Acknowledgements Methods to manage respiratory motion in radiation treatment
advertisement

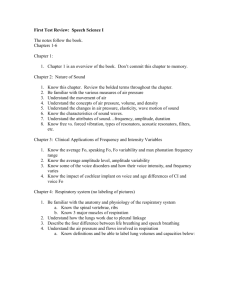
Acknowledgements Methods to manage respiratory motion in radiation treatment William Beaumont Hospital , Royal Oak, MI Remouchamps, Letts, Yan, Kestin, Vicini, Martinez Memorial Sloan Kettering Cancer Center, NY, NY G. Mageras, E. Yorke, E. Ford Oakwood Hospital, Dearborn, MI O. Salazar John Wong William Beaumont Hospital Royal Oak, USA Princess Margaret Hospital, Toronto,Canada D. Jaffray, M. Sharpe NCI (USA) and Elekta Inc. Respiratory Trace by Spirometry Respiratory Motion 7 • • • • • Quiet breathing is an involuntary action Periodic in response to chemo-receptors, mainly CO2 Breathing cycle ~ 14 breathes per min ~ 4 sec and 400 – 500 cc / breath Diaphragmatic excursion : – > 1 – 2 cm quiet; > 4 cm voluntary deep breathing • Clinical Sites: lung ca, liver ca, pancreas ca, breast, lymphoma Mechanics of Breathing Time 6 Maximum inspiratory capacity 5 Liters 4 3 Tidal volume 2 1 Vital capacity Total lung capacity Functional residual capacity Residual volume 0 Mechanics of Breathing Inspiration : mostly due to diaphragmatic contraction O O Expiration: Passive relaxation O O O DIAPHRAGM THORAX O 1 Respiration motion is non-uniform in 3D A. Breath-hold 1 B. Breath-hold 2 B-A Deep inspiration breath-hold • immobilization • local cardiac motion A. End Normal Expiration B-A B. End Normal Inspiration Methods to manage breathing motion • Gating (MSKCC) : – turn radiation on/off at a specific breathing phase • Tracking (MCV) : – synchronize beam motion with breathing motion • Immobilization : – voluntary deep inspiration breath-hold (MSKCC) – active breathing control (WBH) • Optimize free-breathing PTV (UM, NKI, WBH) Respiratory Gating System: Varian Real-time Position Management (RPM) Components: Managing Respiratory Motion: Surrogate and Margin • Validity of the surrogate signal to breathing motion – Gating/Tracking : Reflective external body markers – Breath-hold : lung volumes with spirometry • Margin determination: – Identify the margin achievable with the method • fluoroscopy, CT – Match the appropriate method to resource available, patient acceptance and clinical goal RPM - Record/Playback RPM - Record/Playback • Initial tracking determines min/ max marker position. • Recorded fluoroscopy is synchronized with the external marker position. CCD • Reflective external marker placed on abdomen or chest Breathing monitor • Infrared illuminator/ CCD camera • Workstation to process signals & generate trigger for CT/simulator/linac On/off Control workstation Treatment machine Marker position vs time • User specifies a treatment point in breathing cycle via threshold levels (amplitude based). • Bottom trace indicates beam enable intervals. • More recent: phase-based gating option 2 Initial clinical experience with gating Effect of instruction on patient breathing Example Patient Breathing Signal • Patients given recorded instruction (“breathe in, breathe out”) • Instruction affects breathing pattern in 2 ways: • Changes in patient breathing can affect gating performance • At simulation, thresholds set to gate at end expiration. • At treatment, irregular breathing can cause beam enable at unintended intervals. 183157 lung ap 1 Treatment session Marker vs Time 3 No Instruct 2 Marker Position (cm) Fluoroscopy session 183157 lung ap 10 Larger amplitude 1 0 3 0 5 10 15 20 25 30 Less variation in peak position With Instruct 2 1 0 0 5 10 15 20 25 30 Time (s) External monitor vs internal anatomic motion: Automatic tracking of lung anatomy in fluoroscopy Example Diaphragm / External Marker Correlation Fluoroscopy No Instruction 2.0 Diaphragm Marker 6.5 1.5 1.0 Diaphragm Position (cm) Diaphragm Position (cm) 1.5 0.5 0.0 0.0 2.5 0.5 1.0 1.5 With Instruction 2.0 6.0 1.0 5.52.0 0.5 5.0 1.5 0.0 4.5 100 1.0 Marker Position (cm) 2.5 200 0.5 300 400 Time (seconds x10) 0.0 0.0 0.5 