Rheumatoid Arthritis: Clinical Overview Roger Kornu, MD Associate Clinical Professor
advertisement

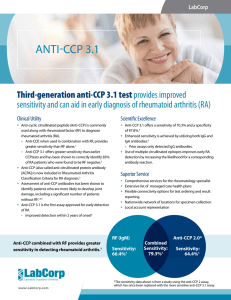
Rheumatoid Arthritis: Clinical Overview Roger Kornu, MD Associate Clinical Professor Division of Rheumatology University of California, Irvine Take Home • RA is a prevalent, inflammatory disease with potential of high morbidity both in articular and extra-articular manifestations. • Symmetrical, small joint pain and morning stiffness with joint swelling on physical exam are the most important clinical features. • Rheumatoid factor, anti-CCP antibody, and inflammatory markers are useful in diagnosis. • Modern clinical criteria allows for earlier diagnosis and more aggressive therapy to minimize joint damage. • Methotrexate is the standard disease modifying agent, but there is a low threshold to add combination therapy as we are in the era of treat to target. Case Presentation • 52 year old Caucasian female presents with 6 months of swelling and stiffness in her bilateral hands, wrists, and feet. She has one hour of morning stiffness. • She is still able to work full-time as a supervisor, but has difficulty in grasping objects and opening doors. Case Presentation • She has no significant medical history and is taking OTC ibuprofen. • Her mother may have had rheumatoid arthritis, but she is not sure. • Physical exam shows joint swelling and tenderness in her bilateral 2nd-5th PIP and 2nd-3rd MCP joints with right wrist swelling. She has tenderness in bilateral MTP joints. Case Presentation • On work-up, she has a normal CBC, electrolytes, and LFTs • ESR 46, CRP 1.5, RF negative, anti-CCP antibody 120 and ANA negative Case Presentation What’s the diagnosis? Rheumatoid arthritis “One must from time to time attempt things that are beyond one’s capacity.” —Pierre-Auguste Renoir Epidemiology • • • • • Prevalence up to 1% Annual incidence 40 per 100,000 Peak age of onset between 50-75 years Female:Male ratio, 2-3:1 Prevalence of RA in females over 65 years is up to 5% • Monozygotic twins 13.5% vs dizygotic twins 3.5% Genetics • HLA-DRB1: “shared epitope” – Individuals with certain sequence found in DR4, DR14 and DR1 beta-chains have higher RA and anti-CCP positivity • Risk of RA and Smoking – Men 2x higher and Women 1.3x higher – Also related to the shared epitope – No relationship of heavy or light smoking McInnes and Schett, NEJM 2011 McInnes and Schett, NEJM 2011 Clinical Presentation of RA Severe RA Early RA Intermediate RA Latinis KM, et al. The Washington ManualTM Rheumatology Subspecialty Consult. Philadelphia, Pa: Lippincott Williams & Wilkins; 2004. Establishing a Diagnosis for RA • Joint stiffness upon awakening • Swelling in specific fingers or wrist joints, with or without pain • Swelling in soft tissues around the joints • Symmetrical pattern of affected joints • Fatigue, depression, occasional fevers, anemia, general sense of malaise • Symptoms may last for years and get progressively worse for the majority of patients Diagnosis of RA: 2010 ACR Criteria Diagnostic Tools in Rheumatoid Arthritis • Rheumatoid factor • Anti-CCP antibodies • Plain X-ray • MRI • Ultrasound Rheumatoid Factor • Antibody directed against the Fc portion of IgG • Present in approximately 80% of RA patients – Sensitivity for RA is ~80% – Specificity is 85-95% • May be involved in disease pathogenesis • Higher levels tend to be associated with poorer prognosis • Found in other conditions, especially Hepatitis C Anti-Cyclic Citrullinated Peptide (CCP) Antibodies in RA • Anti-citrulline Abs produced in RA synovium • Early RA Diagnosis – sensitivity 48%; specificity 96% – seen in 2% of pts with other autoimmune diseases and infections (vs. 14% for RF) – less than 1% of healthy controls • Predicts erosive disease PPV - 63% and NPV 90% • Present years before the onset of symptoms. 