ORIGINAL CONTRIBUTION
Association of Perioperative -Blockade
With Mortality and Cardiovascular Morbidity
Following Major Noncardiac Surgery
Martin J. London, MD
Kwan Hur, PhD
Gregory G. Schwartz, MD, PhD
William G. Henderson, PhD, MPH
T
HE EFFECTIVENESS AND SAFETY
of perioperative -blockade for
patients undergoing noncardiac surgery remains controversial.1 Class I recommendations in the
current American Heart Association/
American College of Cardiology Foundation (AHA/ACCF) Guidelines on Perioperative Evaluation and Care for
Noncardiac Surgery remain limited to
continuation of preexisting -blockade.2
Given medical and ethical concerns regarding withdrawal of patients from preexisting -blockade and the expense of
conducting randomized clinical trials
powered to determine effects on perioperative outcomes, observational analyses have been used to aid in clinical decision making regarding perioperative
-blockade. However, observational
analyses have been largely limited by
single-center data or by an inability to
capture data from the actual perioperative period. Lindenauer et al,3 using a
managed care administrative database,
reported a large multicenter analysis of
in-hospital perioperative -blockade, relating exposure to -blockers during the
first 2 days of hospitalization to inhospital mortality. Using propensity
matching and subclassification on the revised Cardiac Risk Index (CRI) predictors, an association of perioperative
-blockade with a lower rate of mortality was demonstrated in patients with 2
or more predictors.4 In those with none
or only 1 predictor, treatment was asso1704
Importance The effectiveness of perioperative -blockade in patients undergoing
noncardiac surgery remains controversial.
Objective To determine the associations of early perioperative exposure to -blockers with 30-day postoperative outcome in patients undergoing noncardiac surgery.
Design, Setting, and Patients A retrospective cohort analysis evaluating exposure
to -blockers on the day of or following major noncardiac surgery among a populationbased sample of 136 745 patients who were 1:1 matched on propensity scores (37 805
matched pairs) treated at 104 VA medical centers from January 2005 through August 2010.
Main Outcomes and Measures All cause 30-day mortality and cardiac morbidity (cardiac arrest or Q-wave myocardial infarction).
Results Overall 55 138 patients (40.3%) were exposed to -blockers. Exposure was
higher in the 66.7% of 13 863 patients undergoing vascular surgery (95% CI, 65.9%67.5%) than in the 37.4% of 122 882 patients undergoing nonvascular surgery (95%
CI, 37.1%-37.6%; P⬍.001). Exposure increased as Revised Cardiac Risk Index factors increased, with 25.3% (95% CI, 24.9%-25.6%) of those with no risk vs 71.3%
(95% CI, 69.5%-73.2%) of those with 4 risk factors or more exposed to -blockers
(P⬍.001). Death occurred among 1.1% (95% CI, 1.1%-1.2%) and cardiac morbidity occurred among 0.9% (95% CI, 0.8%-0.9%) of patients. In the propensity matched
cohort, exposure was associated with lower mortality (relative risk [RR], 0.73; 95%
CI, 0.65-0.83; P⬍.001; number need to treat [NNT], 241; 95% CI, 173-397). When
stratified by cumulative numbers of Revised Cardiac Risk Index factors, -blocker exposure was associated with significantly lower mortality among patients with 2 factors (RR, 0.63 [95% CI, 0.50-0.80]; P⬍.001; NNT, 105 [95% CI, 69-212]), 3 factors
(RR, 0.54 [95% CI, 0.39-0.73]; P⬍.001; NNT, 41 [95% CI, 28-80]), or 4 factors or
more (RR, 0.40 [95% CI, 0.25-0.73]; P⬍.001; NNT, 18 [95% CI, 12-34]). This association was limited to patients undergoing nonvascular surgery. -Blocker exposure
was also associated with a lower rate of nonfatal Q-wave infarction or cardiac arrest
(RR, 0.67 [95% CI, 0.57-0.79]; P⬍.001; NNT, 339 [95% CI, 240-582]), again limited to patients undergoing nonvascular surgery.
Conclusions and Relevance Among propensity-matched patients undergoing noncardiac, nonvascular surgery, perioperative -blocker exposure was associated with lower
rates of 30-day all-cause mortality in patients with 2 or more Revised Cardiac Risk Index
factors. Our findings support use of a cumulative number of Revised Cardiac Risk Index
predictors in decision making regarding institution and continuation of perioperative -blockade. A multicenter randomized trial involving patients at a low to intermediate risk by
these factors would be of interest to validate these observational findings.
www.jama.com
JAMA. 0;0(16):1704-1713
Author Affiliations: Department of Anesthesia and Perioperative Care, US Department of Veterans Affairs
Medical Center and University of California, San Francisco (Dr London); Center for Medication Safety, Pharmacy Benefits Management Services, US Department
of Veterans Affairs Medical Center, Hines, Illinois
(Dr Hur); Cardiology Section, US Department of Veterans Affairs Medical Center and University of Colorado,
JAMA, April 24, 2013—Vol 309, No. 16
Corrected on April 23, 2013
Downloaded From: http://jama.jamanetwork.com/ on 06/05/2014
Denver (Dr Schwartz); Health Outcomes Program and
Department of Biostatistics & Informatics, Colorado
School of Public Health, Aurora (Dr Henderson).
Corresponding Author: Martin J. London, MD, Department of Anesthesia and Perioperative Care, San
Francisco VA Medical Center, Anesthesia (129), 4150
Clement St, San Francisco, CA 94121 (londonm
@anesthesia.ucsf.edu).
©2013 American Medical Association. All rights reserved.
PERIOPERATIVE -BLOCKADE AND MORTALITY POSTSURGERY
ciated with no difference or a higher rate
of mortality. However, this analysis was
limited by inability to account for outpatient medication use, the type of
-blocker, and uncertainty regarding
the date of surgery and has not been
corroborated in another large clinical
data set.
Recent evidence suggests that use of
perioperative -blockade may be declining.5 Contributing factors may include uncertainty about safety and recent data questioning the efficacy of
long-term  blockade in stable outpatients.6,7 Thus, additional multicenter
analyses of associations of perioperative -blockade with outcome are
timely and potentially relevant to clinicians and regulatory agencies promoting perioperative quality and safety
efforts.
Using system-wide databases in the
Veterans Health Administration (VHA),
we conducted a propensity-matched
analysis using a robust set of clinical
predictor, process, medication, and outcome variables to model the association of perioperative -blockade with
all-cause 30-day mortality and cardiac
morbidity in a contemporary cohort of
patients undergoing major noncardiac surgery.
METHODS
This study was approved by the VHA’s
Office of Patient Care Services and all
responsible institutional review boards
with waiver of informed consent. Race/
ethnicity was coded to be white, black,
or other using patient self-reported data
obtained from the VA Surgical Quality Improvement Program (VASQIP).
Perioperative risk, process and outcome data from patients undergoing
noncardiac surgical procedures in 7 surgical subspecialties (vascular, general,
neurosurgery, orthopedics, thoracic,
urology, and otolaryngology) between October 1, 2005, and September 30, 2010, were obtained from the
VASQIP database. Data collection methods, variable definitions, and interobserver agreement with abstracted chart
data for the VASQIP program have been
reported.8,9
Data were linked with outpatient and
inpatient pharmacy records for -blockers and other commonly prescribed cardiovascular medications captured by the
VHA Pharmacy Benefits ManagementStrategic Healthcare Group (PBMSHG). Since 1998 the PBM-SHG has
maintained a system-wide electronic database of all outpatient prescriptions
filled at VHA pharmacies.10 In 2001, an
inpatient database was instituted.11 We
collected prescription data in 24 VA National Formulary Drug Classes from
both of these databases (eTable 1 available at http://www.jama.com).
