The Virtual Nurse: Adding Value to the Perioperative Experience
advertisement

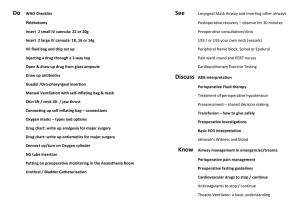
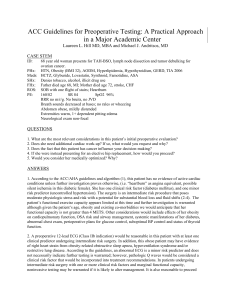
The Virtual Nurse: Adding Value to the Perioperative Experience Laura Hollis, MSN, RN, CCRN; Julie Hamm, MSN, ACNP-BC; Kristy Bishop, ADN, RN3 Vanderbilt University Medical Center BACKGROUND PROCESS OF IMPLEMENTATION IMPLICATIONS Due to high surgical volume in an academic medical center, there were continuous challenges with the optimization of surgical patients. The need to touch more patients for anesthesia preparation created an opportunity for innovative strategies to add value to the organization and the patient experience. Innovative technology was crucial to assist in the assessment of patient information and quickly communicate regarding appointments, current medications, plan of care, and medical history. A multidisciplinary team worked to devise a program pilot proving feasibility to have an RN call American Society of Anesthesiology Physical Status Classification (ASA Class) 1 & 2 patients preoperatively. A Nurse Practitioner (NP) conducted the pilot and showed success. The RN position was hired and the program began looking to touch more patients and add value to day of surgery preparedness. An additional RN FTE and two PRN RN positions were hired to facilitate this work. A Clinical Lead NP role was developed to review cases with RNs, act as a liaison with the anesthesiologists, and serve as a resource, mentor, and educator. Several technologies have been incorporated into these roles to provide an immediate view of the information for real time decision making. Patient preparation with the use of preoperative RN “virtual” visits adds a level of convenience for patients, eliminates patient clinic wait time, cost of getting to a clinic visit, as well as improves day of surgery flow and downtime within the perioperative system. This work has also shown improved satisfaction and quality for patients, physicians, and staff. RN VOLUME PURPOSE Utilize nurse (RN) callers to optimize the patient experience and satisfaction with the use of a “virtual” phone call option for the preoperative anesthesia evaluation as well as add value to other aspects of the perioperative arena. Optimizing patient records reduces time spent day of surgery seeking information, additional patient testing, and decreases risk of cancellation. RN Volume 350 300 250 200 150 100 50 0 July August September October November December January February March April May June July August September Volume steadily increasing with onboarding staff. Patient and Staff satisfaction/engagement vital to success. TECHNOLOGIES OBJECTIVE Create RN positions that would complete “virtual” appointments using technology to facilitate pertinent patient information for anesthesia providers in order to add value to the patient experience and optimize perioperative patient movement on the day of surgery. CONCLUSION To optimize the patient experience and add value to perioperative system, the role of the RN caller has been developed and incorporated to provide current patient information and medication reconciliation preoperatively without an in-person appointment. Retrieval of outside records and other pertinent information allows for improved patient preparation for day of surgery. This role has increased perioperative efficiency and productivity as well as created an opportunity to reach more patients that previous efforts allowed. Technology has improved communication with patients as well as within the clinic and organization. Growth and development of this program has expanded the number of FTEs as well as provided an opportunity for growth and development of nursing staff. REFERENCES LYNC application through Outlook, along with Clinic Whiteboard and Message Basket applications within StarPanel, create real time data streaming enhancing communication and situational awareness thus increasing productivity. Vanderbilt Preoperative Evaluation Center website. (2014). https://vandypoint.mc.vanderbilt.edu/sites/anesthesiology/VPEC/SitePages/Home.aspx