PMD 18. Digest.syst.A&P - campus
advertisement

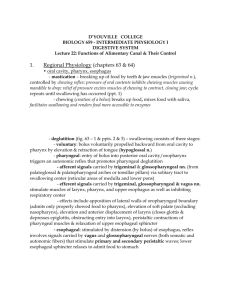
D’YOUVILLE COLLEGE PMD 604 - ANATOMY, PHYSIOLOGY, PATHOLOGY II Lecture 18: Digestive System G & H chapters 62 - 64 1. Organization: two parts: • alimentary canal (GI tract) (fig. 62 – 1 & ppts. 1 & 2) - oral cavity – initial breakdown of food, swallowing - pharynx – swallowing - esophagus -- swallowing - stomach – digestion, storage - small intestine (duodenum, jejunum, ileum) – digestion, absorption - large intestine (cecum , ascending colon, transverse colon, descending colon, sigmoid colon, rectum & anus) – water recovery, defecation - wall layers (fig. 62 – 2 & ppt. 3) - mucosa – last stages of chemical digestion, absorption - submucosa – blood supply, glands, nerve net (submucosal plexus) PMD 604, lec 18 - p. 2 - - muscularis – motility; inner circular & outer longitudinal smooth muscle, nerve net (myenteric plexus) (ppt. 4) PMD 604, lec 18 - p. 3 - - serosa – outer limiting serous membrane, continuous with peritoneum (visceral peritoneum) • accessory glands - major salivary glands (three pairs: sublingual, submandibular, parotid) – secretion of saliva to aid oral digestion (ppt. 5) - liver – metabolic regulation of absorbed nutrients, secretion of bile (ppt. 6) - pancreas – secretion of buffering and enzyme – rich juices (ppt. 7) 2. Blood Supply: • splanchnic circulation (fig. 62 – 6 & ppt. 8): flow pattern is from arteries to gut, pancreas, liver & spleen; portal vein conveys blood from gut, pancreas & spleen to liver; liver drainage is via hepatic veins - arterial supply (fig. 62 – 7, ppts. 9 to 12) – celiac trunk (from aorta) supplies liver, stomach & spleen - superior mesenteric artery (from aorta) supplies the small intestine, pancreas & the right half of large intestine PMD 604, lec 18 - p. 4 - - inferior mesenteric artery (from aorta) supplies left half of large intestine & rectum - increased intestinal activity stimulates vasodilation of arterioles supplying active area; several hormones released by the active GI tract also promote vasodilation - villi are served by arteriole-capillary-venule system + lymphatic capillary (lacteal) (fig. 62 – 8, ppts. 13 & 14) - venous drainage all of abdominal GI tract + pancreas and spleen drain into hepatic portal system, which delivers nutrient-rich blood directly to liver (fig. 62 – 6 & ppt. 8) - liver processing (storage, metabolic conversion, etc.) regulates blood levels of absorbed substances - liver drains via hepatic veins to inferior vena cava 3. Motility and Secretory Activity: • electrical activity of unitary smooth muscle - organized as sheets of cells interconnected by gap junctions allowing electrical disturbances to pass unimpeded throughout muscle mass (functional syncytium) - types of electrical activity (fig. 62 – 3 & ppt. 15): - slow waves – graded potentials, usually not strong enough to elicit contraction; slow waves that exceed threshold cause spike potentials - spike potentials are volleys of action potentials; action potentials are of long duration (10 – 40 times duration of a nerve AP); tonic contractions result from spike potentials & also from hormonal stimulation PMD 604, lec 18 - p. 5 - - depolarization – factors such as stretching, acetylcholine or parasympathetic stimulation or certain GI hormones may raise the resting membrane potential, making the muscle more excitable - hyperpolarization – factors such as epinephrine or norepinephrine or sympathetic stimulation may drive the resting potential down, making the muscle less excitable • enteric nervous system (fig. 62 – 4 & ppt. 16) - nerve plexuses (myenteric and submucosal) extend entire length of GI tract from esophagus to anus - myenteric regulates motility; submucosal regulates glandular secretions - local reflexes or autonomic reflexes modulate enteric nervous system - enteric nervous system secretes excitatory (e.g. acetylcholine) or inhibitory (e.g. norepinephrine) neurotransmitters - parasympathetic innervation – fibers of cranial nerves VII (facial) & IX (glossopharyngeal) supply major salivary glands - most of the remaining alimentary canal is supplied by cranial nerve X (vagus) - sacral nerves (pelvic nn.) from S2 – S4 supply lower large intestine, rectum & anus (fig. 60 - 3 & ppt. 17) - parasympathetic signals excite the enteric nervous system, leading to enhanced motility & secretions PMD 604, lec 18 - p. 6 - - sympathetic innervation – fibers of spinal nerves from T5 to L2 supply most of the alimentary canal via prevertebral ganglia (e.g. celiac) (fig. 60 - 1 & ppt. 18) - sympathetic