We supplemented our data set with
International Classification of Diseases,
Ninth Revision, Clinical Modification discharge and treatment codes extracted
from the VHA Outpatient Care and Patient Treatment Files for inpatient medical admissions administrative databases, within 1 year of each assessed
surgical procedure12 (eTable 2). These
data provided additional risk variables that we considered covariates in
treatment allocation for -blocker
therapy.
Using these databases, we classified
the 6 revised Cardiac Risk Index component variables: high-risk surgery,
cerebrovascular disease, ischemic heart
disease, congestive heart failure,
diabetes mellitus, and renal insufficiency3,4 (eTable 3).
Our primary outcome was all-cause
mortality and the secondary outcome
a composite of Q-wave myocardial infarction (MI) or nonfatal cardiac arrest assessed at 30 days after surgery.
We also categorized the incidence of
new cerebrovascular accident, given its
association with -blocker administration in the Perioperative Ischemic
Evaluation (POISE) study.6
We excluded patients not admitted on
the day of, or hospitalized for the day after surgery (defined as postoperative day
0 and 1) and those dying on either of
those days (landmark analysis). The data
set was truncated at either end to allow
comparable periods of preoperative pharmacy and postoperative outcome analysis. We randomly selected 1 surgical procedure per patient. The resulting cohort
©2013 American Medical Association. All rights reserved.
was then linked with the PBM-SHG and
administrative databases using scrambled
Social Security numbers. We imputed
missing values for preoperative laboratory values and body mass index using
multiple imputation.13,14 Imputed values were constrained within plausible
ranges. The frequency of missing values for physiologic data ranged from
2.3% to 32.4% (average, 16.9%), whereas
for the process variables, it was negligible (1-4 patients). Serum creatinine
concentration (missing in 3% of patients) was not imputed (eTable 3). We
eliminated 193 patients (0.14%) from the
propensity matching process with missing categorical variables used in the regression model (described below).
-Blocker exposure from the inpatient pharmacy database was defined as
any prescription ordered on either postoperative day 0 or 1. Intraoperative or
nonelectronically ordered medications are not captured by PBM-SHG and
therefore were not considered. Dose and
duration of therapy are not currently
approved for research use from the inpatient database.
We extracted prescriptions from the
outpatient pharmacy database within 90
days of hospital admission, coding indicator variables for availability of medication at several periods (90, 60, 30, and
7 days preoperatively). The proportion of days covered by -blocker prescription (in the 90-day preoperative
window), was used in supplementary
analyses.15 We made no attempt to categorize users a priori as acute or longterm given the lack of data on the
indications for the prescription.
-Blockers were coded into the following categories: atenolol, carvedilol,
metoprolol tartrate, metoprolol succinate, and others. Combination antihypertensives were coded by the -blocker
component. Similar methods were used
for drugs ordered after the 2-day exposure period until the time of hospital discharge for descriptive analyses.
Statistical Analysis
To control for treatment-selection bias,
we performed a propensity-score
matched analysis.16 To avoid immorJAMA, April 24, 2013—Vol 309, No. 16 1705
Corrected on April 23, 2013
Downloaded From: http://jama.jamanetwork.com/ on 06/05/2014
PERIOPERATIVE -BLOCKADE AND MORTALITY POSTSURGERY
tal time bias, we performed a landmark analysis, eliminating patients who
died or sustained 1 of the composite
morbidity outcomes during the exposure period.17 A propensity score was
estimated using a nonparsimonious logistic regression model (omitting any
preoperative -blocker use variables;
eTable 4 available at http://www.jama
.com). To adjust for possible regional
differences in -blocker usage, we included a dummy variable for each of the
VHA’s 21 geographical regions in which
the surgery was performed. -Blocker
exposure was regressed on risk or process variables that we considered related to -blocker exposure or outcome with a prevalence in the data set
of at least 1% (eTable 4).
Propensity-score matching (1:1) was
conducted using previously described
methods.18 Pairs of -blocker exposed
and nonexposed patients were matched
using a greedy matching algorithm with
a caliper width of 0.2 standard deviation of the log odds of the estimated
propensity score.19 To accommodate
subanalyses of the type of surgery (vascular vs nonvascular) and estimated cardiac risk (cumulative number of Revised Cardiac Risk Index predictors),
patients were also matched on these
factors. Covariate balance between
matched pairs for continuous and dichotomous categorical variables was assessed using the standardized difference, with values of less than 10%
indicating minimal imbalance.20 The
use of interaction terms between covariates to minimize the standardized
difference was explored iteratively. The
McNemar test was used to compare the
frequency of the primary and secondary outcomes between the matched
groups.21 Relative risks (RRs) were computed using methods appropriate for
paired data and are presented with their
95% CIs.21 Numbers needed to treat
(NNT) were calculated as the inverse
of the absolute risk reduction estimated in the propensity-score matched
sample.
To evaluate associations of longterm and acute -blocker use with outcome, we performed sensitivity analy1706
ses: first, an indicator variable for
outpatient -blocker use within a week
of surgery was included in the propensity-score regression; second, the percent of time covered within the 90day preadmission period and the type
of -blocker were included with appropriate interaction terms. Using our
matched data set, we also compared primary and secondary outcome frequencies between patients with new prescriptions within 7 days or 30 days prior
to surgery relative to those with existing prescriptions in the 60 or 90-day
time periods.
To evaluate associations of the components of the revised Cardiac Risk Index with outcome, we regressed the 6
components, along with the propensity score and -blocker exposure, on
postoperative mortality using the full cohort. Model discrimination and calibration were assessed using the C index and
the Hosmer-Lemeshow goodness-offit statistic, respectively. We then examined mortality rates between exposed
and nonexposed patients using paired
t tests for each of the possible 64 combinations of Revised Cardiac Risk Index strata in the matched cohort.
To evaluate associations of potential
-blocker withdrawal, including differences between the 2 most commonly prescribed -blockers (metoprolol tartrate
or metoprolol succinate vs atenolol), we
categorized potential patterns of drug use
in patients receiving either of these drugs,
considering continuation or withdrawal from outpatient therapy during
the 2-day exposure period. The association of these patterns with our primary
outcome, stratified by vascular vs nonvascular surgery, was evaluated using logistic regression. We also assessed associations between either drug class and the
Revised Cardiac Risk Index predictors.
Continuous and categorical variables were compared using parametric or nonparametric methods as appropriate. The Mantel-Haenszel 2 test
was used to test for trends. All P values were 2-tailed and a value of .05 was
considered significant. SAS software,
version 9.2 (SAS Institute Inc) was used
for the analysis.
JAMA, April 24, 2013—Vol 309, No. 16
Corrected on April 23, 2013
Downloaded From: http://jama.jamanetwork.com/ on 06/05/2014
RESULTS
The initial VASQIP cohort consisted of
334 130 patients. We excluded 197 385
patients following adjustment for surgery on the day of hospital admission
(n = 106 097), length of stay criteria
(n=53 046; including 285 patients dying during the exposure period),
exclusion of multiple surgeries
(n=16 904), truncation of the data set
by the initial 90 and last 30 days
(n = 10 119) and combinations of the
aforementioned (n=11 219). Thus, the
final cohort consisted of 136 745 patients at 104 VHA hospitals. Selected
demographic and clinical characteristics of the study cohort, before and after propensity-score matching, are presented in TABLE 1; all variables used in
the modeling process are presented in
eTable 5.
