Supplementary material
advertisement

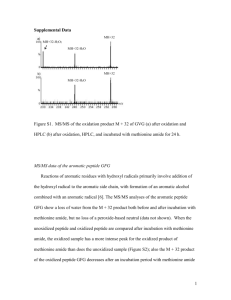
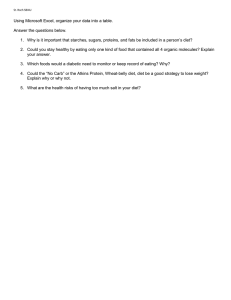
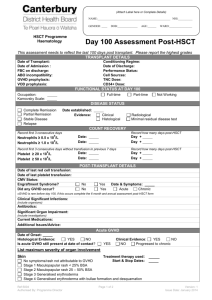
Supplementary material Supplement to: Staufner C et al, Adenosine kinase deficiency: expanding the clinical spectrum and evaluating therapeutic options, Journal of Inherited Metabolic Disease 2015. I. Case reports II. Supplementary tables and figure Table S1. Anthropometrical data at birth and at last assessment Table S2. Biochemical response to low methionine diet in patient 7 Figure S1. Impact of low methionine diet on liver function and methionine levels I. Case reports Case report family I (patient 1 and 2) Family I is a consanguineous Turkish family with four children; patient 1 is the oldest and patient 2 the youngest child, the other two children are healthy. Patient 1 is a girl delivered at 36+4 weeks of gestation by caesarean section due to pathological CTG. Birth weight was normal for gestational age. Cyanosis was noted at 4 hrs post-delivery with hypoglycemia (blood glucose not detectable) and hypothermia (35.1 °C). Glucose infusion of up to 16mg/kg/min was needed to stabilize blood glucose levels and insulin was high during hypoglycemia (blood glucose 1.67 mmol/L, insulin 30.9 mU/L), so hyperinsulinism was diagnosed. From the second day of life she received phototherapy due to hyperbilirubinemia. There was mild liver dysfunction with an increase of transaminases and INR but no cholestasis. Hyperinsulinism was responsive to diazoxide. Because of mild hypothyroidism, supplementation with L-thyroxine was started. Methionine concentrations were mildly and intermittently elevated (max. 107 µmol/L), whereas concentrations of AdoMet and AdoHcy were markedly and consistently elevated in plasma (AdoMet 355 nmol/L; AdoHcy 224 nmol/L) and CSF (AdoMet 384 nmol/L; AdoHcy 218 nmol/L). Recurrent mild to moderate hyperammonemia (80-140 µmol/L) was observed but could not be explained. Echocardiography revealed a perimembranous ventricular septum defect (VSD), persistent ductus arteriosus (PDA) and persistent foramen ovale (PFO). Because of hemodynamic decompensation, cardiosurgical correction of the defects became necessary at the age of 4 months. By that time patient 1 showed hepatomegaly, severe muscular hypotonia without head control, severe global developmental delay and frontal bossing. Epilepsy developed at the age of 5 months. Liver function had nearly normalized but treatment with diazoxid was needed to control hyperinsulinism. At the age of 7 months, liver biopsy showed periportal and intralobular fibrosis with low grade parenchymal fat and no signs of cholestasis. At the age of 15 months, patient 1 died due to a pulmonary infection. Patient 2 (male) was born at term as the 4th child of family I with normal birth weight. On his first day of life, he presented an episode of cyanosis and bradycardia and hypoglycemia of 0.56 mmol/L was detected. Infusion of glucose 10 mg/kg/min was needed to stabilize blood sugar levels and hyperinsulinism was detected in the further workup (blood glucose 1.17 mmol/L; insulin 4.3 mU/L), responsive to diazoxide. The patient showed muscular hypotonia and hepatomegaly. From day 3 on, cholestatic hyperbilirubinaemia, increased transaminases and severe liver dysfunction presented (see table 2 for maximum values). Hypermethioninemia was detected (methionine 176 µmol/L at day 6; 400 µmol/L at day 34). A low methionine diet was initiated, but was discontinued after 5 days because of lacking clinical and biochemical response. Notably, methionine concentrations spontaneously normalized in the course of the disease. Echocardiography revealed a persistent arterial duct (PDA) and an atrial septum defect (ASD), which both resolved spontaneously. Liver biopsy at the age of 1 month showed severe portal, septal and perisinoidal fibrosis with transition to cirrhotic rearrangement with pronounced ductal reaction and incipient sings of chronic cholestasis, and hardly viewable extra hepatic bile ducts. Liver function recovered under symptomatic treatment, but there was neurological impairment with muscular hypotonia and global retardation. Clinical seizures were first observed at the age of 4 months, but EEG has already been highly pathologic during the newborn period. At the age of 2.5 years, frontal bossing was noted. Treatment with diazoxide was stopped at the age of 2.7 years, but single hypoglycemic episodes were still noted