1.0 1.5 2.0 Marker Position (cm) Example phase delay in diaphragm motion Diaphragm 0.5 0.0 0.7s 0.0 0 10 20 30 0.7s delay applied to marker waveform 40 Diaphragm Position (cm) Time (s) 1.0 1.0 0.5 0.5 0.0 0.0 0.5 Marker Position (cm) 1.0 0.0 0.0 0.5 Marker Position (cm) 1.0 Variability, SD (mm) 1.0 0.5 Marker Position (cm) Diaphragm Position (cm) Diaphragm Variability (SD) : Fluoro vs Treatment 1.5 Marker 1.0 Fluoro: No Gate Fluoro: Gate Tx Localization Film 10 8 6.9±2.1 mm 6 4 2.8±1.0 mm 2.6±1.7 mm 2 0 1 2 3 4 5 6 7 8 Patient 3 Comparison unsynchronized vs RTCT RPM – Respiratory Triggered CT (RTCT) • RTCT: – Acquisition in axial mode – Each gate triggers 1 CT slice Inspiration Free Breathing Expiration #2 Expiration #1 CT Reproducibility – other organs • Average S-I shifts for all organs: – E-I shift: 12.8 mm (range: 3.0 - 29.2 mm) – E-E shift: 2.0 mm (range: 0.0 - 6.4 mm) Diaphragm Reproducibility • 10 liver patients simulated, 8 treated (177 treatments) with gating at end-expiration 20 18 Displacement (mm) 16 Fluoro data 14 12 10 8 6 CT data Avg. △S-I (mm) Gated Ungated Avg. △S-I (mm) E-E E-I R Diaphragm 3.9 14.7 R Diaphragm 2.2 11.5 L Diaphragm 3.8 21.4 4 2 0 Liver R Kidney L Kidney Sup-inf, E-I Spleen GTV Sup-inf, E-E Film-based verification of lung position/inflation during gating Gated film / EPI: respiration motion variation Diaphragm-vertebral displacement relative to DRR Patient #1 4 2 0 0 Number 2 4 insp 2 0 #3 4 #6 0 #7 4 2 2 0 0 #4 mean 4 insp 2 #8 4 2 0 0 Gated Localization Film Number #2 4 DRR from Exhale CT Patient #5 4 2 -10 Superior -5 0 5 10 Displacement (mm) Inferior Lung Treatment -10 Superior -5 0 5 10 Displacement (mm) Inferior Liver Treatment 4 Managing Respiration Motion: Respiration Correlated CT (RCCT) Respiratory gated treatment summary Gated RT: • • • • • • 10 patients treated to date (2 lung, 8 liver) 8 patients gated at end exhale, 2 at end inhale Preserve patient’s comfort at free breathing Regular breathing important, instruction helps Setup needs to be characterized for systematic correction Breathing motion reduced to 5mm (exhale); PTV ~ 10mm or unchanged • Treatment session times increased ~5min, mostly due to decreased beam duty cycle Standard Free breathing • Respiration-triggered CT Î images at only 1 phase, acquisition times 4-5x longer • Cannot determine free-breathing PTV for ungated treatment Respiration correlated CT: • Adapted from Kachelriess & Kalender 1998 • “4D” imaging – 3D images at 8-10 phases Î treatment volume better approximates target RCCT – Acquisition Resp. triggered End expiration RCCT – Retrospective correlation Slow table: Pitch 0.5; 0.5mm spacing (0.5s) 5mm Time or z 3mm thick time 0 5 0 1 0 0 1 5 0 Spiral CT trajectory X A x is T it le CT slices 2 0 0 5 0 0 1s 5 0 1 0 0 X Varian RPM system A x is 1 5 0 2 0 0 5 0 T it le Slices at end exhale Slices at end inhale Slices at intermediate phase Respiration trace Î Time stamp each CT slice with phase RCTC : Phantom Study RTTC: Phantom study Static RTCT 0.0 0.6 1.3 1.9 2.5 3.1 3.8 4.4 5.0 5.7 Moving RCCT Number of unique phases is a function of: respiratory period, CT rotation period, fraction of rotation information 5 RCCT - Treatment planning: RCCT – Summary Internal target volume definition Intra-fractional motion GTV SI 0 A P Position (cm) -1 GTV AP 0 ITV ungated -1 0 Diaphragm -1 Gate 1 RPM Trace • Potential benefits to RT planning: – Intra-fx motion info Î improve PTV defintion for breathing motion – Deformable registration models Î dose to moving organs – Simulate errors for standard CT & RT Î what is effect on dose to organs for std RT, how much will RCCT benefit RT? • RTTC : – PQ5000: 8-10 phases, 5mm spacing, 1s/slice, 9 cm scan 0 0 1 2 3 4 5 Time (s) ITV gated Cine CT – Patient 1 10 phases @ 0.5s Clinac 23EX mounted with dual X-ray sources and flat panel X-ray sensors Fig 1 • 4-slice CT: 30cm scan, 2.5mm spacing, 0.5s/slice • Allow validation of surrogate signal for