Treatment Outcomes in Low-Income Depressed Women with and
advertisement
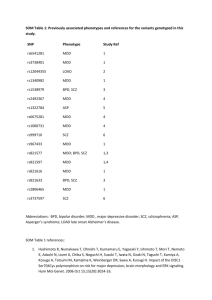
TREATMENT OUTCOMES IN LOW-INCOME DEPRESSED WOMEN WITH AND WITHOUT POSTTRAUMATIC STRESS DISORDER Joyce Y. Chung, M.D., Juned Siddique, M.S., Bonnie Green, Ph.D., Katherine Beebe, Ph.D., Erica Wetherhold, B.S.N., Jeanne Miranda, Ph.D. ABSTRACT Objective: We evaluated treatment outcomes in low-income depressed women with and without comorbid PTSD to determine whether comorbidity affects treatment response. Methods: The WECare study is a treatment intervention study for MDD that focuses on low-income mostly minority women. We report clinical outcomes for the first 61 subjects treated with either CBT or paroxetine. Fifty-four percent had both MDD and PTSD at the time of study enrollment. Ethnic representation: African American 69%, Hispanic 25% and White 7%. Demographic characteristics: mean age 30.6, mean number of children 2.4, married 33%, uninsured 53%, Medicaid 22%. Baseline HAMD/HAM-A scores for CBT subjects were: MDD alone 15.1/16.1, MDD+PTSD 16.6/14.2; for medication subjects: MDD alone 17.0/15.6, MDD+PTSD 19.2/17.6. Results: CBT subjects’ 6 month mean change in HAM-D scores: 6.5 (MDD) and 9.9 (MDD+PTSD). Antidepressant subjects’ 6 month mean change in HAM-D scores: 8.4 (MDD) and 12.5 (MDD+PTSD). Six-month mean change in HAM-A scores for CBT subjects: 5.5 (MDD) and 6.8 (MDD+PTSD). Six-month mean change in HAM-A scores for medication subjects: 8.1 (MDD) and 11.9 (MDD+PTSD). SF-36 summary scores improved for all subjects. Conclusions: Subjects with MDD and comorbid PTSD treated with either CBT or paroxetine did as well, if not better, than subjects with MDD alone. Our findings support the effectiveness of standard treatments for depression in low-income women with complex psychiatric profiles. INTRODUCTION Depressive and anxiety disorders often co-exist. Research is needed to examine the effectiveness of treatment when more than one condition is present. Our study carefully evaluates subjects with Major Depressive Disorder for trauma and the diagnosis of posttraumatic stress disorder. The objective of this analysis is to examine whether comorbid posttraumatic stress disorder in association with major depressive disorder affects treatment outcome with standard treatments for depression. STUDY CHARACTERISTICS The WECare (Women Entering Care) study at Georgetown University enrolls economically disadvantaged African American, Hispanic and white women with Major Depressive Disorder into a randomized trial of antidepressant medications, cognitive behavioral group therapy or usual care. Study subjects are women 18 years or older who are recruited from community based programs in the Washington, DC metropolitan area that serve low-income women and families. The primary sites for recruitment are family planning clinics, WIC (Women, Infant, Child) programs, and pediatric/primary care clinics for indigent/under-insured patients. Patients qualify for the study if they screen positive for possible depression using a version of the PRIME-MD, and then are found to meet criteria for Major Depressive Disorder on a phone administered CIDI. Depression severity is assessed using a modified version of the HAM-D (6 additional items about atypical symptoms of depression); subjects must enter the study with a score or 14 or greater on the modified HAM-D. The WECare study population is unique and we have been gathering data about characteristics of depressive and anxiety disorders in this population as well as how to effectively treat these problems. To date we have enrolled 216 women with major depressive disorder in the study, 114 (53%) African American, 13 (6%) white, and 89 (41%) Hispanic. In addition we have enrolled 54 non-depressed comparison subjects. TREATMENT CHARACTERISTICS After assignment to either treatment arm, subjects may be seen in up to four education meetings to prepare them for treatment. Antidepressant treatment Subjects are offered treatment with 24 weeks of antidepressant medication using AHCPR treatment guidelines and administered by primary care nurse practitioners supervised by a psychiatrist. The first-line medication offered is paroxetine; the secondline treatment is buproprion (if paroxetine is not tolerated or effective). Dosing protocols of the medications