in the further course. At time of report, the patient is 7 years old. He is a happy and cooperative boy, but there is severe global developmental retardation; he has a hypotonic-dystonic movement disorder with changing muscle tone. He has no speech but communicates with sounds and gesticulation. His developmental age is 2-4 months (according to DENVER testing). He is wheel chair bound and fed through a percutaneous gastrostomy. He is nearly blind because of retinal dystrophy. He is free of seizures on therapy with lamotrigin and phenobarbital. Liver function is normal. Orchidopexia was performed due to maldescensus testis on both sides. Methionine levels are normal but plasma AdoMet and AdoHcy and urine adenosine are increased. After ADK deficiency had been published, genetic testing of the ADK gene was performed and revealed a homozygous missense mutation (c.905 T>C, p.Phe302Ser). The same mutations could be confirmed in DNA from fibroblasts of patient 1. Case report family II (patient 3) Family II is a consanguineous Turkish family with 7 children and is related to family I, as the father of patient 1 and 2 is brother of patient 3. Patient 3 is a girl born at term who presented on her first day of life with severe hypoglycemia (0.39 mmol/L). Blood glucose stabilized quickly after glucose infusion. On her 2nd day of life she developed hyperbilirubinaemia (total bilirubin 345.3 µmol/L, direct bilirubin 6.8 µmol/L) that remained on the same level till the 8th day of life although intensive phototherapy was applied. Transaminases and gamma-GT were mildly increased (ASAT 85 U/L, gamma-GT 441 U/L), and coagulopathy (INR max. 2) developed within the first week of life. During the neonatal period, truncal muscular hypotonia became evident; eye fixation was inconsistent and social contact not appropriate for age. Partial tube feeding was required. Echocardiography revealed persistent ductus arteriosus, persistant foramen ovale and neonatal coarctation of the aorta, which resolved spontaneously during follow-up. Newborn screening from dried blood spot (DBS) revealed hypermethioninaemia (138 µmol/L, N < 91; day 4 of life), but on day 11 methionine had become normal in DBS (70 µmol/L). Neither amino acid analysis in plasma nor further metabolic work-up were investigated at this stage. Due to cholestatic hyperbilirubinaemia (total bilirubin 230.8 µmol/L, direct bilirubin 70.1 µmol/L) and increased ASAT, ALAT and gamma-GT at the age of 2 months (ASAT 240 U/L and GGT 219 U/L) liver biopsy was performed, showing predominantly lobular hepatitis and a reduced number of bile ducts. Frontal bossing was noticed at 3 months of age. In the further course recurrent asymptomatic hypoglycemia (min 1.22 mmol/L) was noted. In one hypoglyacemic episode ketone bodies were low but insulin was not measured at this time. In an earlier hypoglycemic episode insulin was not detectable. At the age of 5 months, there was a continuous cholestatic icterus and hepatomegaly with increased transaminases but near to normal coagulation (total bilirubin 365.8 µmol/L, direct bilirubin 265.0 µmol/L, ASAT 235 U/L, INR 1.2). Metabolic work up was then initiated and revealed massive hypermethioninaemia (methionine 809 µmol/L) with clearly elevated AdoMet (2299 nmol/l) and moderately increased AdoHcy (187 nmol/L) in plasma. Betaine (trimethylglycine) (995 µmol/L; N 18-41), dimethylglycine (54.6 µmol/L; N 1.8-3.7) and sarcosine/ monomethylglycine (6 µmol/L; N not detectable) were also increased in plasma. At the age of 7 months liver function had further deteriorated (see maximum values in table 2) and hepatorenal syndrome with metabolic acidosis and ascites developed. Low methionine diet was started as experimental therapy with a mean daily intake of 15 mg methionine per kg of body weight. As neither laboratory results nor the clinical situation improved within the first week, the parents decided to take her daughter home but to continue the low methionine diet in an overall setting which was believed to be palliative. In the further months, liver function stabilized and improved until about one year later, liver function had normalized nearly completely (see figure S1). Also concentrations of methionine, AdoHcy, betaine and DMG had normalized whereas concentrations of AdoMet and sarcosine were still above the normal range but had decreased (AdoMet 164 nmol/L, sarcosine 4 µmol/L). At the age of 1.9 years the low methionine diet was stopped but successfully