Analyses of -Blocker Exposure
Overall, 45 347 patients (33.2%) had
an active outpatient prescription for
-blockers within 7 days of surgery
and 55 138 patients (40.3%) were
potentially exposed to -blockers on
either postoperative day 0 or 1. Compared with nonexposed patients,
exposed patients were older and had a
higher burden of cardiovascular and
related comorbidities; 75.4% had significantly greater use of -blockers
during the 90-day preoperative period
(95% CI, 75.0%-75.8%) vs 13.6% of
those who were not exposed (95% CI,
13.4%-13.8; P⬍.001; Table 1 and eTable
5). Of patients exposed on postoperative day 0 or 1, 66.1% had an active prescription covering the week before surgery, whereas only 2.4% of patients had
a new prescription issued in that period (TABLE 2). Inpatient -blocker exposure was higher in the 66.7% of 13 863
patients who underwent vascular surgery (95% CI, 65.9%-67.5%) than in the
37.4% of 122 882 patients who underwent nonvascular surgery (95% CI,
37.1%-37.6%; P⬍.001). The rate of use
increased with increasing Revised Cardiac Risk Index variables: 25.3% for no
factors (95% CI, 24.9%-25.6%) vs 71.3%
for 4 or more factors (95% CI, 69.5%73.2%; P⬍.001; eFigure 1A). Over the
©2013 American Medical Association. All rights reserved.
PERIOPERATIVE -BLOCKADE AND MORTALITY POSTSURGERY
5 years studied, there was a modest, but
significant, trend toward lower -blocker
exposure: 43.5% (95% CI, 42.8%44.2%) during fiscal-year 2006 and
36.2% (95% CI, 35.7%-36.8%) during
fiscal year 2010 (P⬍.001; eFigure 1B).
Metoprolol tartrate was the most commonly prescribed preoperative outpatient -blocker (37.0% of exposed patients) followed by atenolol (26.9% of
exposed patients). Metoprolol tartrate
was the most commonly ordered inpa-
tient -blocker (62.5% of oral prescriptions, 67.2% of intravenous prescriptions) during the exposure period,
followed by atenolol (24.4% of oral
prescriptions, 0.2% of intravenous
prescriptions; Table 2).
Table 1. Selected Study Cohort Characteristics a
Matched Cohort
Full Cohort
Percentage of Patients
Variables
Age, mean (SD), y
Race
White
Sex
Men
Body mass index, mean (SD) b
Preoperative risk variables
ASA physical status classification
I
II
III
IV
V
Revised Cardiac Risk Index variables
Congestive heart failure
Cerebrovascular disease
Diabetes (insulin)
Diabetes (insulin or oral)
Ischemic heart disease
High-risk surgery
Renal insufficiency
Laboratory measurements, mean (SD)
Serum creatinine, mg/dL
Hematocrit, %
White blood cell count, ⫻103/L
Surgical details
Surgery specialty
General
Neurosurgery
Orthopedic
Otolaryngology
Thoracic
Urology
Vascular
Emergency procedure
Laparoscopic procedure
Endovascular procedure
Duration of surgery, mean (SD), h
Principal anesthesia technique
General
Spinal/epidural alone
Other
All
(n = 136 745)
64.4 (10.2)
Exposed
(n = 55 138)
65.3 (9.9)
Not Exposed
(n = 81 607)
61.3 (11.5)
Percentage of Patients
P
Value
⬍.001
All
(n = 75 610)
62.9 (11.1)
Exposed
(n = 37 805)
64.4 (10.0)
Not Exposed
(n = 37 805)
64.4 (10.4)
P
Value
.60
66.4
67.5
65.1
⬍.001
66.1
66.5
66.3
96.3
29.3 (5.7)
96.9
29.3 (5.7)
94.1
28.8 (5.5)
⬍.001
⬍.001
95.3
29.0 (5.6)
96.3
29.3 (5.6)
96.3
29.2 (5.7)
0.1
16.6
0.1
12.5
1.3
29.8
0.8
22.8
0.2
16.8
0.1
16.4
74.4
8.7
0.1
75.7
11.6
0.1
63.5
5.3
0.1
⬍.001
68.4
7.8
0.1
74.0
8.9
0.1
74.8
8.6
0.1
.07
9.8
10.0
10.4
27.5
28.0
40.4
3.2
15.2
12.2
12.5
30.7
42.9
40.9
4.2
5.3
6.6
6.5
19.1
14.7
35.9
1.9
⬍.001
⬍.001
⬍.001
⬍.001
⬍.001
⬍.001
⬍.001
9.3
8.8
8.9
23.8
26.1
37.9
2.8
10.2
10.2
10.3
27.5
28.2
39.5
3.3
9.4
9.9
10.4
27.5
27.7
41.2
3.1
⬍.001
.2
.7
.99
.16
⬍.001
.11
1.2 (0.8)
41.0 (8.8)
1.2 (0.8)
40.8 (4.9)
1.1 (0.6)
41.5 (4.6)
⬍.001
⬍.001
1.1 (0.7)
41.2 (4.7)
1.2 (0.8)
41.0 (8.8)
1.2 (0.8)
41.0 (8.8)
⬍.001
.74
7.9 (3.9)
8.0 (3.6)
7.8 (3.8)
⬍.001
7.9 (3.7)
7.9 (3.5)
8.0 (4.3)
.6
.27
.92
0.09
25.0
9.3
30.5
26.1
8.8
29.3
27.0
8.4
28.1
⬍.001
4.1
5.9
15.0
10.1
4.0
6.8
14.4
10.6
4.0
7.0
14.8
10.6
.002
6.6
10.1
0.8
2.73 (1.7)
.006
⬍.001
⬍.001
⬍.001
6.4
10.4
1.5
2.8 (1.7)
6.3
10.6
1.5
2.8 (1.7)
6.5
11.0
1.5
2.8 (1.7)
.5
.04
.76
.74
88.9
9.3
1.8
⬍.001
89.1
9.0
1.9
89.0
9.0
1.9
89.4
8.7
1.9
.28
26.6
8.6
28.7
26.1
7.9
25.9
24.3
10.2
33.5
4.0
6.9
14.6
10.6
3.6
7.2
12.5
16.8
4.5
5.1
16.7
5.7
6.4
10.8
1.5
2.8 (1.7)
6.2
10.7
2.6
2.89 (1.7)
89.2
8.9
1.9
89.3
8.6
2.1
Abbreviations: ASA, American Society of Anesthesiologists.
SI conversion factors: To convert creatinine from mg/dL to mol/L, multiply by 88.4.
a A complete list of variables is available in eTable 5 (http://www.jama.com).
b Body mass index is calculated as weight in kilograms divided by height in meters squared.
©2013 American Medical Association. All rights reserved.