34% of blood samples obtained 2.5 yr before onset of symptoms (vs. 1.8% of controls) Plain X-ray Magnetic Resonance Imaging as a Diagnostic Tool Erosions Detected: X-rays vs MRI (%) 50 45 40 30 20 14 10 0 McQueen FM et al. Ann Rheum Dis. 1999;58:156-163. McQueen FM et al. Ann Rheum Dis. 1998;57:350-356. X-ray MRI Ultrasound as a Diagnostic Tool Keen et al. Rheum Dis Clinic N Am 31 (2005) 699-714 Relationship of Radiographic Joint Damage to Disability Severity (Arbitrary Units) Inflammation Disability Radiograph Scores 0 5 10 15 20 Duration of Disease (Years) Adapted from Kirwan JR. J Rheumatol. 1999;26:720-725. 25 30 Features Related to Poor Outcomes Extra-articular disease High rheumatoid factor titer, positive anti-CCP antibody Poor functional status Involvement of multiple joints Radiographic erosions Sustained elevation of acute-phase reactants (eg, ESR) Low socioeconomic status/educational level Increased genetic risk of developing RA plus smoking Anaya JM, et al. Ann Rheum Dis. 1994;53:782-783. Pincus T, et al. Balliere’s Clin Rheumatol. 1992;6:161-191. Furst DE. Rheum Dis Clin North Am. 1994;20:309-319. Padyukov L, et al. Arthritis Rheum. 2004;50:3085-3092. Rheumatoid arthritis: episcleritis Copyright © 1972-2004 American College of Rheumatology Slide Collection. All rights reserved. Rheumatoid arthritis: scleromalacia perforans Copyright © 1972-2004 American College of Rheumatology Slide Collection. All rights reserved. RA: Pulmonary Manifestations • Interstitial lung disease may appear in 25% of RA patients – Nonspecific interstitial pneumonitis (NSIP) • Homogeneous mononuclear infiltrate • Ground glass infiltrate on HRCT • Better prognosis – Usual interstitial pneumonitis (UIP) • Non productive cough and dyspnea • Honeycombing of HRCT • Worse prognosis RA: Pleural Disease • • • • • Males > females In <5% of patients Long-standing disease Low pleural fluid glucose Must exclude infections, malignancy RA: Felty’s Syndrome • Seropositive rheumatoid arthritis – Long standing RA, can have bland synovitis • Splenomegaly • Leukopenia – WBC < 4000 – Neutropenia <1500 • Recurrent infections Large Granular Lymphocyte (LGL) Syndrome • Neutropenia, splenomegaly, and recurrent infections • Clinical features may mimic Felty’s syndrome (“pseudo” Felty’s) • Neutropenia with normal or increased total WBC due to lymphocytosis • May have associated anemia, thrombocytopenia • Clonal populations of LGL in some patients may represent neoplastic proliferation and some patients ultimately develop leukemia or lymphoma RA and Lymphoma • Majority Non-Hodgkin’s Lymphoma (NHL) – Diffuse Large B cell type – MALT (mucosal associated lymphoid tissue) • EBV association in 12% • Higher incidence with age • In early biologic trials with TNF alpha inhibitors, increased incidence of NHL Adult Still’s Disease • Triad – Quotidian fever – evanescent salmon rash – inflammatory arthritis • High acute phase reactants – High ferritin (>4000) – Elevated CRP • Lymphadenopathy, heptomegaly Treatment • NSAIDs, glucocorticoids • Biologics – TNF alpha inhibition – T-cell inhibition – B cell inhibition – IL-6 inhibition • Small molecules – JAK kinase inhibition Maximum Percentage of Joints Affected Joint Erosions Occur Early in Rheumatoid Arthritis 30 Metatarsophalangeal joint 20 Total Hand 10 0 0 1 2 3 Year van der Heijde DM, et al. J Rheumatol. 1995;22:1792-1796. Fuchs HA, et al. J Rheumatol. 1989;16:585-591. McQueen FM, et al. Ann Rheum Dis. 1998;57:350-356. Treatment: The Earlier, the Better Delayed treatment 1993-1995* (median lag time to treatment=123 days; n=109) Change in Median Sharp Score 14 Early treatment 1996-1998* 12 (median lag time to treatment=15 days; n=97) 10 8 6 4 2 0 0 6 12 18 Time (Months) *Patients were treated with chloroquine or sulfasalazine Lard LR, et al. Am J Med. 2001;111:446-451. 