Systemic Lupus Erythematosus Sheetal Desai, MD, MSEd Division of Rheumatology
advertisement

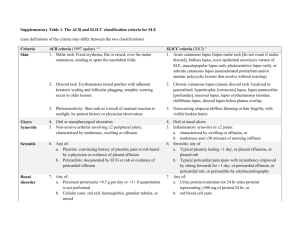
Systemic Lupus Erythematosus Sheetal Desai, MD, MSEd Division of Rheumatology UC Irvine Medical Center Questions??? 1. What is compound E? 2. Who is Phillip Hench? 3. What are the 11 criteria for lupus? 4. What are the two most common drugs associated with drug induced lupus? 5. What is the risk of neonatal lupus in a patient with positive SSA or SSB? Questions??? 6. What is the most common organ system involved in lupus? 7. How many FDA approved medicines are there for lupus and what are they? 8. What is the 10 year life expectancy for lupus? Case #1 23 year old female comes to rheumatology c/o joint pains in her PIPs and wrists, fatigue and a rash on her face. This has been going on for several months. She denies any fevers, ulcers, CP, SOB, Raynaud’s. She does have photosensitivity. PMH: acne, endometriosis PSH: none Meds: OCP, minocycline PE: VSS, malar rash, TTP to PIPs, no synovitis Labs: WBC 5, Hg 11, Plt 200, BUN 8, Cr 0.6, ANA pos 1:160, TSH 4.3 What do you do? History of Lupus Lupus means “wolf” in Latin 10th century- case reports appeared in writings Late 1800s- Sir William Osler initially described the systemic nature and linked rashes to organ involvement 1949- LE cell described by Malcolm Hargraves at Mayo Clinic 1954- ANA described 1971- First set of classification criteria proposed for Lupus 1983- Antiphospholipid antibody syndrome described What exactly is Lupus? Autoimmune disease where one’s immune system attacks itself Autoantibody production -> immune complex deposition -> inflammation -> damage Chronic disease, characterized by flares and remission Pleomorphic with different phenotypic expressions Multisystem involvement Types Of Lupus Drug Induced Lupus Neonatal Lupus Cutaneous Lupus Systemic Lupus Erythematosus Drug- Induced Lupus Approximately 80 offending agents can cause lupus 15,000- 30,000 cases reported annually Production of autoantibodies more common than clinical symptoms 99% disappear within 3 months of stopping the medicine. DIL Definite Associations Procainamide (15-20%) Hydralazine (7-13%) Enbrel/Remacaide/Humira (2/1000) Minocycline (5/10,000) Diltiazem Penicillamine INH Quinidine Clinical DIL Classic SLE Age of onset 50 20-40 F:M ratio 1:1 9:1 arthralgia 95% 90% hepatomegaly 25% 25% Rash 74% 10-20% Renal disease 5% 53% CNS disease 0% 32% ANA 95% 95% Anti-histone 90% 80% Case #1 23 year old female comes to rheumatology c/o joint pains in her PIPs and wrists, fatigue and a rash on her face. This has been going on for several months. She denies any fevers, ulcers, CP, SOB, Raynaud’s. She does have photosensitivity. PMH: acne, endometriosis PSH: none Meds: OCP, minocycline PE: VSS, malar rash, TTP to PIPs, no synovitis Labs: WBC 5, Hg 11, Plt 200, BUN 8, Cr 0.6, ANA pos 1:160, TSH 4.3 What do you do? Case #2 32 year old female with known Lupus for five years, on plaquenil 400mg a day and prednisone 3mg a day, wants to get pregnant. How do you advise her? Fertility? Risk of neonatal lupus? Medications during pregnancy? Neonatal Lupus Rare condition not true lupus, passively transferred autoimmune disease Occurs when mother is SSA/SSB positive Transplacental transfer of IgG anti SSA or SSB antibodies 5-7% babies will have a transient rash, resolves by 6-8 months 2% of babies will have cardiac complications with congenital heart block Neonatal Lupus See erythematous, annular plaques tends to involve scalp, face, periorbital areas Who get’s Lupus? Prevalence is over 1.5 million Americans Incidence difficult due to lack of strict definition Bimodal peak presentation: ages 20-40 and again after age 60 Prevalence is higher in African Americans, Asians, Hispanics Female to male predominance Does your sex really matter? 