JAMA, April 24, 2013—Vol 309, No. 16 1707
Corrected on April 23, 2013
Downloaded From: http://jama.jamanetwork.com/ on 06/05/2014
PERIOPERATIVE -BLOCKADE AND MORTALITY POSTSURGERY
Table 2. Medication Data
Matched Cohort
Full Cohort
Percentage of Patients
All
Exposed Not Exposed
Variables
(n = 136 745) (n = 55 138) (n = 81 607)
Preoperative medications
ACE-I/ARB
43.1
54.7
35.3
Diuretic
43.1
54.4
35.4
CEB-dihydropyridine
19.5
24.9
15.9
CEB-nondihydropyridine
6.6
7.3
6.2
Clonidine
3.5
4.8
2.6
Other antihypertensive
7.2
11.9
4.0
Anticoagulant/antiplatelet
75.7
84.3
69.9
Antilipemic agent
53.9
67.2
45.0
Digoxin
5.0
7.5
3.2
Oral hypoglycemic
18.9
24.2
15.3
Rosiglitazone
1.6
2.2
1.2
Insulin
16.4
22.8
12.0
Bronchodilator
23.7
28.0
20.8
-Blocker usage outpatients parameters
90 d prior
38.5
75.4
13.6
7 d prior
33.2
66.1
10.9
New within 7 d prior
1.2
2.4
0.4
Type -blocker outpatient within 90 d prior
Atenolol
14.1
26.9
5.4
Metoprolol tartrate
18.5
37.0
6.1
Metoprolol succinate
2.5
5.0
0.8
Carvedilol
1.6
3.1
0.6
Other
1.8
3.5
0.7
No use
61.5
24.6
86.5
-Blocker use day of surgery
33.7
83.6
0
Inpatient type -blocker exposure period, unit dose
Atenolol
24.4
24.4
0.0
Metoprolol tartrate
62.5
62.5
0.0
Metoprolol succinate
4.1
4.1
0.0
Carvedilol
3.0
3.0
0.0
Other
6.0
6.0
0.0
Inpatient type -blocker exposure period, intravenous dose
Atenolol
0.2
0.2
0.0
Metoprolol tartrate
67.2
67.2
0.0
Other
32.6
32.6
0.0
Inpatient -blocker use prior to discharge
21.3
36.3
11.2
Inpatient type -blocker prior to discharge
Atenolol
3.5
6.4
1.5
Metoprolol tartrate
15.4
25.7
8.5
Metoprolol succinate
0.8
1.5
0.3
Carvedilol
0.6
1.1
0.3
Other
1.0
1.6
0.6
No additional prescriptions
78.7
63.7
88.8
Postdischarge use, 30 d
75.3
39.3
14.9
Postdischarge type -blocker, 30 d
Atenolol
3.5
25.4
4.9
Metoprolol tartrate
20.6
39.0
8.1
Metoprolol succinate
2.3
4.7
0.7
Carvedilol
1.5
2.9
0.6
Other
1.7
3.3
0.6
No use
60.7
24.7
85.1
Percentage of Patients
P
All
Exposed Not Exposed P
Value (n = 75 610) (n = 37 805) (n = 37 805) Value
⬍.001
⬍.001
⬍.001
⬍.001
⬍.001
⬍.001
⬍.001
⬍.001
⬍.001
⬍.001
⬍.001
⬍.001
⬍.001
49.6
51.1
23.2
7.7
4.2
7.9
80.3
59.6
5.7
21.9
1.9
19.1
25.8
49.5
51.2
23.3
7.6
4.1
8.0
80.3
59.6
5.8
21.9
1.9
19.9
25.9
49.6
51.0
23.1
7.8
4.2
7.5
80.3
59.5
5.6
21.9
1.8
18.3
25.7
.91
.64
.61
.41
.96
.01
.98
.66
.13
.91
.31
⬍.001
.47
⬍.001
⬍.001
⬍.001
46.9
40.3
1.6
71.8
62.8
2.5
22.0
17.8
0.6
⬍.001
⬍.001
⬍.001
18.2
21.9
2.7
1.7
2.4
53.1
41.5
28.3
33.4
3.9
2.2
4.0
28.2
83.0
8.1
10.5
1.4
1.1
0.9
78.0
0.0
26.9
60.7
3.4
2.3
6.7
26.9
60.7
3.4
2.3
6.7
0.0
0.0
0.0
0.0
0.0
0.3
72.6
27.1
25.8
0.3
72.6
27.1
33.5
0.0
0.0
0.0
18.2
4.4
18.6
0.8
0.7
1.3
74.2
48.0
6.3
23.6
1.1
0.8
1.6
66.5
72.6
2.5
13.6
0.5
0.6
0.9
81.8
23.3
17.0
24.6
2.5
1.6
2.2
52.0
26.8
36.3
2.7
2.1
3.7
76.7
7.2
12.9
1.3
1.1
0.8
27.4
⬍.001
⬍.001
⬍.001
⬍.001
⬍.001
⬍.001
⬍.001
⬍.001
⬍.001
⬍.001
⬍.001
⬍.001
⬍.001
⬍.001
⬍.001
⬍.001
Abbreviations: ACE-I, angiotensin converting enzyme inhibitor; ARB, angiotensin receptor blocker; ASA, American Society of Anesthesiologists; CEB, calcium entry blocker.
1708
JAMA, April 24, 2013—Vol 309, No. 16
Corrected on April 23, 2013
Downloaded From: http://jama.jamanetwork.com/ on 06/05/2014
©2013 American Medical Association. All rights reserved.
PERIOPERATIVE -BLOCKADE AND MORTALITY POSTSURGERY
Table 3. Postoperative Outcomes
Matched Cohort
Full Cohort
Percentage of Patients
Variables
30-d All-cause mortality
Cardiac complications
Cardiac arrest
Q-wave myocardial infarction
Composite cardiac complication
Cerebrovascular accident
Total surgical LOS, median (IQR), d
Total hospital LOS, median (IQR), d
Percentage of Patients
All
(n = 136 745)
1.1
Exposed
(n = 55 138)
1.4
Not Exposed
(n = 81 607)
1.0
P
Value
⬍.001
All
(n = 75 610)
1.3
Exposed
(n = 37 805)
1.1
Not Exposed
(n = 37 805)
1.5
P
Value
⬍.001
0.6
0.3
0.9
0.3
4 (3-7)
0.8
0.5
1.2
0.4
4 (3-7)
0.4
0.3
0.7
0.2
4 (3-6)
⬍.001
⬍.001
⬍.001
⬍.001
⬍.001
0.7
0.4
1.0
0.4
4 (3-7)
0.6
0.3
0.8
0.4
4 (3-7)
0.7
0.5
1.2
0.3
4 (3-7)
.01
⬍.001
⬍.001
.45
0.25
4 (3-7)
5 (3-7)
4 (3-7)
⬍.001
4 (3-7)
4 (3-7)
4 (3-7)
0.80
Abbreviation: LOS, length of stay.
