PMD 20. Alimentary pathol.doc
advertisement

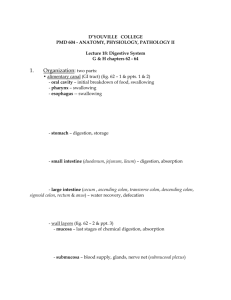
D’YOUVILLE COLLEGE
PMD 604 - ANATOMY, PHYSIOLOGY, PATHOLOGY II
Lecture 20: Disorders of Alimentary Canal
G & H chapter 66 & Robbins chapter 15
1.
General GI Response to Irritations:
• vomiting (emesis): retrograde expulsion (=antiperistalsis) from stomach &/or
small intestine occurs via a reflex involving vomiting center of brainstem
- removes offending materials from upper GI tract, usually with minimal upset
except when a condition becomes chronic
- sensory signals from pharynx, esophagus, stomach & upper small
intestine (especially distension of duodenum), conveyed by vagus n. or spinal
sympathetic nerves represent afferent limb of reflex
- sensation of nausea (consciousness of impending emesis) often precedes
vomiting reflex
- stimuli such as emotional upset, certain drugs or chemicals (excessive
spices or alcohol, bacterial toxins), upset equilibrium signals, gastric stretching due
to overfilling, -- are mediated by higher brain levels, or via 'chemoreceptor trigger
zone' in the brain (fig. 66 - 2 & ppt. 1)
- motor fibers, carried by divergent circuitry from vomiting center (cranial
nerves V, VII, IX, X & XII) trigger various responses:
- closures of duodenum, glottis, and soft palate to ensure expulsion
pathway is out the mouth
- powerful contractions of abdominal wall muscles and antiperistalsis of
gastric muscularis, to expel stomach (and sometimes, intestinal) contents (ppt. 2)
- chronic vomiting may result in loss of fluids, loss of electrolytes, increased
blood pH (as stomach replaces acid deficiency)
PMD 604, lec 20
- p. 2 -
• diarrhea: increased stool mass, stool fluidity & heavy mucus production
cause distension that stimulates increased frequency of defecation reflex
- types of diarrhea include secretion, exudative, malabsorptive & osmotic
diarrheas
- usually results from various infectious (viral, bacterial or protozoon
enterocolitis) conditions in the GI tract (table 15 - 7) that lead to excess fluid in colon
- excessive fluid stems from: (ppt. 3)
- factors that stimulate secretion: irritants such as bacterial toxins,
impaired fat digestion & absorption, poor recycling of bile salts (associated with resected
ileum), tumors & excessive use of laxatives
- factors that impose osmotic retention of water in colon: increased
content of undigested materials in colon, overuse of antacids containing poorly
absorbed ions such as Mg+
- factors that impair water absorption by colon: malabsorption diseases,
irritable bowel syndrome (disturbed motility and accelerated clearance)
- laxatives act to increase colonic volume (& distention) via:
- water-retaining or bulk-producing materials (e.g. methylcellulose)
- increasing osmotic concentration (e.g. magnesium ion)
- irritant effects that stimulate secretion by the large bowel
- emulsifying agents that soften stools
- chronic diarrhea may lead to fluid loss, electrolyte loss & acidosis (due to
bicarbonate loss = metabolic acidosis)
- many cases may be associated with constipation or irritable bowel
syndrome, a poorly understood but frequently encountered condition
PMD 604, lec 20
- p. 3 -
- treat with inhibitors of motility, promoters of fluid absorption
PMD 604, lec 20
2.
- p. 4 -
Disorders of Oral Cavity:
• infections & tumors: Herpes simplex, a virus infection, causing cold sores;
although usually uneventfully resolved, may become latent in nerve ganglia
- Candida infections are fungal (usually occur in immunosuppressed
individuals), produce plaques in oral mucosa & carry high risk of fungal dissemination
- main tumors are squamous cell carcinomas
3.
Disorders of Esophagus:
• achalasia involves incomplete relaxation of lower esophageal sphincter (LES) with
resultant functional obstruction of swallowing & esophageal distension; potential for
development of squamous cell carcinoma
• esophagitis (less frequent than other regional inflammations) most often
stems from impaired constriction of lower esophageal sphincter (LES)
- CNS depressant drugs, chocolate, alcohol & smoking are among agents that
impair LES
-acid reflux from stomach results in inflammation & damage to esophageal
mucosa
- may be associated with sliding hiatal hernia or (less frequently) with
paraesophageal hiatal hernia (fig. 15 - 6 & ppt. 4)
4.
