Rheumatoid arthritis - Ipswich-Year2-Med-PBL-Gp-2
advertisement

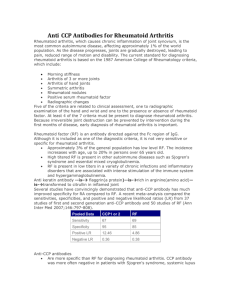
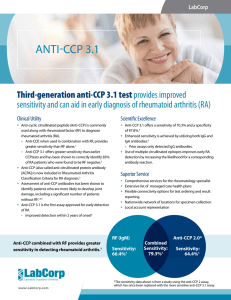
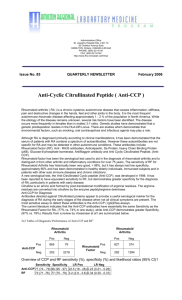
Rheumatoid arthritis Symmetric, inflammatory, peripheral polyarthritis Unknown aetiology Multi-system autoimmune disease Epidemiology 1-2% adult popn; 30-40 years at onset: F >> M RFs: smoking Immunopathogenesis Antigen-dependent activation of T cells activation and proliferation of synovial lining and endothelial cells, recruitment and activation of additional pro-inflammatory cells, secretion of cytokines+proteases by macrophages, autoantibody production Autoantibody to rheumatoid factor (anti-RF), against the Fc portion of IgG, non-specific, in 80% of RA patients (seropositive) Primary arthritogenic agent: ?EBV Genetics: multiple genes with alleles of HLA-DRB1 (30-50% of risk) o Non-HLA: PTPN22, MHC2TA, C5-TRAF1, STAT4, DCIR, REL, CD40 Autoantibodies to citrullinated protein Ags (anti-CCP) is specific, (70% of RA patients) o Anti-CCP+ RA is more aggressive Stretching of tendons/ligaments + destruction of joints (erosion of cartilage+bone) deformity Histogenesis Hyperplastic synovium with lymphoid follicles, synovial hyperplasia and giant cells Clinical features Stages of RA development: Symmetric, bilateral involvement of diarthrodial joints o Generally moves from peripheral to more proximal joints Morning stiffness (> 1 hr for > 6 weeks) Swelling of 3+ joints for > 6 weeks Swelling of wrist/MCP/PIP joints for >6 weeks Symmetric joint swelling Hand x-ray changes: erosions, bony decalcification Rheumatoid subcutaneous nodules in pressure areas (elbow, legs, fingers) 25% pts; + also in visceral organs area of necrosis with surrounding rim of palisaded macrophages RF or anti-CCP Raised ESR or CRP Extra-articular manifestations o Acute necrotising vasculitis o Lung fibrosis, pleuritis, Caplan’s syndromes o Inc risk of MI, pericarditis o Episcleritis o Renal amyloidosis o Anaemia (anaemia of chronic inflammatory diseases) o GI complications (tx) Diagnostic criteria According to up-to-date, generally need all of the following (although dx can be made in other conditions too): Inflammatory arthritis with 3+ joints Positive RF and/or anti-CCP tests Elevated CRP or ESR Other diseases have been ruled out (especially psoriatic arthritis, acute viral polyarthritis, polyarticular gout, calcium pyrophosphate deposition disease and SLE) Sx duration of >6 weeks Seronegative RA: RA and anti-CCP negative: if appropriate exclusions have been met Recent onset RA: <6 weeks if viral serologies are negative and appropriate exclusions have been met Inactive RA: no elevated acute-phase proteins but with documented past findings characteristic of RA (esp if RF and anti-CCP positive) 2010 ACR/EULAR classification criteria for RA DDx Undifferentiated arthritis (seropositive or seronegative) Fibromyalgia Seronegative spondyloarthropathies (psoriatic arthritis, reactive arthritis and associated with IBD) Connective tissue diseases: SLE Sarcoidosis Viral polyarthritis OA Polymyalgia rheumatic Crystal arthropathies Investigations RF and anti-CCP Abs tests but negative in < 20% of patients with RA ESR and CRP are both elevated ANA testing to exclude SLE and other systemic rheumatic diseases but may still be +ve FBC, eLFTs, eGFR, serum uric acid, urinalysis both to rule out other diseases and because comorbid liver/kidney diseases affect drug dosages X-ray of hands, wrists, feet more as a baseline for monitoring disease progress Treatment/management DMARDs (disease-modifying anti-rheumatic drugs) o Controls disease and prevents joint injury/disability Yearly imaging to monitor disease progression Corticosteroid injections Pain relief Monitor for drug toxicity Monitor CV risk factors Bone protection Infection prophylaxis Complications If untreated, deformity loss of physical function inability to perform ADLs and/or maintain employment Inflammation can accelerate atherosclerosis when combined with smoking/hypercholesterolemia/HT/FHx/diabetes/age