Primary and Secondary
Outcomes
Overall, 1568 patients (1.1%) sustained the primary 30-day mortality
outcome and 1196 patients (0.9%) the
secondary cardiac morbidity outcome. Unadjusted primary outcomes
occurred in 1.4 % (95% CI, 1.3%1.5%) of exposed patients vs 1.0% (95%
CI, 0.9%-1.1%) of unexposed patients. Primary and secondary outcomes occurred more frequently in patients exposed to -blockers (mortality
in those exposed, 1.4% [95% CI, 1.3%1.5%] vs those unexposed, 1.0% [95%
CI, 0.9%-1.1%], cardiac morbidity of
those exposed, 1.2% [95% CI, 1.1%1.3%] vs those unexposed, 0.7% [95%
CI, 0.6%-0.7%]; P ⬍.001 for both) and
occurred more frequently in those exposed who underwent vascular surgery than those who underwent nonvascular surgery (vascular surgery
mortality, 1.6% [95% CI, 1.4%-1.8%]
vs nonvascular surgery, 1.1% [95% CI,
1.0%-1.2%]; vascular surgery cardiac
morbidity, 1.6% [95% CI, 1.4%-1.8%]
vs nonvascular surgery cardiac morbidity, 0.8% [95% CI, 0.7%-0.8%]; P ⬍.001
for both); and occurred more frequently in patients with increasing number of Revised Cardiac Index Risk predictors (TABLE 3 and eFigure 2A and B).
Patients sustaining a secondary outcome were at markedly elevated risk of
mortality compared with those who did
not (571 deaths [47.7%] vs 997 deaths
[0.7%]; odds ratio [OR], 123 [95% CI,
108-140]; P ⬍ .001). Stratification by
-blocker exposure revealed that exposed patients had a slightly lower, but
still markedly elevated, risk of mortality following a secondary outcome (OR,
93 [95% CI, 78-112] vs OR, 161 [95%
CI, 133-195]; P ⬍.001 for both), with
a similar pattern for patients undergoing vascular surgery or when analyzed
by cumulative Revised Cardiac Risk Index factors.
Following 1:1 propensity matching,
we obtained 37 805 matched pairs for the
primary mortality model, a match rate
of 68.5% for exposed patients. Following exclusion of an additional 317 patients from the original cohort who had
sustained a secondary outcome during
the exposure period and rematching, we
obtained 37 662 matched pairs for the
secondary cardiac morbidity analysis.
The distribution of covariates, -blocker
usage parameters and outcomes between matched pairs in the primary outcome analysis are presented in Table 1
and eTable 5. The groups were well balanced with standardized differences of
less than 10% for all continuous and dichotomous categorical variables (eTable
6 available at www.jama.com).
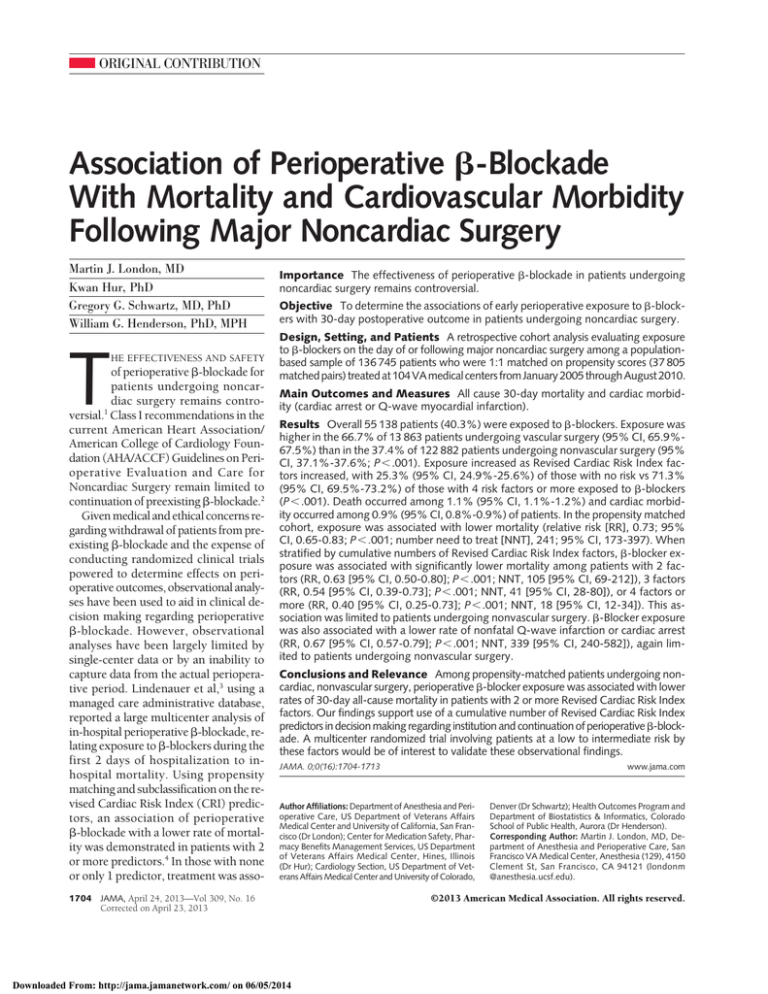
In the matched cohort, a lower rate
of mortality was observed in the
exposed group (relative risk [RR],
0.73 [95% CI, 0.65-0.83]; P ⬍ .001;
NNT, 241 [95% CI, 173-397];
FIGURE 1A and eTable 7). Stratification by revised Cardiac Risk Index variables revealed a lack of association with
none or 1 revised Cardiac Risk Index
factor. However, significant associa-
©2013 American Medical Association. All rights reserved.
tions of -blocker exposure with lower
mortality were noted in patients with
2 Revised Cardiac Risk Index factors
(RR, 0.63 [95% CI, 0.50-0.80]; P⬍.001;
NNT, 105 [95% CI, 69-212], 3 factors
(RR, 0.54 [95% CI, 0.39-0.73]; P⬍.001;
NNT , 41 [95% CI, 28-80]), or 4 factors or more (RR, 0.40 [95% CI, 0.250.73]; P⬍.001; NNT , 18 [95% CI, 1234]. When stratified by type of surgery,
no significant associations were noted
in patients undergoing vascular surgery, regardless of the Revised Cardiac Risk Index strata (Figure 1B and
eTable 7). The distribution of study covariates between the matched patients
in the risk strata with significant associations (eg, 2 or more Revised Cardiac Risk Index factors) revealed similar balance as in the overall cohort,
albeit at a higher preoperative risk profile than in those patients with fewer
than 2 risk factors (eTable 8).
Considering the secondary cardiac
morbidity outcome, -blocker exposure was associated with a significantly lower rate of cardiac complications (RR, 0.67 [95% CI, 0.57-0.79];
P ⬍ .001; NNT, 339 [95% CI, 240582]; FIGURE 2A and eTable 9). Stratified by Revised Cardiac Risk Index
factors, significant associations of
-blocker exposure to rates of cardiac
complications were noted in patients
with 2 or 3 Revised Cardiac Risk
Index factors only (Figure 2A and
eTable 9). In the vascular surgery subgroup, no significant associations were
present (Figure 2B and eTable 9).