reintroduced one month later, as liver impairment and hypermethioninaemia redeveloped. However, the patient showed severe neurological impairment with pronounced psychomotor retardation. Epilepsy developed at the age of 4.8 years. The low methionine diet was stopped again at the age of 4.9 years and liver function remained stable since then, but there were two episodes with slight increase of transaminases, total bilirubin and methionine with spontaneous normalization within a few days; one of these episodes was triggered by a viral infection. At time of report the patient is 11.75 years old. She has moderate to severe muscular hypotonia and dystonia. She had learned to crawl and was able to walk a few steps without support but has lost these abilities during the last year. She has no speech but communicates on a low level with sounds and gesticulation. Her developmental age is 9-11 months (according to DENVER testing). Apart from frontal bossing and abnormal dentition, slender hands and feet are noticeable. Anticonvulsive treatment has become increasingly challenging and the patient has daily seizures despite a combination therapy with topiramat, levetiracetam and lamotrigin. Patient 3 shares the same homozygous missense mutation as her cousins patient 1 and 2 (c.905 T>C, p.Phe302Ser). Case report family III (patient 4 and 5) Family III is a consanguineous Arabic family from Kuwait with 3 children, two of them affected (patient 4 and 5). Patient 4 was born at term as 1st child of family III with a birth weight of 2300g. She had phototherapy for 2 days to treat hyperbilirubinemia and was discharged home in stable condition. She was re-admitted to hospital at the 12th day of life with severe hyperbilirubinaemia (total bilirubin 427.4 µmol/L, direct bilirubin 128.2 µmol/L), raised transaminases and muscular hypotonia. The patient had recurrent hypoglycemia since infancy, but insulin levels were not checked during hypoglycemia episodes. Due to elevated levels of tyrosine (and methionine), tyrosinaemia type I was suspected although urine succinylacetone was negative and feeding with a Phe-Meth-Tyr free formula was initiated. Repeated blood amino acid examinations showed no significant abnormalities under diet. At the age of 1.2 years liver biopsy had revealed cholestasis with microvesicular fatty degeneration and periportal fibrosis. Ultrasound showed cholelithiasis. Dietary treatment was stopped at that time, after tyrosinaemia type I had been considered very unlikely. Psychomotor development was retarded, but she learned to sit at the age of 3 years and to stand at the age of 5 years. From 3 years of age she was able to speak single words. Epilepsy was diagnosed at the age of 8 years. At the age of 14 years, ADK deficiency was suspected because of an isolated elevation of methionine with a moderate increase of AdoMet and AdoHcy in plasma and elevated adenosine concentration in urine (see table 2 for laboratory values). Molecular genetics revealed a homozygous deletion in exon 3 of the ADK gene (p.30-47del). The patient can walk independently, gait is broad-based and she speaks single words. There is an increased muscular tone of the lower extremities. She is of short stature, shows frontal bossing and has sparse hair. Furthermore, downward slanted palpebral fissures, hypertelorism, a broad nose, low-set ears, and severely distorted teeth are noticeable. Seizures are well controlled with lamotrigin monotherapy. After prolonged fasting she develops episodes of hypoglycemia. Patient 5 was born at term as the 3rd child of family III with a birth weight of 2900g. Due to neonatal hyperbilirubinaemia, she received phototherapy for 10 days. There was muscular hypotonia from birth on. Seizures started at 6 months of age. Recurrent hypoglycemia was first noted when she was 2 years old. It is not reported whether insulin levels were measured. Psychomotor development has been severely retarded. At the age of 5 years, she started to crawl and was able to speak very few single words. ADK deficiency was suspected at the age of 8.3 years, when elevated concentrations of methionine, AdoMet and AdoHcy (all in plasma) and adenosine (urine) were measured (see table 2 for laboratory values). At that time patient 5 was short of stature, showed frontal bossing, hypertelorism and downward slanted palpebral fissures. She can pull herself up, but there is no standing or walking. There is an increased muscular tonus and coarse