] C. Isovolumetric ______________ – ventricles relax (__ wave), interventricular pressure drops, some blood flows backward, SL valves close. Cycle then repeats. D. _________ heart failure results from the failure of either ventricle to eject blood effectively, usually due to heart disease; causes are pulmonary or systemic edema XI. _______________ is the amount of blood ejected by each ventricle per minute A. Cardiac output (CO) is the product of heart rate (HR) and stroke volume (SV): [___ = ___ x ___], and averages about 5.25 L/min (total blood volume in the body is 4-6 L) B. Normal adult HR averages about __ bpm. C. Normal stroke volume is about ____ ml D. What would the normal cardiac output be? _______________ L/min E. __________ is raised by positive chronotropic agents and lowered by negative chronotropic agents in the autonomic nervous system 1. __________ oblongata contains a sympathetic cardioaccelatory center and a parasympathetic cardioinhibitory center a. Cardio_____________ center nerves secrete norepinephrine, which ______ HR & increases CO b. Cardio_______ center sends nerve impulses to the SA & AV nodes via the _____ nerves, which secrete ACh, slowing HR to the normal rate 2. _______ceptors in muscles and joints inform the cardiac center of changes in physical activity 3. _____receptors (pressure receptors) in the aorta and internal carotid arteries send signals to the cardiac center if BP drops or rises, increasing or decreasing HR to compensate 4. ______receptors in aortic arch, carotid arteries, and medulla, sense changes in blood pH, CO2, and O2 and alter HR 5. ________ medulla secretes epinephrine and norepinephrine in response to arousal, stress, and exercise, which increases HR 6. Other substances, such as __________, nicotine, and thyroid hormone increase HR 7. Electrolytes, such as Ca2+ and especially ___ ions, can increase or decrease HR 8 F. ____________________ is governed by three factors: preload, contractility, and afterload 1. ___________ is the amount of tension in the ventricular myocardium just before it begins to contract; this increases with physical activity – the more ventricles are stretched with increased blood flow, the harder they contract a. Frank-_____________ law – the more blood there is in a ventricle at the beginning of a contraction (increased EDV), the greater the stroke volume b. _______ is determined by venous return of blood to the heart, which is affected by 1) Skeletal ___________ contractions 2) ________________ contractions (respiratory pump) 3) Constriction of veins by ________________ NS activity 2. _______________ – contractile force of the myocardium for a given preload. a. ___________ ionotropic factors, such as Ca2+, epinephrine, norepinephrine, and glucagon _________ contractility and SV b. __________ ionotropic factors, such as low Ca2+ and the vagus nerves _____________ contractility and SV 3. ___________ is the blood pressure in the arteries just outside the SL valves, which opposes the opening of the valves. Increased afterload __________ stroke volume E. _______ influences cardiac output via its effects on proprioceptors and on the venous return to the heart. Habitual exercise increases ventricular size and stroke volume, and reduces the resting HR. XII. Differences in __________ Circulation A. Shunts Away from the _____________ Circuit 1. Foramen _______ - hole (valve) in the interatrial septum that diverts some blood from the R. atrium to the L. _____; this closes at birth to become the __________ 2. ________ arteriosus - short artery that diverts blood from the pulmonary trunk to the ________; closes at birth to become the ____________ arteriosum B. Fetal Vessels to & from the Placenta 1. The _________ is a shared structure of the fetus and mother across which nutrients & ____ diffuse from mother to child and wastes & ____ diffuse from fetus to mother 2. Paired umbilical _________ branch from internal _______ arteries and carry deoxygenated blood to the placenta to pick up oxygen & nutrients 3. A single umbilical ______ returns the oxygenated blood to the fetus’ hepatic portal vein or through the ductus _______, where it proceeds directly into the hepatic veins, to the inferior vena cava and right atrium. a. At birth, the umbilical vein becomes the ligamentum ________ b. The ductus venosus becomes the ligamentum __________