Bradford C. Ashley MD MS MPH NW Performance Medicine LLC
advertisement
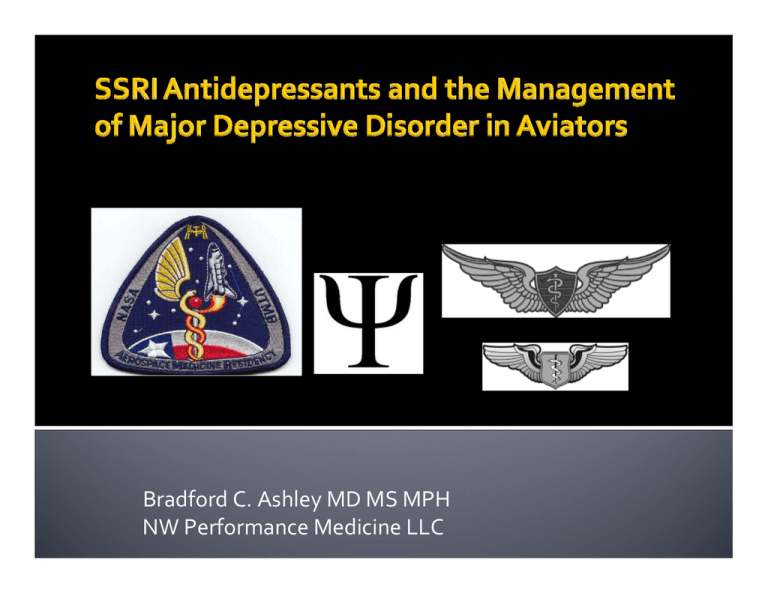
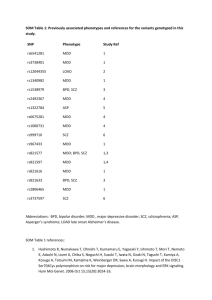
Bradford C. Ashley MD MS MPH NW Performance Medicine LLC Review DSM IV TR diagnostic criteria of Major Depressive Disorder (MDD), epidemiology, and pathophysiology Current treatment of MDD Aviation & aerospace compatible treatment options Review current aeromedical regulatory polices regarding SSRI antidepressant medication use Mood: The sustained internal emotional state of an individual. Affect: The external expression of present emotional content. Mood can be normal, elevated, or depressed. Pathologically elevated mood is labeled mania. Mania is seen in Bipolar Type I illness. Hypo mania is seen Bipolar Type II illness and Cyclothymia. Found in many psychiatric and medical conditions. A depressed mood is a symptom not a diagnosis. Physical Exam Neurological Exam Laboratory Studies (CBC with diff., CMP, TSH, FT4, B12, Vitamin D, RPR, HIV, UA, UDS) EKG (pretreatment screening for medication) Sleep Study (if at risk for OSA) Neuro‐imaging (if indicated) Mood Symptom: “Bad” Mood (Dysphoric State) *Alexathymia And‐Or Anhedodonia: No Pleasure or Motivation for Pleasure Neurovegetative Signs: Appetite or Weight Change Disturbed Sleep Psychomotor Agitation or Retardation Low Energy Poor Concentration Thought Content: Guilt or Worthlessness Suicidal Thought or Behaviors 10 Exclusions: Not due to a general medical condition or substance induced Severity Specifiers Mild Moderate Severe without psychotic features Severe with psychotic features Partial remission Full remission Chronic > 2 years Longitudinal Specifiers With full interepisodic recovery Without full interepisodic recovery With seasonal pattern With post‐partum onset Feature Specifiers Psychotic, Catatonic, Melancholic, Atypical Mild: Episodes are characterized by the presence of only five or six depressive symptoms and either mild disability or the capacity to function normally but with substantial and unusual effort. Moderate: Intermediate between mild and severe Severe: Episodes are characterized by the presence of most of the criteria symptoms and clear‐cut, observable disability (e.g. unable to work) *Severity is judged to be mild, moderate, or severe based on the number of criteria symptoms, the severity of the symptoms, and the degree of functional disability and distress. DSM IV TR p412. Lifetime prevalence of about 15% 12 month prevalence 6.6% Approximately twice as often in women (1:1.7) 50% of episodes occur between age 20 and 50 15% commit suicide National Comorbidity Survey Replication (NCS‐R) Kessler et al, JAMA June 18,2003; 289(23) 72% of people with lifetime MDD have a comorbid psychiatric disorder Anxiety Disorder – 59% Substance use disorder – 24% Impulse control disorder ‐30% National Comorbidity Survey Replication (NCS‐R) Kessler et al, JAMA June 18,2003; 289(23) Family studies: MDD found 2‐3x more frequently in relatives of those with MDD Twins: Concordance rate of 50% in monozygotic twins versus 20% in dizygotic twins Adoption Studies: Higher concordance between depressed children and biological parents than adoptive parents Serotonin–5HT Norepinephrine‐NE Dopamine‐DA First biochemical theory of MDD based on clinical observations Resperpine (depleting monoamines worsens MDD) Iproniazid (inhibiting monoamine metabolism improves MDD) Depression due to decreased monoamines (TOO SIMPLE) Exposure to stress and increases in stress hormones have been shown to decrease the expression of brain‐derived neurotrophic factor (BDNF) this leads to atrophy of the hippocampus and depression. Low P11 intracellular protein which recruits 5HT1b receptors to the neuronal surface. P11 is low in MDD. All antidepressant medication and ECT increase P11. At present no specific molecular biological theory to explain MDD pathogenesis A PET scan can compare brain activity during periods of depression (left) with normal brain activity (right). An increase of blue and green