Gastric Disorders:
• gastritis: chronic gastritis often results from bacterial infection (Helicobacter
pylori)
- autoimmune condition that destroys gastric mucosa (conducive to pernicious
anemia) is less frequent cause
- usually produces symptoms of 'indigestion', but serious cases may lead to
ulcers or tumors
- acute gastritis, an acute mucosal inflammation, may be exacerbated by
aspirin, NSAIDs, alcohol abuse or heavy smoking
PMD 604, lec 20
- p. 5 -
• gastric ulceration: large majority of ulcers are peptic ulcers in gastric or
duodenal regions - regions that may be exposed to acid & pepsin; more prevalent in males
than females
- normal mucosal defenses involve mucus production (including bicarbonate
ion content), tight junctions of epithelial cells (prevent H+ diffusion into submucosa) &
disposal of damaged cells via cell renewal system
- impaired defenses coupled with gastric hypersecretion of acid and
pepsin lead to mucosal erosion followed by digestion of submucosal tissues (fig. 15 - 15 &
ppt. 5)
- peptic ulcer is most frequently associated with bacterial infection (Helicobacter
pylori)
- in absence of infection, ulceration is associated with NSAID use; often
exacerbated by alcohol abuse and/or heavy smoking (ppt. 6)
- severe cases may result in bleeding (potential hypovolemic shock) and
perforation (potential for peritonitis)
- bleeding: from severe ulcers, lacerations due to violent vomiting & mucosal
inflammations
- blood in vomitus has coffee ground appearance; blood in stools, a tar-like
appearance (dark brown product of acidified hemoglobin)
- obstruction may result with pyloric ulcers -- due to muscle spasm &
submucosal scarring (fig. 66 - 1 & ppt. 7)
- antibiotic therapy may eliminate the H. pylori infection and facilitate
healing
- antacid &/or antihistamine therapies may combat hyperacidity
PMD 604, lec 20
- p. 6 -
- stress ulcers usually are less severe & result from conditions that may disrupt
mucosal blood supply (ischemia)
PMD 604, lec 20
5.
- p. 7 -
Small and Large intestinal Disorders:
• diverticulosis: pouches of mucosa extruded through muscularis, usually in
sigmoid colon (ppt. 8)
- results from elevated pressure in the colon
- diverticula may lead to entrapped fecaliths, which lead to inflammation
- inflammation represents diverticulitis
- risk of peritonitis from bleeding and/or perforation
- adequate fiber in diet is preventive
• inflammatory bowel disease (IBD): cause not well understood, but genetic
predisposition and immune/autoimmune attack on mucosa may be involved
- most cases are characterized by chronic episodic attacks (cramping,
diarrhea & fever) followed by periods of remission
- inflammations seem to be triggered by microbial flora
- two patterns are recognized:
- Crohn disease mainly afflicts terminal ileum and colon & frequently
involves systemic inflammatory complications; Crohn is associated with fistulas,
abscesses, peritonitis & intestinal strictures; lesions are localized with intervening normal
bowel ('skip lesions')
- ulcerative colitis is confined to colon (fig. 15 - 32, table 15 - 10 & ppt. 9);
like Crohn disease, involves systemic inflammatory complications; lesions are continuous,
commencing from rectum and may involve entire colon
- ulcers associated with Crohn disease or ulcerative colitis arise from disease
process within mucosa, not surface attack as is the case with peptic ulcers
- treatment: antidiarrheals, immunosuppressants & anti-inflammatories are
used, but, with Crohn, total bowel resection is often a necessary treatment
PMD 604, lec 20
- p. 8 -
• bowel obstructions (= ileus): mechanical ileus and adynamic ileus (arrest of
peristalsis) are recognized; adynamic ileus includes strictures (due to spasms, paralysis
or fibrosis)
- mechanical obstructions include loops entrapped in hernias (with resulting
strangulation), adhesions, volvulus and intussusception (figs. 66 - 3, 15 - 26, table 15 - 6 &
ppts. 10 to 12)
- sequelae include obstipation (obstructive constipation), fluid & electrolyte
loss due to vomiting, necrosis & possible perforation (ppt. 13)
• peritonitis: irritants from perforations of abdominal organs, or from wounds,
surgical incisions, or sexually transmitted infections may provoke inflammation of
peritoneum
- detectable by palpation of abdomen (rebound tenderness) due to extreme
sensitivity of peritoneum to pain
- irritants cause local abscesses, scarring, and adhesions that may disrupt bowel
motility, or may cause fistulas (abnormal connections between lumina of unrelated organs,
e.g., colon with other loops of bowel, with vagina, with urinary bladder, etc.)
- generalized peritonitis is associated with widespread damage to
abdominal organs with high risk of septicemia & shock
• appendicitis: obstruction to opening of appendix (frequently by hardened
stool = fecalith) facilitates infection, swelling, & potential perforation (sequel to ischemia,
necrosis & gangrene)
- more prevalent in young people (age 10 - 20 years)
- risk of peritonitis with burst appendix (fig. 15 - 46 & ppts. 14 & 15)
• malabsorption: consequence of impaired digestion, impaired absorption,
&/or impaired transit; sequel of many other disorders (table 15 - 9)
- impaired digestion results from enzyme insufficiencies, bile insufficiency
(due to pancreatic &/or liver disorders) or bowel resections
- impaired absorption may involve immune sensitivity (to certain food
nutrients, e.g. gluten from grains) that destroys villi (= celiac disease) or infections that
destroy villi (= tropical sprue)
- impaired transit involves disturbances to normal lymphatic delivery of
absorbed fats to the circulation (lipoprotein deficit or collapsed lacteal due to
infiltration of villus with macrophages)
PMD 604, lec 20
- p. 9 -
- consequences are widespread affecting many other systems (ppt. 16)
PMD 604, lec 20
- p. 10 -
• cancer: tumors, e.g. carcinomas, adenomas, polyps, may be found (in order of
frequency) in colon (fig. 15 - 35 & ppt. 17), stomach, esophagus, and small intestine
- may cause obstructions, bleeding, pain
- polyp removal is most often achieved during colonoscopy