90% of patients with lupus are female Before puberty F:M ratio is 2:1 During reproductive years ratio 8:1 Post-menopausal ratio 2.3:1 Increased frequency in women attributed to the hormonal effect of estrogen Does your sex really matter? Nurses Health Study use of estrogen-containing contraceptive agents associated with an 50 percent increase in risk of developing SLE either early onset of menarche (age ≤ 10 years) or administration of estrogen to postmenopausal women doubles their risk Treatment of clinically stable SLE with oral contraceptives for one year does not increase disease flares What causes Lupus??? Damage Genetically susceptible individual Environmental factors Inflammation Auto antibody production Genetics of Lupus High concordance in monozygotic twins 5-12% or relatives with lupus have the disease No single lupus gene Disease is polygenic At least 30 susceptiblility genes identified HLADR2, HLADR3, HLADR4, HLADR8 (present in 75%) Homozygous deficiency of C1q complement Environmental Factors UVA and UVB light can stimulate/ up-regulate autoimmunity stimulating keratinocytes to produce cytokines -> activate B cells to produce ab Viruses/Bacteria: molecular mimicry SLE patients have higher titers of antibodies to Epstein-Barr virus (EBV), increased circulating EBV viral loads; SSA ab has a sequence similar to EBV nuclear ag 1 Parvovirus B19 Drugs Silica exposure, tobacco smoke, emotional stress Lupus Damage Genetically susceptible individual Environmental factors Inflammation Auto antibody production Immune dysregulation Upregulation of innate immunity Delayed clearance of apoptotic cells, resulting in antigenic stimulation Loss of tolerance via failed elimination of autoreactive T lymphocytes Abnormalities in B cells Abnormalities in T regulatory cells (CD4+/CD25+ cells down regulate immune system responses) Autoantibodies in Lupus Study of US army recruits revealed lupus autoab present for up to 9 years prior to dx in 85% ANA dsDNA Anti-Smith Anti-RNP Anti-SSA, anti-SSB Anticardiolipin Anti B2 glycoprotein Meaning of ANAs What exactly are they? Antibodies that bind to various antigens in the nucleus of a cell How is it measured? Indirect Immunofluorescence ANA measurement Indirect Immunofluorescence Assay 1. Take patient serum and add it cells 2. If there are antibodies they will bind 3. Add a fluorochrome tag 4. View under a fluorescent microscope 5. If it lights up in the nucleus then it is positive 6. Dilute sample and repeat steps 1-5 until nuclear fluorescence disappears ANA patterns ANA patterns Staining Patterns Observer dependent Not sensitive Not specific Only LOOSELY associated with certain disease states ANA associated Diseases Rheumatic Conditions Rheumatic Conditions AutoImmune Misc Lupus Polymyositis Grave’s Aging Drug-induced Lupus Dermatomyositis Primary Biliary Primary Cirrhosis Pulmonary HTN Scleroderma RA Hashimoto Thyroiditis Sjogren’s Vasculitis Autoimmune Hepatitis MCTD MS ANA and Aging For every year after age 50, percentage of ANA positivity increases 1%/year For example Age 50 1% Age 55 5% Age 60 10% ANA in Lupus Sensitivity 93-99% in SLE Sensitivity 95-100% in drug induced Lupus Specificity is not great Higher the titer, higher the specificity 1:40- 30% normal population 1:160- seen in 5% of the population Clinical Indications for ANA ANA is NOT a good screening test given its low specificity Presence of ANA does NOT mandate the presence of rheumatologic illness A negative ANA is more useful and makes Lupus very unlikely ANA titers correlate poorly with disease activity so serial measurements are not recommended A positive ANA with anti-centromere pattern is very specific for limited scleroderma How do patients present? Myriad of symptoms Symptoms are often non-specific No two patients are alike 50% of patients have organ threatening disease 50% do not have organ threatening disease Question What is the most common organ system involvement in lupus? How do patients present? 