tremor of the extremities and she shows dystonic movements. She has lost her skill of speaking a few words, uses no speech anymore and has no understanding of words. Electrophysiology shows signs of a mild demyelination polyneuropathy. At the age of 9 years, she had a gall bladder removal because of symptomatic cholelithiasis. She is free of seizures with lamotrigin and levetiracetam. She shares the same homozygous deletion as her older sister. Case report family IV (patient 6 and his three sisters, published by Labrune et al. in 1990) Family IV is a consanguineous Moroccan family with 9 children. The eldest, born in 1978, died at the age of 9 months due to an unknown cause. Three girls of this family were previously reported to have suffered from a syndrome of hypermethioninaemia, liver dysfunction, recurrent hypoglycemia, neurological impairment and facial dysmorphism including a prominent forehead, sparse hair and abnormal teeth. All had become symptomatic on their first day of life. Plasma concentrations of AdoMet and AdoHcy were not measured, but in urine, concentrations of AdoMet were high. A beneficial effect had been observed when a low methionine diet was applied. The cases have been published by Labrune et al. in 1990 as “familial hypermethioninemia partially responsive to dietary restriction” (Labrune, et al. 1990). One of the siblings died at the age of 19 years due to respiratory distress in the course of an influenza infection, the others are alive and 34 and 28 years old at time of report. Both have a severe neurological phenotype with pronounced mental disability: one presenting very severe behavioral disturbances (such as coprophagia), severe epilepsy and schizencephaly on brain MRI (frontal right). She has an asymptomatic cholelithiasis. The other patient is bedbound. Due to the genetically confirmed diagnosis of their brother these siblings can be classified as ADK deficiency. Patient 6, a boy, was born from a twin pregnancy at 36 weeks of gestation with normal birth weight. As he presented severe neonatal jaundice and cholestasis, he was considered to be affected from the same disease as his older sisters, and a low methionine diet was started from the neonatal period on. He had recurrent hypoglycemia; insulin levels are not known. At the age of 9 months, mental retardation was noted. He learned to speak a few words at the age of 5.5 years. There was motor delay and muscle weakness. At the age of 22 years, reintroduction of natural protein and increase of methionine was tried, but led to recrudescence of the liver dysfunction (anicteric cholestasis and cytolysis). Protein was withdrawn a few months later and hepatic function normalized subsequently. At time of report, he is of 24 years old, of short stature but severely macrocephalic (+4 SDS), has frontal bossing, hypertelorism, slender hands and feet, and sparse hair. He did not develop seizures and EEG was repeatedly normal (latest 3 years ago). At time of report, he has severe mental retardation and severe behavioral disturbances. He is hardly able to walk, has muscular atrophy and pyramidal syndrome. He has an asymptomatic cholelithiasis. A homozygous frame shift mutation in the ADK gene was identified (c.685_687 delinsCC, p.Thr229ProfsX16). Case report family V (patient 7) Family V is a consanguineous Italian family from Sardinia with an unremarkable past medical history. Patient 7 was born at term with normal birth weight and became symptomatic with cholestatic jaundice and increase of transaminases in his first days of life. Frontal bossing was noted from birth. There was failure to thrive, and at the age of 2 month, hypoglycemia was noted. Initially, the patient presented with dicarboxylic aciduria when hypoglycemic and he was glucagon unresponsive (most similar to a defect of fatty acid oxidation). At the age of 4 months, he developed a picture compatible with hyperinsulinism. Within his first year of life, he had recurrent bouts of massive cytolysis with coagulopathy (see table 2 for maximum values), but rather mild hyperbilirubinaemia (max. total bilirubin after 3 months of life 39.3 µmol/L). Alfa-fetoprotein was repeatedly massively increased (max. 9014 ng/mL). Methionine has only been measured in few occasions but was highly elevated after the 7th month of age (see figure S1). Muscular hypotonia and global developmental retardation was noted within the first year of life. At the age of one year, a more detailed