JAMA, April 24, 2013—Vol 309, No. 16 1709
Corrected on April 23, 2013
Downloaded From: http://jama.jamanetwork.com/ on 06/05/2014
PERIOPERATIVE -BLOCKADE AND MORTALITY POSTSURGERY
Substitution of the secondary Revised Cardiac Risk Index definition for
diabetes based on treatment with oral
hypoglycemic medications, insulin, or
both (eTable 3) significantly increased the number of patients coded
Figure 1. Thirty-Day Mortality Propensity Model
A All surgery
No. of Deaths
No. of Patients
All Patients
No. of Revised Cardiac
Risk Index predictors
0
1
2
3
>4
Exposed
37 805
Not Exposed
37 805
Exposed
426
Not Exposed
583
12 250
16 057
6795
2090
613
12 250
16 057
6795
2090
613
67
166
111
59
23
53
186
176
110
58
Favors
Exposure
Favors
Nonexposure
Sensitivity and Exploratory
Medication Analyses
0.2
5
1.0
Relative Risk (95% CI)
B Vascular surgery
No. of Patients
All Patients
No. of Revised Cardiac
Risk Index predictors
0
1
2
3
>4
No. of Deaths
Exposed
3999
Not Exposed
3999
Exposed
55
Not Exposed
62
857
1593
1033
403
113
857
1593
1033
403
113
5
20
11
13
6
6
21
18
12
5
Favors
Exposure
0.2
Favors
Nonexposure
5
1.0
Relative Risk (95% CI)
Figure 2.Thirty-Day Cardiac Morbidity Propensity Model
A All surgery
No. of Deaths
No. of Patients
All Patients
No. of Revised Cardiac
Risk Index predictors
0
1
2
3
>4
Exposed
37 662
Not Exposed
37 662
Exposed
225
Not Exposed
336
12 228
16 004
6761
2063
606
12 228
16 004
6761
2063
606
23
83
63
36
20
35
104
105
59
33
Favors
Exposure
0.2
Favors
Nonexposure
1.0
5
Relative Risk (95% CI)
B Vascular surgery
No. of Patients
All Patients
No. of Revised Cardiac
Risk Index predictors
0
1
2
3
>4
No. of Deaths
Exposed
3973
Not Exposed
3973
Exposed
34
Not Exposed
49
852
1590
1024
395
112
852
1590
1024
395
112
0
5
15
9
5
4
14
13
11
7
Favors
Exposure
0.2
Favors
Nonexposure
5
1.0
Relative Risk (95% CI)
1710
JAMA, April 24, 2013—Vol 309, No. 16
Corrected on April 23, 2013
Downloaded From: http://jama.jamanetwork.com/ on 06/05/2014
as having diabetes (23.7% [95% CI,
23.5%-24.0%]) relative to those with
diabetes (8.9% [95% CI, 8.7%-9.0%];
P ⬍.001) base on the primary definition. However, it resulted in a similar
match rate in the propensity model
(37 856 matched pairs) with no differences within any of the strata from the
model using the primary definition
(eTables 10 and 11).
Sensitivity analyses incorporating prehospital admission -blocker use in the
propensity model did not alter the results for mortality (eTables 12-14). Post
hoc comparisons of the primary and
secondary outcomes between patients
classified as either acute or chronic users again revealed results consistent
with the primary analysis (eTable 15).
Based on absence of reordering of an
outpatient preoperative prescription
during the exposure period, we detected 8911 patients (6.5%) of the
136 745 patients who had potentially
withdrawn from -blockers. These patients were noted to be at higher risk
of mortality than the 36 436 patients
who continued treatment (OR, 1.60
[95% CI, 1.34-1.91]; P ⬍ .001) and
higher than the 72 696 patients with no
prior preoperative use or exposure (OR,
2.30 [95% CI, 1.93-2.70]; P ⬍ .001).
However, when compared with 18 702
patients who were exposed to treatment with no prior use, no significant
difference was noted (OR, 1.15 [95%
CI 0.95-1.38]; P=.15).
Comparisons of mortality among patients receiving metoprolol (tartrate or
succinate) vs atenolol prior to surgery
and the effects of their withdrawal are
presented in eTable 16. Mortality was
significantly lower in the atenolol group
(treated or withdrawn) than in the
metoprolol group. However, similar
ORs for mortality were noted for either
drug in patients who stopped taking
-blockers. Patients in whom inpatient metoprolol was substituted for
atenolol during the exposure period had
a stronger association with mortality
relative to the opposite pattern. How-
©2013 American Medical Association. All rights reserved.
PERIOPERATIVE -BLOCKADE AND MORTALITY POSTSURGERY
ever, the number of patients in the latter group was trivial (16-36 patients).
Associations of withdrawal of metoprolol in patients who had undergone
vascular surgery was similar (OR, 1.66
[95% CI, 1.01-2.73]; P ⬍ .05), although of lesser significance than patients who did not (OR, 1.78 [95% CI,
1.41-2.23]; P ⬍ .001). We were unable to detect a significant association
of atenolol withdrawal (OR 1.34 [95%
CI, 0.60-3.03]; P⬍.47) among the 1884
patients who had undergone vascular
surgery compared with the 14 420 who
had not (OR, 2.19 [95% CI, 1.503.19]; P⬍.001), possibly due to lower
sample size.
The distribution of the components
of the Revised Cardiac Risk Index for
the full and matched cohorts, are presented in Table 1. Their combinations
and the corresponding associated mortality rates are presented in eTable 17
(available at http://www.jama.com).
Pairwise comparisons of mortality rates
in each of the possible 64 combinations of the cumulative Revised Cardiac Risk Index predictors revealed only
7 significant combinations. Given the
multiple comparisons involved, none
of these would be considered significant (using a threshold of P⬍.001). Logistic regression models for mortality
incorporating the Revised Cardiac Risk
Index factors, adjusted for propensity
score and -blocker exposure, using
either the entire or matched cohort, revealed similar ORs for each Revised
Cardiac Risk Index component (eTable
18). Stratification of metoprolol or atenolol patients by the cerebrovascular,
congestive heart failure, and ischemic
heart disease components revealed significantly stronger associations of metoprolol over atenolol with each of these
components (eTable 19).
Relations With Postoperative Stroke
In unadjusted analyses, postoperative
stroke occurred in 415 patients (0.3%;
Table 3). Incidence of stroke was significantly higher in patients who were
exposed to -blockers (0.45% [95% CI,
0.39%-0.50%]) than those who were not
(0.21% [95% CI, 0.17%-0.24%];
P⬍.001). However, the overall stroke
incidence among the full cohort did not
differ significantly by exposure in the
matched cohort (exposed, 0.35% [95%
CI, 0.29%-0.41%] vs unexposed, 0.32%
[95% CI, 0.26%-0.38%]; P = .45), nor
among patients with the strongest association of exposure with outcome
(those with a Revised Cardiac Risk Index score ⱖ 2; exposed vs unexposed,
0.6%; P=.70; eTable 8). Although patients who had undergone vascular surgery had a higher incidence of stroke
(1.05%; 95% CI, 0.88%-1.22%) than did
patients who had not (0.22% [95% CI,
0.19%-0.25%]; P⬍.001), there were no
significant differences in stroke incidence noted between patients exposed
(1.0% [95% CI, 0.70%-1.32%]) vs those
unexposed (1.1% [95% CI, 0.79%1.44%]; P=.74) or among matched patients who had undergone vascular surgery (0.28% [95% CI, 0.22%-0.33%]) or
those who had not (0.22% [95% CI,
0.17%-0.28%]; P=.22) of the matched
cohort. We noted significant associations of drug group with stroke (atenolol vs metoprolol, OR, 0.63 [95% CI,
0.45-0.89]; P=.008; eTable 20).