colors, along with decreased white and yellow areas, shows decreased brain activity due to depression. Decreased prefrontal metabolism L>R 20 A‐amygdala, BF‐basal forebrain, C‐cerebellum, H‐hippocampus, Hy‐ hypothalamus, NA‐nucleus accumbens, NT‐brain stem neurotransmitters, PFC‐prefrontal cortex, S‐striatum, SC‐spinal cord, T‐thalamus Hypersecretion of cortisol is present Dexamethasone suppression test (DST) positive in 50% of patients with melancholia and 80% of MDD patients with psychotic features Loss of deep slow wave sleep Increase in nocturnal arousal & awakening Reduced REM latency and increased REM density MDD is not HIBERNATION Adjustment disorder with depressed mood. Dysthymia Acute grief, Bereavement Borderline personality disorder Accurate diagnosis is critical for treatment! Treatment Principals Medications Psychotherapy ECT/TMS VNS implant Exercise Nutraceuticals ‐ OTC Acute (active symptoms) Acute (partial remission of symptoms) Acute (full remission of symptoms) Continuation (6‐12 mo. after full remission) Maintenance (prophylaxis after continuation phase) Kupfer DJ: J Clinical Psychiatry 1991:52 After 1st MDD episode in general population 25+% may relapse in one year 50‐60% may relapse in 5 years Up to 85% may relapse in 15 years Mueller & Leon, et al Am J Psychiatry 1999 156:1000‐1006 Mueller & Leon, et al Am J Psychiatry 1999 156:1000‐1006 Monoamine oxidase inhibitors Monoamine releasing agents Norepinephrine reuptake inhibitors Serotonin reuptake inhibitors Mixed norepinephrine/ serotonin uptake inhibitors Dopamine reuptake inhibitors Neurotransmitter receptor agonists Drugs with mixed actions Benzodiazepine receptor agonists 30 MAOI‐A (5HT ,NE,DA) MAOI‐B(DA, phenethylamine, tyramine) Brain MAOI‐A inhibition required for antidepressant effect Older Medications original antidepressants non‐selective & irreversible MAOI‐A & MAOI‐B Effective & Most Powerful Treatment MAOIs : excessive side effects, sedation, hypotension, food avoidance (tyramine ‐NE HTN crisis), dangerous with OTC meds (pseudoephedrine). Just Too Dangerous! Mechanism of Action Tertiary TCA – non selective Secondary TCA more selective for NE 5HT & NE reuptake inhibitors (non‐selective) Anticholinergic & Antimuscarinic blocker Alpha‐1 Blocker Histamine‐1 blocker Inhibit voltage gated sodium channels (Cardio‐Toxic) Very effective antidepressants Gold Standard for all new antidepressant drugs Aero‐medically Significant Side Effects Blurred vision ‐Ach Dry mouth ‐Ach Slow Cardiac Conduction –Na Channels Urinary retention ‐Ach Postural hypotension –alpha 1 Dizziness –alpha 1 Sedation –histamine 1 Weight gain –histamine 1 Decreased cognitive function ‐Ach Toxic in overdose (VT, torsades de pointes) Side effect profile: Not compatible with flight operations SSRI: Selective Serotonin Reuptake Inhibitor SNRI: Serotonin Norepinephrine Reuptake Inhibitor NDRI: Norepinephrine Dopamine Reuptake Inhibitor NRI: Norepinephrine Reuptake Inhibitor NaSSA: Noradrenergic and Specific Serotonergic Antidepressant SSRI: (fluoxetine, sertraline, paroxetine, fluvoxamine, citalopram, escitalopram) SNRI: (venlafaxine, desvenlafaxine, duloxetine) NDRI: (bupropion) NRI: (atomoxetine)* NaSSA: (mirtazapine) *FDA approved for treatment of ADHD only All SSRIs Equally effective Adequate trial is full dose for 4‐8 weeks 33% of those treated with a single antidepressant respond (25% relapse in 1yr) 20‐40% partial responders (76% relapse in 1yr) Critical to achieve full remission ASAP Atypical antipsychotic (aripriprazole, quetiapine) Lithium buspirone Dual therapy (SSRI +SNRI or SSRI + TCA) Thyroid hormone T3 Stimulants (amphetamine, methylphenidate) Triple AD therapy *Treatment Algorithms American Psychiatric Association TMAP – http://dshs.state.tx.us/mhprograms/tmapover.shtm Using the force Patient cooperation essential Different schools of therapy Very effective for Mild – Moderate MDD (equal to medication in elderly)* Most likely of limited benefit as mono‐therapy in severe major depression *(Am J Psychiatry 2006; 