were developed so that antidepressant treatment is standardized. Increases in antidepressant medication dosage are made according to the dosing protocols, side effects, and serial scores on the modified HAM-D. Subjects are seen in face-to-face meetings every two to four weeks during treatment with medications. There is weekly phone contact with the nurse practitioner throughout the treatment phase. Psychotherapy treatment: Subjects are enrolled in group treatment consisting of eight weekly sessions of cognitive behavioral therapy using a standardized manual and conducted by psychologists trained in CBT. For subjects who remain depressed or have partial resolution of depression after eight weeks, a second eightweek module is offered. If group treatment is not feasible, individual CBT in eightweek modules is provided in lieu of group. Usual care condition Usual care consists of informing subjects about their depression diagnosis, educating them about treatment for depression, and offering assistance with a referral to mental health services available in the community. Subjects assigned to usual care are followed via ten phone interviews in the course of a year. STUDY SAMPLE To date, 98 subjects have been assigned to treatment with CBT or antidepressant medications and have been assessed at 3 or 6 months after study enrollment. In order to select subjects who received an adequate course of treatment, we defined treatment in the following manner. Antidepressant treatment is defined as at least nine weeks of medication (either paroxetine or buproprion). Psychotherapy is defined as at least five sessions of CBT in either group or individual format. Using these definitions, 61 of the 98 subjects received treatment for depression (62%). Thirty-three of the 61 subjects received antidepressant medication with a mean duration of 21 weeks. Twenty-eight subjects received psychotherapy with a mean number of sessions of 8.3. DEMOGRAPHICS See Tables TRAUMA EXPOSURE AND PTSD Multiple traumas were reported by 53 of 61 treated subjects (86.9%). Interpersonal trauma, such as sexual or physical assault, was the most common type of trauma reported. Twenty-seven (44.3%) of the women reported being physically forced to have intercourse. Comorbid PTSD was present in 54.1% of our treated sample: essentially the same rate as in the overall WECare study population (55%). Baseline Hamilton depression and anxiety scores were similar between subjects with MDD alone compared with those with both MDD and PTSD (see tables). RESULTS See Tables Subjects treated with CBT or antidepressant medications improved on measures of depression and anxiety symptom severity (HAM-D and HAM-A) as well as on measures of functioning (SF-36). Contrary to our initial hypothesis, there were no significant differences in mean depression score changes between CBT subjects who had comorbid PTSD at either 3 or 6 months when compared to subjects with MDD alone. The same was true for the comparison of subjects treated with antidepressant medication. Similarly, 6-month mean changes in HAM-A scores for CBT and antidepressant treated subjects were not significantly different for those with MDD alone or both MDD and PTSD. SF-36 summary scores improved for all subjects regardless of comorbidity. Medication subjects with both MDD and PTSD functioned significantly better than those with MDD alone in measures of role limitations due to emotional problems and emotional wellbeing. CONCLUSIONS Subjects with MDD and comorbid PTSD treated with either CBT or antidepressant medication did as well, if not better, than subjects with MDD alone. In our study, women with major depressive disorder in the context of current PTSD who were treated with antidepressant medication responded particularly well despite having more than one current psychiatric disorder. Our findings support the effectiveness of standard treatments for depression in low-income women with complex psychiatric profiles. REFERENCES 1. Sherbourne, C., & Wells, K. “The Course of Depression in Patients with Comorbid Anxiety Disorders.” J Affective Disorder, 43(3):245-250, 1997. 2. Brown, G., Schulberg H., Madonia, M., Shear M., & Houck, P. “Treatment Outcomes for Primary Care Patients with Major Depression and Lifetime Anxiety Disorders.” American Journal of Psychiatry, 153(10):1293-1300, 1996.