DISCUSSION
We report associations of early perioperative -blocker exposure with
30-day all-cause mortality and cardiac
morbidity in patients undergoing
noncardiac surgery in the VHA health
care system. Our analyses suggest that
such exposure is significantly associated with a lower rate of all-cause mortality, with the strongest association in
those undergoing nonvascular surgery and in those with 2 or more Revised Cardiac Risk Index factors. We
also noted a significant association with
a lower rate of cardiac arrest and
Q-wave MI. Although the latter complications occurred infrequently, they
are highly predictive of subsequent
mortality. 22,23 The incidence of Qwave MI in the current analysis is lower
than the risk of MI reported in other
studies in which elevation of cardiac
biomarkers or less specific electrocardiographic patterns were used to define perioperative MI.24,25
©2013 American Medical Association. All rights reserved.
We were unable to detect significant associations between -blocker exposure and outcome in patients undergoing vascular surgery. Although
considered at greatest risk of cardiovascular complications, prior analyses
in this population have reported variable associations. 1,26,27 However, a
smaller sample size relative to the nonvascular cohort and the possibility that
these patients received medication not
captured by PBM-SHG (eg, those administered intraoperatively or ordered nonelectronically) or received a
higher level of care (eg, ICU utilization), a factor not captured by VASQIP,
must be considered.
The rate of -blocker exposure over
the period of this analysis significantly declined from 43.5% to 36.2%.
This may be related to the findings of
the POISE trial of increased stroke and
death in treated patients, leading to
more conservative guideline recommendations within this period.2,6 Similar findings have been recently reported by Canadian investigators during
this timeframe.5
We were unable to demonstrate significant differences between our post hoc
definitions of long-term use or acute institution of -blockade. Limited evidence suggests that long-term use of
-blockade is associated with lower rates
of adverse outcome than institution
within 1 week of or immediately after
surgery.28,29 Our data suggest that institution of -blockade within 30 days is
associated with similar outcome rates as
longer periods. However, our analysis of
associations within 7 days of surgery is
limited by the very low incidence observed (2.4%).
We noted associations of increased
rates of mortality with -blocker withdrawal in the exposure period. This association, corresponding to approximately 2-fold increased risk, is similar to
that reported by other investigators.30-32
Controversy exists over the efficacy
and safety of specific -blockers used
for perioperative -blockade. Agents
with greater -1 specificity (eg, atenolol or bisoprolol) have been associated with improved outcome relative to
JAMA, April 24, 2013—Vol 309, No. 16 1711
Corrected on April 23, 2013
Downloaded From: http://jama.jamanetwork.com/ on 06/05/2014
PERIOPERATIVE -BLOCKADE AND MORTALITY POSTSURGERY
more widely used formulations of metoprolol.33 Our exploratory analyses suggest stronger associations with mortality among patients treated with
metoprolol than with atenolol. However, we also found that patients taking metoprolol were significantly more
likely to have ischemic heart disease or
congestive heart failure, consistent with
existing AHA/ACCF guideline indications for therapy.34,35
Similartootherinvestigators,wenoted
significant interaction of perioperative
-blockade and the number of Revised
CardiacRiskIndexpredictorsonoutcome
rates, with the difference in event rates
between patients who were exposed and
those were not exposed, being most
prominent among patients with the largest number of Revised Cardiac Risk Index predictors.3,32 However, we were not
able to demonstrate significant interaction of perioperative -blockade with any
specific combination of these variables.
We used all 6 revised Cardiac Risk Index
predictors, including history of congestive heart failure, a major risk factor for
perioperative mortality.36 Although decompensated heart failure remains an absolute contraindication to perioperative
-blockade, long-term use for compensated heart failure has a class I indication
for therapy and therefore continuation
in the perioperative period.2,34
We were unable to demonstrate significant associations of perioperative
-blockade with the risk of postoperative stroke. This contrasts with an increased risk observed in the POISE
trial.6 Our overall incidence (0.3%) was
lower than that of the highly selected
patients enrolled in that trial (0.7%). Although the overall stroke rates in our
vascular cohort are similar to the treated
patients in POISE (1% in both), no differences between our exposed and unexposed patients were noted. Analysis
of existing randomized trials suggests
that either timing of initiation and or
dose of -blocker are important covariates.37 Our data capture did not allow
us to address dose parameters. Our finding of a higher incidence of stroke in
patients treated with metoprolol may
be related to the fact that metoprolol
1712
users had a significantly higher incidence of preexisting cerebrovascular
disease relative to atenolol users, potentially predisposing them to perioperative injury.38
In conclusion, our results suggest
that early perioperative -blocker exposure is associated with significantly
lower rates of 30-day mortality and cardiac morbidity in patients at elevated
baseline cardiac risk undergoing nonvascular surgery. Although assessment of cumulative number of Revised Cardiac Risk Index predictors
might be helpful to clinicians in deciding whether to use perioperative
-blockade, the current findings highlight a need for a randomized multicenter trial of perioperative -blockade in low- to intermediate-risk patients
scheduled for noncardiac surgery.
Author Contributions: Dr London had full access to
all of the data in the study and takes responsibility for
the integrity of the data and the accuracy of the data
analysis.
Study concept and design: All authors.
Acquisition of data: London, Henderson.
Analysis and interpretation of the data: All authors.
Drafting of the manuscript: London.
Critical revision of the manuscript for important intellectual content: All authors.
Statistical analysis: London, Hur, Henderson.
Obtained funding: London.
Administrative, technical or material support: London.
Study Supervision: London.
Conflict of Interest Disclosures: All authors have completed and submitted the ICMJE Form for Disclosure
of Potential Conflicts of Interest. Dr Schwartz reported that institutional grants are pending from Roche,
Resverlogix, Anthera, and Sanofi. Dr London reported receiving an unrestricted grant from the Anesthesia Patient Safety Foundation. No other conflicts of interest were reported.
Funding/Support: This study was supported by a grant
from the Anesthesia Patient Safety Foundation.
Role of the Sponsor: The Anesthesia Patient Safety Foundation had no role in the design and conduct of the study,
in the collection, management, analysis and data interpretation, or in the preparation, review or approval of
the manuscript. The VASQIP database was provided by
VASQIP who collected the data and reviewed and approved the manuscript prior to submission.
Disclaimer: The opinions expressed are those of the
authors and not necessarily those of the Department
of Veterans Affairs or the United States Government.
Online-Only Material: The 20 eTables and 2 eFigures are available at http://www.jama.com.
Additional Contributions: We thank Francesca
Cunningham, PharmD, Director of the Department of
Veterans Affairs Center for Medication Safety (VAMedSAFE) and Program Manager for Pharmacoepidemiologic and Outcomes Research for VHA-PBM who provided constructive input throughout the design and
conduct of this analysis. Dr Cunningham received no
financial compensation from this project. We also thank
the VA Surgical Quality Data Use Group (SQDUG) for
its role as scientific advisors and for the critical review
of data use and analysis presented in this article.
JAMA, April 24, 2013—Vol 309, No. 16
Corrected on April 23, 2013
Downloaded From: http://jama.jamanetwork.com/ on 06/05/2014
REFERENCES
1. Bangalore S, Wetterslev J, Pranesh S, Sawhney S,
Gluud C, Messerli FH. Perioperative beta blockers in
patients having non-cardiac surgery: a meta-analysis.
Lancet. 2008;372(9654):1962-1976.
2. Fleisher LA, Beckman JA, Brown KA, et al. 2009
ACCF/AHA focused update on perioperative beta
blockade incorporated into the ACC/AHA 2007 guidelines on perioperative cardiovascular evaluation and
care for noncardiac surgery: a report of the American
college of cardiology foundation/American heart association task force on practice guidelines. Circulation.
2009;120(21):e169-e276.