metabolic workup was done and elevated concentrations of AdoMet, AdoHcy and tHcy were detected (values see table 2), at that time methionine was massively elevated with 1100µmol/L. Liver biopsy showed signs of mild to moderate portal fibrosis at the age of 15 months and sonography revealed a small gallbladder stone. At the age of 2.5 years, he had feeding difficulties, recurrent vomiting, hypoglycemia, neurodevelopmental delay and ataxia. A low methionine diet was started and the showed striking improvement of feeding difficulties with disappearance of vomiting, no further need of tube feeding and almost complete normalization of hypoglycaemia (only occasionally reported after prolonged fasting) and of liver function testing. Improvement of developmental delay and speech was also observed, and the patient reached autonomous gait (but is still ataxic). Under therapy, plasma methionine concentrations, AdoMet, AdoHcy and tHcy could be lowered (see table S2) and AdoMet and AdoHcy were normal in CSF (not measured in CSF before onset of diet). At time of report the patient is 5.25 years old and is free of seizures. Current psychomotor status (according to Griffiths testing) is 2.5 years (IQ 46). Genetic analysis revealed a homozygous nonsense mutation in the ADK gene (c. 199 C>T, p.Gln*67). Case report family VI (patient 8) Family VI is a non-consanguineous German family with unremarkable family history. Patient 8 was born at term with normal birth weight. She became symptomatic within the newborn period with prolonged jaundice. Echocardiography revealed PDA. In the further course, there was mild liver dysfunction, muscular hypotonia and delayed development. Slender hand and feet were noticed when she was 2 years of age and frontal bossing became apparent at the age of 3 years. Elevated concentrations of methionine, tHcy, AdoMet and AdoHcy were measured in plasma. A therapeutic trial with a low methionine diet was initiated at the age of 3.25 years. Concentrations of methionine and tHcy normalized, but there were no significant changes observed clinically, and the diet was stopped one year later. She received phosphatidylcholine from the 3rd – 8th year of life, but no response has been observed. At time of report she is 9.5 years old and has not developed epilepsy. During the last year she had 3 episodes of hypoglycemia in the morning (lowest blood glucose 2.05 mmol/L), which was treated by substitution of complex carbohydrates. She shows moderate global developmental delay and attends a school for disabled children. She speaks fluently but has a reduced vocabulary. Her muscle tone is reduced but she can walk up to one kilometer. Patient 8 is compound heterozygous for a nonsense and a missense mutation in the ADK gene (c.893 C>A, p.Ala298Asp and c.925 C>T, p.Gln309*). Case report family VII (patient 9 and 10) Family VII is a consanguineous Iranian family. Two affected female patients had an uneventful pregnancy and normal height, weight and head circumference at birth. They didn’t have any history of hyperbilirubinaemia, liver impairment or hypoglycemia in the newborn period. Frontal bossing was noted from birth. They had generalized seizures at one year of age. Cognitive and social milestones were retarded: head control started at age 7 months, sitting at 12 months, standing 18 months, walking at age 2 years and speaking at 3 years. Both patients have hypertelorism with slightly hypotonic appearance with no neurological signs like spasticity, hyperreflexia, ataxia or hypertonia. They have moderate mental impairment, do their personal work without any help, can walk without any gait imbalance, help in washing dishes and cleaning house. They are not able to count money. Cognitive function was tested by Wechsler Adult intelligence Scale (WAIS-IV) and showed IQs of 55 and 40. EEG showed abnormal sharp waves, abdominal ultrasound and echocardiography were unremarkable. Both siblings have megaloblastic anemia with low Hb 12.1g/dL (normal 12.516 g/dL), elevated MCV 106 fL (normal 78-100fL), MCH 31.4 pg (normal 27-31 pg), reduced MCHC 29.7 g/dL (normal 31.0-37.0), and RDW-CV 11.4% (normal 11.5-14%). No diagnostic workup was done until the age of 29 and 23 years, when they participated in an exome sequencing study for intellectual disability and homozygous missense mutations in the ADK gene were identified (c.[971 A>G], p.