gating or tracking Y. Takai, 1 et al, 1Department of Radiation Oncology, School of Medicine, Tohoku University, Sendai, Japan, 2Varian Medical Systems, CA, USA Image processing courtesy Tinsu Pan Fig 4 Real-time tracking of a gold seed in lung cancer with DFFP system Fig 6 Tracking virtual respiratory motion (one cycle) End-exhale End-inhale 6 Management of respiratory motion: Breath-hold techniques DIBH - Patient Setup at MSKCC • Breath-hold is immobilization; and reproducible if the breathing pattern does not deviate significantly • End inspiration or deep inspiration to increase separation of thoracic contents • Voluntary Breath-hold Techniques – MSKCC : instruction based on spirometry – Cross Cancer Center : instruction without monitoring signal • Active Breathing Control/Coordinator – Beaumont : digital spirometry linked to a computer controlled valve (a) Normal breathing (b) ABC (c) ABC 30 min. later DIBH Summary • Over 20 patients treated since 2/98 at MSKCC; breath-hold duration of 10 sec • No margin reduction at present • Dose increase from 69.4 to 87.9 Gy (ave.) possible with NTCP <25% • 3-5 mm margin seems possible (MSKCC, Beaumont) • Simulation and treatment times ~ 1.5X longer • Compliance hurdle at MSKCC: – ~1/2 of patients unable to perform procedure – patient fatigue (Rosenzweig ‘00) Active Breathing Control (ABC) • ABC is a technique to immobilize respiratory motion repeatedly and reproducibly for a period of time that can be comfortably tolerated by the patient • Moderate deep inspiration breath-hold (mDIBH) at 75% to 80% of maximum inspiration capacity to – displace of thoracic contents – avoid tiring the patient • Patient selection; long breath-hold (>15 sec) is desirable • Therapists involve in verbal coaching ABC Apparatus Valve Flow Meter Mouthpiece 7 ABC at Beaumont Visual display of breathing motion ABC Margin Determination : CT Study Protocol • CT protocol to set PTV for breathing motion – 2 scans at mDIBH – 1 end inspiration (NI), 1 end expiration (NE) – repeat 1 mDIBH 1 to 2 weeks later • Left sided breast patients as surrogate for evaluation of lung immobilization • Breath-hold duration based on individual patient Segmental - Regional analysis of left and right lung separately • Repeat (intra and inter-fraction) CT scans registered using the bony landmark. • Lungs and main bronchi are contoured as surrogates for internal thoracic contents. Intra- and Inter-fraction Lung Reproducibility: Distance-to-agreement (cm) 0.7 0.6 0.35 0.3 0.0 0.0 • Surrogates for 3D distance-to-agreement (DTA) measurements – Lung surface for chest wall motion (~ 300,000 points) – trachea and main bronchus alignments show results similar with lung surface data 8 Lung surface distance to agreement : mean (SD) in cm Lung surface distance to agreement : mean (SD) in cm between 2 registered mDIBH intra-fraction ABC Scans between 2 registered mDIBH intra-fraction ABC Scans INTRA-FRACTION (Same day) Full Lung Region I II III IV V Region VI (Bottom (20%) (20%) (20%) (20%) (Top 10%) 10%) Left 0.19 Lung (0.32) 0.43 (0.56) 0.25 0.15 0.14 0.14 (0.38) (0.20) (0.17) (0.17) 0.14 (0.17) Right 0.22 Lung (0.33) 0.44 (0.54) 0.35 0.17 0.14 0.13 (0.46) (0.20) (0.16) (0.15) 0.15 (0.20) Alpha Cradle Left 0.11 Lung (0.12) 0.17 (0.15) 0.15 0.10 0.09 0.08 (0.14) (0.09) (0.08) (0.08) 0.09 (0.07) 14 patients Right 0.10 Lung (0.11) 0.10 (0.10) 0.12 0.09 0.09 0.08 (0.13) (0.08) (0.08) (0.08) 0.13 (0.09) No Cradle 7 patients ABC Margin Studies : Summary • The lung surface is well immobilized with ABC at mDIBH – 3 mm margin for superior 7/10th of lung – 6 mm margin for inferior 3/10th of lung, (diaphragmatic regions) • Similar results observed with the trachea/carina and main bronchi; maybe applicable for internals of the lung • Setup compromises breathing immoblization with ABC • mDIBH is highly reproducible: – minimizes the variation in breathing pattern – expanded lung volume less sensitive to positional