90% malaise and fatigue 90% arthralgia and myalgias 70% photosensitivity/rashes 57% fever 50% arthritis 44% pleuritis 40% alopecia 25% raynaud’s 25% hypertension 20% oral ulcerations Malar rash Malar rash Discoid Lesions Oral ulcerations Raynaud’s Jaccoud’s arthropathy Laboratory Findings in SLE 97% positive ANA 61% low complement levels (C3, C4) 50% dsDNA ab 46% leukopenia 42% anemia 40% proteinuria, nephritis 35% anticardiolipin antibodies 25% sjogren’s syndrome with positive SSA, SSB 12% pleural effusion Others: thrombocytopenia, anti SM, antiRNP, elevated LFTs, splenomegaly, thrombophilia, miscarriages Diagnosis of SLE Initial criteria proposed by the ACR in 1971, revised in 1982 and 1997 Criteria designed for research purposes Need 4 of 11 criteria for diagnosis of SLE Not perfect, but have over 90% sensitivity and specificity Currently two international groups are reevaluating the criteria ACR 1997 revised criteria 1. malar rash 2. discoid rash 3. photosensitivity 4. oral or nasal ulcers 5. arthritis 6. serositis: pleuritis or pericarditis 7. renal disorder: proteinuria > 500mg/day, cells 8. immunologic: anti SM, anti dsDNA, ACL, lupus ac 9. hematologic: anemia, leukopenia, thrombocytopenia 10. neurologic: seizures or psychosis 11. positive ANA in absence of drugs 2012 SLICC Classification Criteria Need at least 4 criteria (1 clinical and 1 lab) Or biopsy proven Lupus Nephritis with Pos ANA or pos dsDNA Case #3 A newly diagnosed patient with lupus asks you what her lifetime prognosis is. What do you say? Prognosis Dramatically improved over time Normal life expectancy for patients with drug induced lupus cutaneous lupus lupus without organ involvement Possible increased risk of NHL Prognosis Year 5 yr survival 10 yr survival Prior 1948 50% 1949 Steroids widely accessible 1969 Dialysis widely accessible 1971 77% 60% 1980-present Increase use of immunosupp 2000-2007 95% 90% Poor Prognostic Factors Renal disease (esp DPGN) Hypertension Male sex Young age Older age at presentation Poor socioeconomic status Black race, which may primarily reflect low socioeconomic status Presence of antiphospholipid antibodies Antiphospholipid syndrome High overall disease activity Mortality Bimodal mortality Early deaths: infection and renal involvement Later deaths: atherosclerotic disease Premenopausal women with lupus have 30-50x higher risk of CAD than their nonlupus counterparts Treatment Individualized Evaluate their risks for organ involvement dsDNA ab: renal and neurologic SSA/SSB ab: rashes, pregnancy risks APL ab: clotting RNP ab: may develop overlap diseases Treatment: Patient Education 1. Avoidance sun 2. Use of SPF > 35 sunblocks UVA and UVB 3. Sun-protective clothing 4. Promote exercise 5. Healthy diet (low chol, low sugar, low salt) 6. Smoking cessation 7. Avoidance of stress (animal models) 8. Good sleep hygiene Treatment: Antimalarials hydroxychloroquine, quinacrine (available compounded), chloroquine Prevent activation of toll like receptors 7 & 9 Used in lupus over 50 years FDA approved indication Mildest immunosuppressant Very safe, risk of retinal toxicity low Eye exam once yearly Hydroxychlorquine Takes 6 weeks to kick in, up to 6 months for maximal effect Dose maximum is *** mg/kg/day Reduces intensity of flares Increases time to flare Treats skin and joint manifestations May prevent renal disease Mortality benefit Treatment: Steroids Mainstay for organ threatening disease Work quickly and effectively dose of 1mg/kg/day taper over 4-6 weeks, by 10% q week Long term AE: hyperglycemia, hyperlipidemia, accelerated atherosclerosis, bone demineralization, AVN, cataracts, glaucoma, PUD, skin thinning, emotional lability Add a steroid sparing imunosuppresant Immunosuppressive regimens Methotrexate: used for arthritis and skin Leflunomide: used for arthritis and skin Azathioprine: useful for renal disease, autoimmune hepatitis, pulmonary disease, myositis, cutaneous manifestations Mycophenylate Mofetil: lupus nephritis Cyclosporine: membranous nephritis, aplasias Cyclophosphamide: used for severe diseasenepritis, CNS involvement, vasculitis Rituximab: used for severe organ threatening dz On the horizon… 1. Agents that target B cells 2. Agents that target T/B/APC interaction 3. Agents that target complement activation 4. Inducers of immune tolerance 5. Agents that target cytokines 6. Inhibition of Toll receptors 7. Stem cell therapies On the horizon… Only four FDA approved medications for lupusprednisone, plaquenil, aspirin, belimumuab Many clinical trials ongoing looking at innovative biologic therapies Highly likely that the management of lupus will be totally altered in the next 5-10 years Outcome, quality of life and prognosis will also dramatically change