Rheumatoid Arthritis and Diet
advertisement
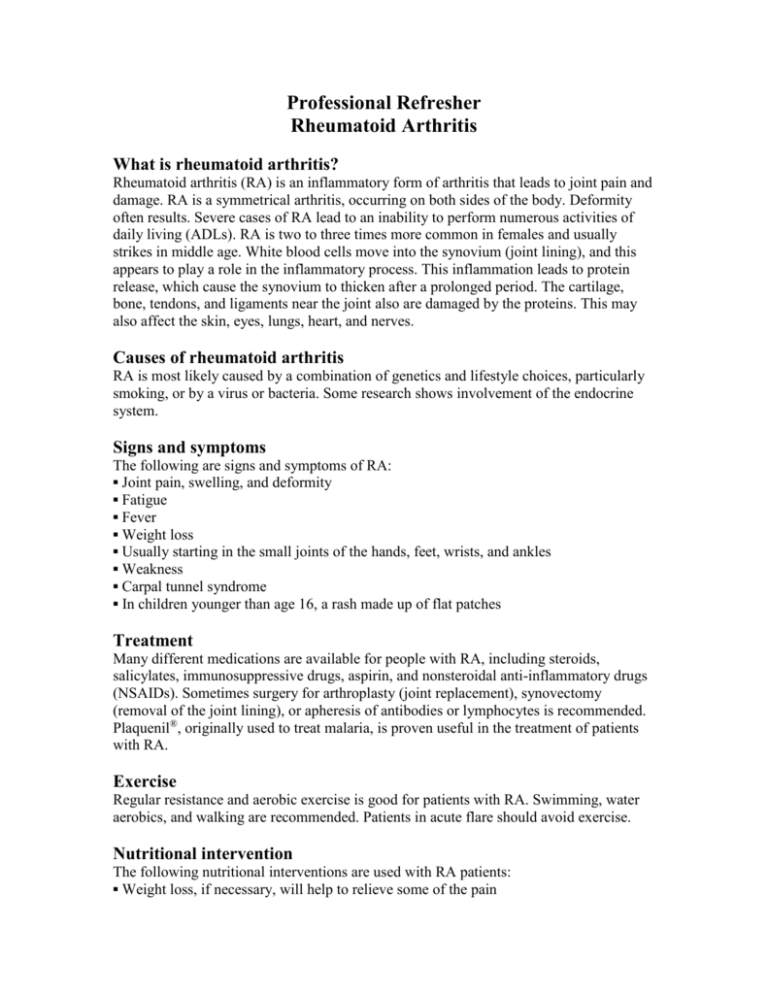
Professional Refresher Rheumatoid Arthritis What is rheumatoid arthritis? Rheumatoid arthritis (RA) is an inflammatory form of arthritis that leads to joint pain and damage. RA is a symmetrical arthritis, occurring on both sides of the body. Deformity often results. Severe cases of RA lead to an inability to perform numerous activities of daily living (ADLs). RA is two to three times more common in females and usually strikes in middle age. White blood cells move into the synovium (joint lining), and this appears to play a role in the inflammatory process. This inflammation leads to protein release, which cause the synovium to thicken after a prolonged period. The cartilage, bone, tendons, and ligaments near the joint also are damaged by the proteins. This may also affect the skin, eyes, lungs, heart, and nerves. Causes of rheumatoid arthritis RA is most likely caused by a combination of genetics and lifestyle choices, particularly smoking, or by a virus or bacteria. Some research shows involvement of the endocrine system. Signs and symptoms The following are signs and symptoms of RA: ▪ Joint pain, swelling, and deformity ▪ Fatigue ▪ Fever ▪ Weight loss ▪ Usually starting in the small joints of the hands, feet, wrists, and ankles ▪ Weakness ▪ Carpal tunnel syndrome ▪ In children younger than age 16, a rash made up of flat patches Treatment Many different medications are available for people with RA, including steroids, salicylates, immunosuppressive drugs, aspirin, and nonsteroidal anti-inflammatory drugs (NSAIDs). Sometimes surgery for arthroplasty (joint replacement), synovectomy (removal of the joint lining), or apheresis of antibodies or lymphocytes is recommended. Plaquenil®, originally used to treat malaria, is proven useful in the treatment of patients with RA. Exercise Regular resistance and aerobic exercise is good for patients with RA. Swimming, water aerobics, and walking are recommended. Patients in acute flare should avoid exercise. Nutritional intervention The following nutritional interventions are used with RA patients: ▪ Weight loss, if necessary, will help to relieve some of the pain ▪ Shopping for, preparing, and eating food is sometimes problematic, depending on the severity of the disease ▪ Tempromandibular joint (TMJ) involvement may necessitate changes to the diet consistency, as will dysphagia secondary to esophageal or pharyngeal dryness ▪ RA often leads to an increased metabolic rate; patients in active disease will require more calories ▪ RA patients require the same amount of protein as the rest of the population, and more if they are in an inflammatory phase of the disease ▪ Low-fat diets lead to lower serum levels of vitamin A and vitamin E, which stimulates lipid peroxidation and eicosanoid production; this appears to aggravate RA ▪ Anorexia is common ▪ Changes to the GI mucosa may lead to digestion and absorption issues ▪ It is sometimes useful to keep a dietary record to ascertain any association between food intake and disease flares ▪ Omega-3 fatty acids seem to decrease inflammatory responses, but interact with some medications ▪ Some studies show that omega-6 oils from evening primrose, black currant, and borage help to alleviate symptoms associated with RA ▪ Vitamin E decreases inflammation, with some studies showing that supplementation is warranted ▪ Patients with RA are most often deficient in calcium, folic acid, zinc, and selenium ▪ Vitamin D appears to act as a selective immunosuppressant; further research will determine whether this is possibly useful for the RA population References Dorfman L. Medical nutrition therapy for rheumatic disorders. In Mahan LK, EscottStump S. Krause’s food, nutrition, and diet therapy. 11th ed. Philadelphia, PA: WB Saunders; 2004:1121-1126. WebMD. Arthritis: rheumatoid arthritis basics. Available at: http://www.webmd.com/content/article/133/118609. Accessed February 18, 2008. Mayo Clinic. Rheumatoid arthritis. Available at: http://www.mayoclinic.com/health/rheumatoid-arthritis/DS00020/DSECTION=1. Accessed February 18, 2008. Review Date 3/08 G-0569