The Urinary System Organs: Kidneys (creates urine), ureters (transport), urinary bladder
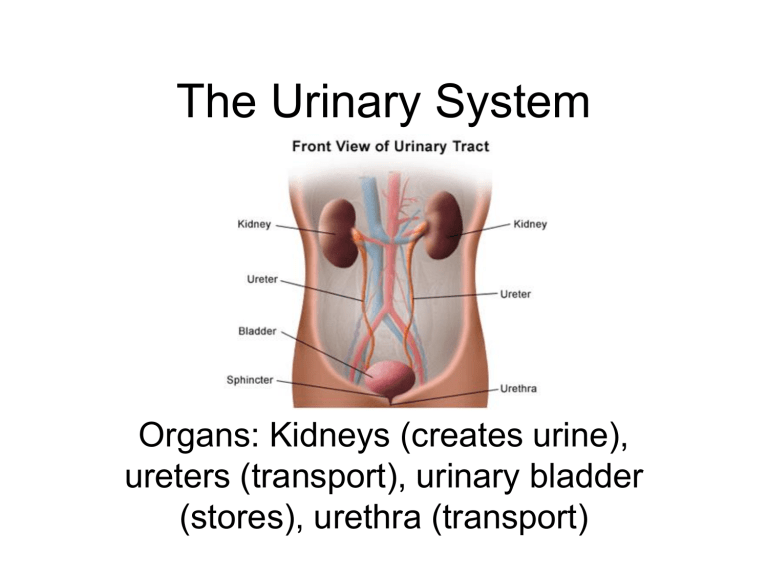
The Urinary System
Organs: Kidneys (creates urine), ureters (transport), urinary bladder
(stores), urethra (transport)
Kidney Function
• Filter fluids from bloodstream and maintain homeostasis in body
• Rids body of wastes, excess ions, toxins, and drugs in urine
• Regulate blood volume, pH, salt content
• Secretes renin – regulates blood pressure
• Secretes erythropoietin – increases rbc production
Kidney Anatomy
• 5” long, 2.5” wide
• Renal capsule:
– encloses kidney
• Renal cortex:
– outer region
• Renal medulla:
– deep to cortex w/ medullary pyramids separated by renal columns
• Renal hilus:
– medial indentation
• Rich Blood Supply
– Renal artery segmental arteries
lobar arteries interlobar artery
afferent arteriole glomerulus capillaries efferent arteriole peritubular capillaries interlobular vein arcuate vein interlobar vein renal vein
Nephrons
• Nephrons form urine
• Glomerulus: knot of capillaries
• Renal tubule w/ enlarged bowman’s capsule at end
• Proximal convoluted tubule
• Loop of Henle
• Distal convoluted tubule
• Collecting ducts: receive urine from many nephrons; deliver urine to renal pelvis
Urine Formation
• Filtration
– Water and solutes smaller than proteins are forced thru capillary walls and pores of glomerular capsule into the renal tubule
• Tubular reabsorption
– Water, glucose, amino acids, and needed ions are transported out of the filtrate into the tubule cells and then enter the capillary blood
• Tubular Secretion
– Urea, H + , K + , creatinine, and drugs are removed from the peritubular blood and secreted by the tubule cells into the filtrate
• Urine: 1-2 L produced every 24 hrs
Ureters
• 10-12” long tubes
• Carry urine from kidneys to bladder
• Peristalsis propels urine transport
• Valve-like folds prevent back flow from bladder
Urinary Bladder
• Smooth, collapsible muscular sac
• Temporarily stores urine
• Empty: 2-3” long
• Full: 5”long and stores 1-2 pints urine
Urethra
•
Thin walled tube
•
Carries urine (by peristalsis) from bladder to outside the body
•
Females: 3-
4” long, opening is anterior to vaginal opening
• Males: 8” long, opening at tip of penis
– Double function: passageway for sperm ejaculation
• internal urethral sphincter:
– Involuntary smooth muscle, keeps closed when urine is not being passed
•
External urethral sphincter:
– Voluntary skeletal muscle through pelvic floor
•
Micturition
– emptying the bladder
– 200mL urine collects and activates stretch receptors and cause bladder to contract to force open internal urtheral sphincter…feel urge to void
Fluid and Electrolyte Balance
• 2/3 water in intracellular fluid (ICF)
• 1/3 water in extracellular fluid (ECF)
• Electrolytes: charged ions that conduct electrical current, alters blood volume and blood pressure
– Ex. sodium, potassium, calcium ions
• Electrolyte balance maintained by hormones
– Antidiuretic hormone (ADH)
– Aldosterone
Acid-Base Balance
• Proper function, blood pH between 7.35-7.45
– Alkalosis rise in blood pH above 7.45
– Acidosis drop in pH below 7.35
• Blood Buffers
• Respiratory System
• Renal Mechanisms
– Excreting bicarbonate ions
– Reabsorbing or generating new bicarbonate ions