163:1493–1501) (Lower better) Medications vs CBT for Severely Depressed Outpatients: Mega‐Analysis of 4 Randomized Comparisons Am J Psychiatry 156:7, July 1999 Psychodynamic therapy (Freud, Abraham, Kohut) Medication is avoided (except in severe vegetative states Conscious and unconscious explored MDD from Ego regression, damaged self esteem Treatment to promote personality change through analyzing transference and resistance 40 Cognitive Therapy (Adler, Beck, Rush) Medication is avoided (except to break psychotherapeutic impasses) Identify self destructive cognitions MDD from distorted thinking, dysphoria due to learned negative views of self and others Treatment to provide symptomatic relief through alteration of target thoughts To promote self control over thinking patterns Therapist is an educator‐shaper Interpersonal Therapy (Meyer, Sullivan, Weissman) Medication and therapy have different effects and response timetables inline with medical model MDD from impaired interpersonal relations, absent or unsatisfactory significant social bonds Treatment to provide symptomatic relief through solution of current interpersonal problems Clarifying and managing maladaptive relationships and learning new ones through training Therapist is an explorer and a positive relationship Works by inducing a generalized seizure which releases excitatory neurotransmitters The Gold Standard of MDD tx Significant side effects Requires general anesthesia Useful in refractory cases of severe medication unresponsive major depressive illness Quick response No absolute contraindications FDA OKs TMS Depression Device Brain‐Stimulating Device Cleared for Depression Treatment After 1 Drug Failure (Oct. 8, 2008) "TMS is in no way equivalent to ECT in terms of efficacy nor in terms of safety. TMS is less effective but substantially safer than ECT," Electrically stimulates left dorsal prefrontal cortex to release excitatory neurotransmitters VNS Therapy was approved in the U.S. in 2005 as an adjunctive, long‐term treatment for chronic or recurrent depression for patients 18 year of age or older who are experiencing a major depressive episode and have not had an adequate response to four or more adequate antidepressant treatments A Tri‐monoamine Booster (Midbrain raphe ‐5HT, Locus coeruleus NE,) “Aerobic exercise at a dose consistent with public health recommendations is an effective treatment for MDD of mild to moderate severity” Am J Prev Med. 2005 Jan;28(1):140‐1. “The efficacy of exercise in patients seems generally comparable with patients receiving antidepressant medication and both tend to be better than the placebo in patients with MDD” Psychosom Med. 2007 Sep‐ Oct;69(7):587‐96. S‐adenosylmethionine (400 – 1600mg Qd)* Omega‐3 Fatty Acids (1‐9 g Qd)* St. Johns Wort (weak MAOI 600 – 1800mg Qd)* L‐Tryptophan (8‐12g divided Qid)* * Not FDA approved for the treatment of MDD What to do with pilots who have mental health issues? Major Depressive Disorder Risk of supervised treatment Risk of no treatment Risk of self treatment *Edwards, JG. Depression, antidepressants, and accidents. British Medical Journal 1995; 311(7010):887–8. *Ramaekers JG. Antidepressants and driver impairment: empirical evidence from a standard on-the-road test. Journal of Clinical Psychiatry 2003; 64(1):20–9. Effective treatment for Major Depressive Disorder Effective treatment for anxiety disorders Mild side effects for most (GI, Headache, Sexual)* Low relative cost Once a day dosing Minimal drug – drug interactions No specific toxicity when taken or mixed with alcohol (not recommended) Can be monitored by trained flight surgeon *Ireland, R.R. (2002). Pharmacological considerations for serotonin reuptake inhibitor use by aviators. Aviation, Space and Environmental Medicine, 73, 5, 421-429. 