[His324Arg]) (Najmabadiet al. 2011). Case report family VIII (patient 11) Patient 11, a boy, was born at term as first child with a birth weight of 3270g. His parents are first-degree cousins of Kurdish ethnicity. Two brothers of the father had died of unknown cause at 6 months of age in Turkey. At birth, patient 11 was non-reactive and hypotonic, severe hypoglycemia (0.6 mmol/L) was detected (within the first minutes after birth) and CPAP was needed to ventilate the patient. Since the neonatal age, dysmorphism with frontal bossing, hypertelorism and sparse hair was noted. He had a liver dysfunction with hyperbilirubinaemia (max. total bilirubin 957.3 µmol/L, direct bilirubin 649.6 µmol/L), which ameliorated after three months of life. There was recurrent moderate hyperammonemia (around 100 µmol/L, normal after birth, realized at the age of 2 weeks) of unknown origin. Sodium benzoate was given to control hyperammonemia. On a low protein diet the patient seemed to do worse and did not gain weight. Surprisingly, he stabilized on a rather high protein diet (3 g/kg/d). Blood ammonia normalized after 5 months of age. Methionine concentration was very high initially (max. 436 µmol/L), but decreased in the further course and was intermittently within the normal range. Adenosine in urine rose secondarily (normal in a first urine sample at 2 weeks of age) and the combination with intermittent high methionine guided to the diagnosis of ADK deficiency. Mutation analysis revealed a homozygous missense mutation in the ADK gene (c.905 T>C, p.Phe302Ser). At last visit, the patient was 2.25 years old. He had short stature and relative macrocephaly. He can comprehend simple orders, is able to walk with assistance and speak some words. He has a developmental age of 12 months. II. Supplementary tables and figure Table S1. Anthropometrical data at birth and at last assessment At birth At last assessment Head Height (cm) / circumference (cm) / SDS SDS Patient, family Gestational Weight (g) / age SDS Head Height (cm) / circumference (cm) / SDS SDS 1, I 37+4 2370 / -1.2 48 / -0.4 33 / -0.5 died 15 m n.a. n.a. n.a. n.a. 2, I 3, II 4, III 5, III 6, IV 7, V 8, VI 9, VII 10, VII 11, VIII 36+4 37+5 „term“ „term“ 36 39 39 38 39 40 3840 / 1.4 3990 / 2.1 2300 / n.a. 2900 / n.a. 2990 / 0.3 3030 / -1.1 2890 / -1.1 2800 / -0.9 2950 / -1.0 3270 / -0.8 54 / 1.4 53 / 1.3 n.a. n.a. n.a. 51 / -0.4 51 / -0.1 n.a. n.a. 48 / -2.0 37 /1.6 34 / -0.1 n.a. n.a. n.a. 36.5 / 0.9 33 / -1.2 35 / 0.5 35 / 0.3 36 / 0.3 7.5 y 11.75 y 14.6 y 8.25 y 22 y 5y 9.5 y 33 y 27 y 2.1 y 28.0 /-0.58 29.0 / -2.0 34.2 / -3.3 18.4 / -2.9 40 / -5.1 20.5 / 0.5 26 / -1.2 52 / n.a. 50/ n.a. 9.7 / -2.0 128.0 / -0.05 145 / -1.1 137.8 / -4.9 118 / -2.9 151 / -4.5 102 / -2.6 132.5 / - 0.4 160 / 0.5 155 / 0.5 80 / -3.3 54.5 / 0.8 54 / -0.2 51.8 / -2.4 53.7 / 0.5 61 / 3.9 51 / -1.2 53 / -0.5 58 / 2 57.5 / 2 50.6 / 0.2 0.64 -2.3 -0.8 -1.9 -1.9 2.1 -1.8 -1.0 -1.0 -0.8 Age Weight (kg) / SDS BMI: body mass index; SDS: standard deviation score; y: years; m: months; n.a.: not available Table S2. Biochemical response to low methionine diet in patient 7 Methionine AdoMet in AdoHcy in Methionine AdoMet in AdoHcy in Adenosine Adenosine in plasma plasma plasma in CSF CSF CSF in DBS in urine (nmol/L) (nmol/L) (nmol/L) (nmol/L) (nmol/L) (nmol/L) (µmol/L) (µmol/L) Unrestricted diet 486±403 1000 170 n.a. n.a. n.a. 0.61-1.55 n.a. Low methionine diet 52±14 280 58 5 313 27 0.36-0.52 16.1 Reference range 15-35 55-116 9-45 <5 104-337 5-31 <0.8 0.0-0.1 Maximum values, unless ranges are given. n.a.: not available. All values measured after new-born period. BMI SDS Figure S1. Impact of low methionine diet on liver function and methionine levels A: Patient 3 received a low methionine diet from 7 months to 59 months; at the age of 23 months, dietary treatment was paused for 2 months. After the start of the methionine restricted diet, methionine concentrations and levels of ALAT decreased, whereas during disruption and after termination of the diet, levels increased again. Thus normalization of methionine concentration and ALAT is associated with dietary treatment. Total bilirubin was very high during the first year of life and decreased after the onset of diet; however there was no increase after termination of the diet. B: In patient 7, the low methionine diet was started at the age of 31 months. Methionine concentrations and ALAT, which were repeatedly highly elevated before, have normalized under therapy and total bilirubin concentration stabilized at a level slightly above the upper normal range.