24 Goals of Therapy • Treat early • Treat to limit and/or prevent – Pain – Joint damage – Extra-articular disease – Disability – Premature death • Treat to target Traditional DMARD Selection Agent Time to Benefit Potential Toxicity Methotrexate 1–2 mo Moderate Hydroxychloroquine 2–6 mo Low Macular damage Sulfasalazine 1–3 mo Low Myelosuppression Leflunomide 4–12 wk Low Diarrhea, alopecia, rash, headache, risk of immunosuppression infection Minocycline 1–3 mo Low Hyperpigmentation, dizziness, vaginal yeast infections Toxicities to Monitor Myelosuppression, hepatic fibrosis and cirrhosis, pulmonary infiltrates McInnes and Schett, NEJM 2011 RA Biologics: TNF alpha blockers • TNF alpha is expressed on surface of macrophages • Binding to its receptors trigger a variety of other inflammatory cytokines • Appears to have improved efficacy in combination with methotrexate and lowers immunogenicity • Receptor blocker – Etanercept (Enbrel) • Monoclonal antibody – Infliximab (Remicade) – Adalimumab (Humira) – Golimumab (Simponi) – Certilizumab (Cimzia) RA Biologics: B and T cells • B-cell targeted therapy – Rituximab (Rituxan) is anti CD20 • Eliminates peripheral B cells within days • FDA approved in TNF alpha failures • T-cell targeted therapy – Abatacept (Orencia) is CTLA4Ig • Interferes with optimal T cell activation which results in decreased proinflammatory cytokines RA Biologics: Interleukin inhibitors • IL-1 inhibition – Anakinra (Kineret) • First biologic for RA • Not as effective in RA • Used more in JIA, Adult Still’s disease • IL-6 inhibition – Tocilizumab (Actemra) • Inhibits IL-6 signaling on cells which lowers proinflammatory cytokines RA Nonbiologics: JAK inhibitors • JAK1/JAK3 inhibition – Tofacitinib (Xeljanz) • JAK proteins are intracellular that associate with and transduce signals from several cytokine and growth factor receptors • Oral therapy, FDA approved • JAK1/JAK 2 inhibition – Baricitinib – Just finished Phase III trials RA Therapies: The Next Generation • Biosimilars • Anti-IL-6 receptor – Sarilumab • Anti-IL-17A – Secukinumab • Anti-IL-20 • Anti-CD22 – Epratuzamab • Chemokine inhibitor: CCX354-L2 • PDE4 inhibitor: aprimilast RA Therapies: Infections • Serious bacterial infection: 3-4% • TB especially in TNF alpha blockers as TNF is important in granuloma formation • Increased risk of fungal infections • Active hepatitis B Safety Issue: TB Bieber and Kavanaugh, Rheum Dis Clin N Am 30 (2004) 257-270 RA Therapies: Malignancies • TNF is important in inducing apoptosis in tumor cells • Long term use has not shown increase in solid tumors and still controversial with lymphoma • Increased risk of melanoma and nonmeloma skin cancers RA Therapies: Vaccines • Non-live vaccines recommended – Influenza injection – DTap – Pneumococcal vaccine – Hepatitis B – HPV • Live vaccines – Not recommended with biologics • Shingles, MMR, flu nasal, yellow fever, oral typhoid – Ok if prednisone <20mg, Methotrexate <0.4mg/week, azathioprine <3 mg/kg/day Together we can work to prevent this: Take Home • RA is a prevalent, inflammatory disease with potential of high morbidity both in articular and extra-articular manifestations. • Symmetrical, small joint pain and morning stiffness with joint swelling on physical exam are the most important clinical features. • Rheumatoid factor, anti-CCP antibody, and inflammatory markers are useful in diagnosis. • Modern clinical criteria allows for earlier diagnosis and more aggressive therapy to minimize joint damage. • Methotrexate is the standard disease modifying agent, but there is a low threshold to add combination therapy as we are in the era of treat to target.