variation Free Breathing Alpha Cradle Immobilization INTRAFRACTION (Same day) 14 patients INTERFRACTION (2-3 weeks later) 8 patients Full Lung Region I II (Bottom (20% ) 10%) III (20%) IV V Region VI (20%) (20%) (Top 10%) Left 0.11 Lung (0.12) 0.17 (0.15) 0.15 (0.14) 0.10 0.09 0.08 (0.09) (0.08) (0.08) 0.09 (0.07) Right 0.10 Lung (0.11) 0.10 (0.10) 0.12 (0.13) 0.09 0.09 0.08 (0.08) (0.08) (0.08) 0.13 (0.09) Left 0.13 Lung (0.15) 0.17 (0.15) 0.17 (0.20) 0.11 0.09 0.10 (0.12) (0.09) (0.09) 0.15 (0.10) Right 0.14 Lung (0.16) 0.19 (0.18) 0.17 (0.20) 0.12 0.11 0.12 (0.09) (0.10) (0.11) 0.16 (0.12) ABC : Clinical Implementation • IMRT for left sided breast --- mDIBH to reduce heart dose – >50 patients CT planning and margin studies at Beaumont, Royal Marsden – 20 treated with IMRT at Beaumont • Lung --- tumor immobilization – Royal Marsden (UK), Mount Vernon (UK), Oakwood Hospital, University of Colorado, Beaumont ….. – patients selected to maintain breath-hold >15s – > 30 patients CT studied; > 20 treated with SRS • Liver --- > 50 patients treated at Oakwood, U of Michigan mDIBH Treatment Procedure CT DRR • Treatment slot of 20 min • Patient positioned during free breathing • Field matches tattoo during FB • ~ 5s mDIBH to set anterior SSD • Shift / gantry rotation during FB • IMRT/ABC complete in 15 min 9 Breathing Trace - Daily Treatment Coaching (Karaoke) by the Therapists 2.5 Medial Set up Lateral 2 1.5 1 0.5 0 EPI -0.5 0 100 200 EPI 300 EPI 400 EPI 500 600 Time (seconds) Left Sided Breast Treatment with ABC at mDIBH Electronic Portal Image Prescription DRR/Sim film • 20 patients treated to date • Average breath-hold duration : – 20 sec at 1.8 liters, 2 per tangents • Heart V(30) : – free-breathing 3.5% (1% - 10%); ABC 0.1% (0% - 0.6%) • Lung V(20): – free-breathing 11.6% (8% - 18%); ABC 10.4% (8% - 14%) Intra-fraction reproducibility: Difference in positioning errors between 2 BH’s (mm) MEDIAL N Transverse Radiation Ablation Treatment with ABC and Body Frame LATERAL Cranio-caudal Transverse Cranio-caudal Mean SD Mean SD Mean SD Mean SD 1.3 1.0 2.0 2.5 1.3 1.0 1.8 1.5 11 Combined Set up and Breath-hold errors (in mm) – (11 patients, 255 to 268 EPIs per beam, 1054 EPIs) Medial BH1 Medial BH2 Lateral BH1 Lateral BH2 Mean SD Mean SD Mean SD Mean SD Transverse 1.3 2.5 1.4 2.3 1.9 2.3 2.3 2.4 Cranio-caudal 2.6 3.0 2.3 2.9 2.5 3.1 3.1 3.2 Rotation 1.1 1.1 1.2 1.0 1.3 1.0 1.0 1.0 Courtesy of Dr. Omar Salazar 10 Radio-ablation of Lung Tumors PTV dose 70%: 10 Gy/fraction /week Ave. Equiv. Irradiaed Sphere Vol (cc) (cc) Vol Range (cc) Mean Dose in PTV (Gy) 3.5 2 – 182 51 37 140 3.3 5.2 4 – 490 55 36 146 5.3 Category n ABC-Lung 14 42 primary Non-ABC Lung primary 9 17 4 46 Courtesy of Dr. Omar Salazar • ABC procedures well accepted by selected patients and staff • Accurate treatment reproducibility • Reductions in the heart dose for left sided breast RT • Dose escalation for radio-ablation of lung tumors A Word of Caution - Dosimetric Margin • Penumbra causes collateral normal tissue irradiation. • Typical distance between 95-50% isodose: – ~10mm in water – ~21mm in lung 1.0 18MV water 0.8 Relative Dose ABC Summary lung 0.6 10x10cm2 100cm SSD 5cm depth 0.4 0.2 0.0 -10 -5 0 5 10 Distance from Central Axis [cm] No inhomogenity correction 1 cm PTV, 8 mm aperture offset 110 105 95 50 20 Superposition calculation 1 cm PTV, 8 mm aperture offset 110 105 95 50 20 11 Superposition calculation; 4 mm aperture offset; Sharp beam: 15% fluence increase to 15 mm internal rind 110 105 95 50 20 Conclusions • RCCT facilitates organ motion evaluation • Gating and ABC are both viable options to reducing margin for respiratory motion • ABC: – pro : active immobilization, highly reproducible – con : not tolerated by all patient • Gating: – pro : patient comfort – con : larger margin, reduced duty cycle (tracking solution) • Long term studies required – change of motion • A combination approach seems most appropriate 12