Memorial ICU UCI/LBM Joint Conference
advertisement
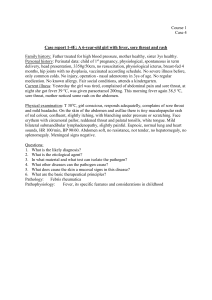
Memorial ICU UCI/LBM Joint Conference 2 Chief Complaint • “Sore throat, fever” 3 HPI • • • • 62 yo M Sore throat, fever x 3 days One day of vomiting, diarrhea Preceded by a week and a half of clear rhinorrhea prior to onset of fever • Presented to LBMC for worsening of symptoms • Onset of symptoms was while traveling in Salt Lake City, Utah for a business trip with his wife. They are in retail. 4 HPI (Con’t) • While in Salt Lake City, he states that there were local fires and proposed that this may have contributed to his symptoms. • The patient also endorses odynophagia, chills, nausea, and shortness of breath when lying flat • Denies sick contacts, chest pain, abdominal pain, weight changes, cough, vision changes, ear pain, urinary symptoms. 5 Review of Systems • CONSTITUTIONAL: No weight loss, endorsed fever, chills, and fatigue • HEENT: No vision changes • SKIN: No rash or itching • CV: No CP or palpitations • RESP: No cough or sputum, endorsed shortness of breath with lying down • GI: endorsed N/V/D • GU: No dysuria, frequency or urgency • NEURO: No HA, dizziness, syncope 6 PMHx/PSHx • GERD - PRN H2 blocker only • Knee arthroscopy – remote • Takes no other medications 7 Social History • Lives in Mount Shasta and visiting family in SoCal • Married • Sexual activity: Monogamous • Pets: Dogs • Worked: Self employed, retail • Tobacco: None • Alcohol: Occasional (2 beers a month) • Illicit: Denies IVDU and all other illicit drugs 8 Physical Examination 1 of 2 • Vitals: T 38.1 , BP 71/43, P 111, RR 34, O2 98% on RA • Gen: Mild discomfort, A&Ox 4 • HEENT: NCAT, anicteric, PERRLA, EOMI, moist oral mucosa . Dentition unremarkable. Mild tonsillar erythema with white exudates on left tonsil. No bulging of posterior pharynx • Neck: Supple, trachea midline. Nontender to palpation. No LAD. 9 Physical Examination 2 of 2 • CV: Tachycardic but regular, no M/R/G. PMI non displaced, no JVD or peripheral edema • Chest: Tachypneic, CTAB, no W/R/R • Abd: Soft, non distended, non tender,, normal BS, no hepatosplenomegaly or palpable masses • Neuro: Awake, alert, oriented x3, speech intact, no focal deficits, patient moving all extremities, CN 2-12 intact bilaterally • Ext: No cyanosis, clubbing or edema • Skin: No rashes, pallor, splinter hemorrhages, Janeway lesions or Osler nodes 10 Initial Labs 1 of 2 • Sodium 136, potassium 4.0, chloride 103, bicarb 18, BUN 40, creatinine 2.10, glucose 182, calcium 8.8, Anion Gap 15 • total protein 7.4, albumin 4.0, alk phos 48, total bilirubin 1.3, AST 24, and ALT 15 • White blood cell count 17.4 (33% Neutrophils, 6% Lymphocytes, 45% Monocytes, 4% Eosinophils, 11% Bands), hemoglobin 13.3, and platelets 131 11 Initial Labs 2 of 2 • • • • • • Lactic acid 5.57.4 CRP 25.8 Cortisol >75 TSH 0.485 ABG: 7.37/26/69/15/-10.0/20% UA: pH 5.0, SG 1.027, Positive for Bilirubin, Glucose 150, WBC 8, Protein 100 • CXR: No acute pulmonary disease • Blood, urine, throat, cultures pending 12 ER Course •Patient was aggressively fluid resuscitated. In the ED, he received 6.5L of NS boluses. •Despite fluids, his SBP remained in the 70s-80s and he was started on Levophed. •He was also empirically started on doxycycline, flagyl, and vancomycin. 13 Initial Assessment • • • • • • Septic Shock Monocytosis – differential on next slide AKI Anion Gap Metabolic Acidosis 2/2 lactic acidosis Thrombocytopenia Pharyngitis 14 Monocytosis DDx • Infectious: ▫ ▫ ▫ ▫ ▫ ▫ ▫ EBV CMV Subacute Bacterial Endocarditis Erlichiosis/anaplasmosis Rocky Mountain Spotted Fever Brucellosis Syphilis • Autoimmune: SLE, IBD, etc • Myeloproliferative: Hodkin’s and certain leukemias 15 Initial management • Early Goal Directed therapy • Empiric Antibiotics with Unasyn, Vancomycin, Doxycycline – concern for tonsillar pathology • Blood, urine, sputum cultures • Throat cultures • Rickettsia, EBV, CMV serologies • RPR, HIV, ANA, procalcitonin • CT neck with IV contrast to r/o peritonsillar abscess once stable • Peripheral blood smear 16 Next day labs • • • • Blood, urine, throat, sputum Cx: Prelim negative Respiratory viral panel PCR: Neg EBV: marked elevation of IgG. IgM normal. Smear review shows increased promonocytes (19%) and rare myeloblasts. This is a finding highly suspicious for acute leukemia 17 Hospital Course • Continued to endorse SOB and was tachypneic with respiratory rates in 50s • CXR unchanged • Patient intubated • Increasing pressor requirement with addition of vasopressin and dobutamine • ABG 7.12/28/88/9 on FiO2 35%, given 2 amps bicarb and started on bicarb drip • Worsening creatinine to >3 with decreasing urine output 18 Hospital Course • Infectious Disease consulted ▫ Meropenam, vancomycin, doxycycline and acyclovir (concern for possible EBV reactivation) • Heme/Onc consulted ▫ ▫ ▫ Reviewed smear with pathology, very likely AML Bone marrow biopsy showed 24% myeloblasts, 18% monoblasts and promonocytes – supportive of AML, suggestive of myelomonocytic leukemia Cytogenetic studies pending 19 Final Diagnosis • Septic shock with unknown source - likely pharyngeal/tonsillar given symptoms and tonsillar exudate ▫ Less likely a zebra as monocytosis reflects leukemia immunodeficient state ▫ Considering strep pharyngitis with development of Lemierre’s syndrome in the setting of AML • CT scan for further evaluation pending…