50 Concerns about cognitive performance* Concerns about daytime sleepiness* Under treatment of more serious psychiatric illness Unmasking of Bipolar Affective Disorder mania SSRI withdrawal syndrome (paroxetine) Serotonergic syndrome Sexual dysfunction, GI upset, nausea, vomiting, headaches, dizziness, anorexia, agitation, vivid nightmares/dreams, urinary retention, tinnitus, tremor, palpitations, tachycardia, restless legs, jaw tension, dry mouth, scalp muscle tension Suicidality (FDA black box 18‐24 year olds) *Paul, M.A., Grey, G. & Lange, M. (2002). The impact of sertraline on psychomotor performance. Aviation, Space and Environmental Medicine, 73, 10, 964-970. *Paul, M.A., Grey, G., Kenny, G. & Lange, M. (2002). The impact of bupropion on psychomotor performance. Aviation, Space and Environmental Medicine, 73, 11, 1094-1099. International Aeromedical Regulatory Policies Agency Psych Dx Australia CASA MDD Medication Sertraline Citalopram Venlafaxine Min. Grounding 4 wks stable rx Who P & ATC no mil w/as Co‐Pilot restr, Canada CAA + Military MDD + Post Partum Dep Sertraline Bupropion (citalopram) 6 mo stable rx US Army MDD, Anxiety, PTSD med for rx Dep FDA 3 yrs, dual rx w/ bupropion 4 mo stable rx FAA Mild‐Moderate MDD Citalopram Escitalopram Sertraline Fluoxetine 12 mo stable rx P w/as Co‐pilots P, FS, Av PA 1st, 2nd, 3rd Mil: Other aircrew Non‐rated aircrew Class medical Certificates + ATC (no Tact) ATC Npsych Testing No Cog‐S Cog‐S, Sim, In Flt Cog‐S,T,S,C,P,W Specialist Expert Tx MDD Psychiatrist Av Psych/ other HIMS‐AME Follow Up q mo x 1yr q 6mo q 6mo per Spec‐Iss “The magnitude of benefit of antidepressant medication compared with placebo increases with the severity of depression symptoms and may be minimal or nonexistent, on average, in patients with mild or moderate symptoms. For patients with very severe depression, the benefits of medication over placebo is substantial” JAMA. 2010;303(1):47‐53. Mild to moderate depressive disorders, such as 1. Major Depressive Disorder (mild to moderate) either single episode or recurrent episode 2. Dysthymic Disorder 3. Adjustment disorder with depressed mood All symptoms of the psychiatric condition for which treatment is indicated must be ameliorated by the single medication and the condition must be stable with no change in or exacerbation of symptoms for 12 months prior to certification Limited enforcement for persons who disclose before Sept 30th 2010, previous use of antidepressant medication, underlying conditions, visits to health professionals regarding antidepressant use. 12 months Grounding Only 4 antidepressants approved Case by Case basis “It is not likely that all applications will result in the issuance of a certificate under section 67.401”* *Specifically Unacceptable diagnoses and or symptoms: Treatment with multiple antidepressant medications concurrently or History of multi‐agent drug protocol use (prior use of other psychiatric drugs in conjunction with antidepressant medications) Accurate psychiatric diagnosis of single episode of Major Depressive Disorder (DSM IV TR) No previous psychiatric history No active or recent suicidal ideation, no psychotic symptoms Rule out medical issues (endocrine, neurological, infectious, drug side effects…) Explore all possible non‐pharmacological treatments (psychotherapy, exercise, environmental, changing physical health medications) Aviation psychiatric consultation available Pilot motivated and willing to participate in all recommended treatment with ongoing monitoring Pilot unable to achieve acceptable symptom control off antidepressant medication or psychiatric need to remain on medication Exercise has antidepressant effects Computer‐Assisted cognitive therapy for Depression is a efficacious as standard cognitive therapy Telephone Psychotherapy Enhances Antidepressant Pharmacotherapy ISS med kit (sertraline, TCA) MDD is a common mental health condition Treatment needs to be quick and effective Only a few treatments are Aeromedically appropriate Aeromedical regulatory agencies need to develop policies that encourage effective treatment and instill hope in the pilot that they can get recertified in a timely fashion Bradford C. Ashley MD MS MPH NW Performance Medicine LLC flightmedicine@verizon.net