signals inhibit the enteric nervous system & inhibit smooth muscle directly • hormonal reflexes (table 62 - 1 & ppt. 19) - gastrin is produced by G cells of stomach mucosa & triggers gastric acid secretion & cell renewal - cholecystokinin is produced by I cells of duodenum and jejunum mucosa; it excites gall bladder contraction, pancreatic secretion of enzymes and inhibits stomach emptying PMD 604, lec 18 - p. 7 - - secretin is produced by S cells of duodenum mucosa; it triggers release of bicarbonate-rich juice by the pancreas & inhibits gastric secretion • patterns of contraction - propulsive – peristalsis (fig. 62 – 5 & ppt. 20) involves formation of ringlike constriction that advances slowly along the gut toward the anus, pushing contents along (mediated by myenteric plexus) - mixing – intermittent constrictions (segmentation contractions) produce chopping or shearing of contents (assist peristaltic mixing) (ppt. 21) 4. Regional Physiology (chapters 63 & 64) • oral cavity, pharynx, esophagus - mastication – breaking up of food by teeth & jaw muscles (trigeminal n.), controlled by chewing reflex - creation of a bolus: broken up food, mixed with saliva, facilitates swallowing and renders food more accessible to enzymes - deglutition (fig. 63 – 1 & ppt. 22) – swallowing consists of three stages: - voluntary: bolus voluntarily propelled backward from oral cavity to pharynx by elevation & retraction of tongue (hypoglossal n.) - pharyngeal: entry of bolus into posterior oral cavity/oropharynx triggers an autonomic reflex that promotes pharyngeal deglutition (trigeminal, glossopharyngeal, vagus & hypoglossal nn.) - effects include narrowing of oropharyngeal boundary (admits only properly chewed food to pharynx), elevation of soft palate (occludes nasopharynx), elevation and anterior displacement of larynx (closes glottis & depresses epiglottis, obstructing entry into larynx), peristaltic contractions of pharyngeal muscles & relaxation of upper esophageal sphincter PMD 604, lec 18 - p. 8 - - esophageal: stimulated by distension of esophagus, reflex involves signals carried by vagus and glossopharyngeal nerves that stimulate primary and secondary peristaltic waves; lower esophageal sphincter relaxes to admit food to stomach PMD 604, lec 18 - p. 9 - - secretions: (fig. 64 - 1 & ppt. 23) - triggered by: 1) contact with mucosa; 2) chemical irritation of mucosa; 3) distension of alimentary canal - local reflexes (enteric nervous system), autonomic reflexes (mostly parasympathetic) and some hormonal reflexes are involved - salivary gland secretions range from watery (serous) to thick and sticky (mucous) - saliva also contains numerous ions (bicarbonate, potassium, sodium, chloride) & enzymes (salivary amylase or ptyalin - commences chemical digestion & lysozyme - combats bacteria in oral cavity) - cranial nerves VII and IX (facial & glossopharyngeal) carry sensory limb of reflex via solitary tract to salivatory nuclei, which send parasympathetic fibers (motor fibers in nerves VII & IX) to major salivary glands (fig. 64 – 3 & ppt. 24) • stomach (fig. 63 – 2 & ppt. 25): - a relaxation reflex in response to initial distension facilitates storage - mixing is accomplished by weak peristaltic (constrictor) waves accompanied by tonic contraction of pyloric sphincter (may cause retropulsion) - emptying – more intense peristaltic waves ‘pump’ chyme into duodenum - controlled by gastrin (+), enterogastric reflex (-) & cholecystokinin (-) - secretions – tubular glands (fig. 64 – 4 & ppt. 26) of the stomach mucosa include mucous neck cells (mucus), parietal cells (HCl & intrinsic factor), chief cells (pepsinogen) & G cells (gastrin) - most of the surface mucosal cells secrete mucus PMD 604, lec 18 - p. 10 - - acid secretion (fig. 64 – 5) appears to be stimulated by gastrin and by postganglionic parasympathetic neurons (secrete acetylcholine) PMD 604, lec 18 - p. 11 - - pepsinogen secretion - stimulated by acid & by parasympathetic fibers - mucus secretion (alkaline) is stimulated by contact of mucosa with food or irritation of the mucosa - phases of gastric secretion (fig. 64 – 7 & ppt. 27) – cephalic: sight, smell, taste or even thought of food initiates parasympathetic signals via vagus nerve to stimulate gastric secretion - gastric: entry of food into stomach stimulates a vagovagal reflex and gastrin secretion, which stimulates gastric juice secretion - intestinal: enterogastric signals (via enteric nervous system), secretin & other GI hormones (e.g. gastric inhibitory peptide) all inhibit secretion of gastric juice