3. Lindenauer PK, Pekow P, Wang K, Mamidi DK,
Gutierrez B, Benjamin EM. Perioperative betablocker therapy and mortality after major noncardiac
surgery. N Engl J Med. 2005;353(4):349-361.
4. Lee TH, Marcantonio ER, Mangione CM, et al. Derivation and prospective validation of a simple index for
prediction of cardiac risk of major noncardiac surgery.
Circulation. 1999;100(10):1043-1049.
5. Wijeysundera DN, Mamdani M, Laupacis A, et al.
Clinical evidence, practice guidelines, and -blocker
utilization before major noncardiac surgery. Circ Cardiovasc Qual Outcomes. 2012;5(4):558-565.
6. Devereaux PJ, Yang H, Yusuf S, et al; POISE Study
Group. Effects of extended-release metoprolol succinate in patients undergoing non-cardiac surgery (POISE
trial): a randomised controlled trial. Lancet. 2008;
371(9627):1839-1847.
7. Bangalore S, Steg G, Deedwania P, et al; REACH
Registry Investigators. -Blocker use and clinical outcomes in stable outpatients with and without coronary artery disease. JAMA. 2012;308(13):13401349.
8. Khuri SF, Daley J, Henderson W, et al; National VA
Surgical Quality Improvement Program. The Department of Veterans Affairs’ NSQIP: the first national, validated, outcome-based, risk-adjusted, and peercontrolled program for the measurement and
enhancement of the quality of surgical care. Ann Surg.
1998;228(4):491-507.
9. Davis CL, Pierce JR, Henderson W, et al. Assessment of the reliability of data collected for the Department of Veterans Affairs national surgical quality
improvement program. J Am Coll Surg. 2007;204
(4):550-560.
10. Sales MM, Cunningham FE, Glassman PA,
Valentino MA, Good CB. Pharmacy benefits management in the Veterans Health Administration: 1995 to
2003. Am J Manag Care. 2005;11(2):104-112.
11. Smith MW, Joseph GJ. Pharmacy data in the VA
health care system. Med Care Res Rev. 2003;60
(3)(suppl):92S-123S.
12. Maynard C, Chapko MK. Data resources in the
Department of Veterans Affairs. Diabetes Care. 2004;
27(suppl 2):B22-B26.
13. Wu WC, Schifftner TL, Henderson WG, et al. Preoperative hematocrit levels and postoperative outcomes in older patients undergoing noncardiac surgery.
JAMA. 2007;297(22):2481-2488.
14. Hamilton BH, Ko CY, Richards K, Hall BL. Missing data in the American College of Surgeons National Surgical Quality Improvement Program are not
missing at random: implications and potential impact
on quality assessments. J Am Coll Surg. 2010;
210(2):125-139.
15. Steiner JF, Prochazka AV. The assessment of refill compliance using pharmacy records: methods, validity, and applications. J Clin Epidemiol. 1997;
50(1):105-116.
16. Rosenbaum PR, Rubin DB. The central role of the
propensity score in observational studies for causal
effects. Biometrika. 1983;70:41-55.
17. Suissa S. Immortal time bias in pharmacoepidemiology. Am J Epidemiol. 2008;167(4):492499.
18. Austin PC. Propensity-score matching in the car-
©2013 American Medical Association. All rights reserved.
PERIOPERATIVE -BLOCKADE AND MORTALITY POSTSURGERY
diovascular surgery literature from 2004 to 2006: a
systematic review and suggestions for improvement.
J Thorac Cardiovasc Surg. 2007;134(5):1128-1135.
19. Austin PC. Optimal caliper widths for propensityscore matching when estimating differences in means
and differences in proportions in observational studies.
Pharm Stat. 2011;10(2):150-161.
20. Austin PC. Balance diagnostics for comparing the
distribution of baseline covariates between treatment groups in propensity-score matched samples. Stat
Med. 2009;28(25):3083-3107.
21. Agresti A, Min Y. Effects and non-effects of paired
identical observations in comparing proportions with
binary matched-pairs data. Stat Med. 2004;23
(1):65-75.
22. Hamel MB, Henderson WG, Khuri SF, Daley J. Surgical outcomes for patients aged 80 and older: morbidity and mortality from major noncardiac surgery.
J Am Geriatr Soc. 2005;53(3):424-429.
23. Davenport DL, Ferraris VA, Hosokawa P,
Henderson WG, Khuri SF, Mentzer RM Jr. Multivariable predictors of postoperative cardiac adverse events
after general and vascular surgery: results from the patient safety in surgery study. J Am Coll Surg. 2007;
204(6):1199-1210.
24. Levy M, Heels-Ansdell D, Hiralal R, et al. Prognostic value of troponin and creatine kinase muscle
and brain isoenzyme measurement after noncardiac
surgery: a systematic review and meta-analysis.
Anesthesiology. 2011;114(4):796-806.
25. Devereaux PJ, Chan MT, Alonso-Coello P, et al;
Vascular Events In Noncardiac Surgery Patients Cohort Evaluation (VISION) Study Investigators. Association between postoperative troponin levels and 30day mortality among patients undergoing noncardiac
surgery. JAMA. 2012;307(21):2295-2304.
26. Poldermans D, Bax JJ, Schouten O, et al; Dutch
Echocardiographic Cardiac Risk Evaluation Applying
Stress Echo Study Group. Should major vascular surgery be delayed because of preoperative cardiac testing in intermediate-risk patients receiving betablocker therapy with tight heart rate control? J Am
Coll Cardiol. 2006;48(5):964-969.
27. Bertges DJ, Goodney PP, Zhao Y, et al; Vascular
Study Group of New England. The Vascular Study
Group of New England Cardiac Risk Index (VSGCRI) predicts cardiac complications more accurately
than the Revised Cardiac Risk Index in vascular surgery patients. J Vasc Surg. 2010;52(3):674-683, 683,
e1-e683, e3.
28. Flu WJ, van Kuijk JP, Chonchol M, et al. Timing
of pre-operative Beta-blocker treatment in vascular surgery patients: influence on post-operative outcome.
J Am Coll Cardiol. 2010;56(23):1922-1929.
29. Ellenberger C, Tait G, Beattie WS. Chronic  blockade is associated with a better outcome after elective noncardiac surgery than acute  blockade: a
single-center propensity-matched cohort study.
Anesthesiology. 2011;114(4):817-823.
30. van Klei WA, Bryson GL, Yang H, Forster AJ. Effect of beta-blocker prescription on the incidence of
postoperative myocardial infarction after hip and knee
arthroplasty. Anesthesiology. 2009;111(4):717724.
31. Wallace AW, Au S, Cason BA. Association of the
pattern of use of perioperative -blockade and postoperative mortality. Anesthesiology. 2010;113
(4):794-805.
32. Kwon S, Thompson R, Florence M, et al; Surgical
Care and Outcomes Assessment Program (SCOAP)
Collaborative. -Blocker continuation after noncardiac surgery: a report from the surgical care and out-
©2013 American Medical Association. All rights reserved.
comes assessment program. Arch Surg. 2012;147
(5):467-473.
33. Badgett RG, Lawrence VA, Cohn SL. Variations
in pharmacology of beta-blockers may contribute to
heterogeneous results in trials of perioperative
beta-blockade. Anesthesiology. 2010;113(3):585592.
34. Jessup M, Abraham WT, Casey DE, et al. 2009
focused update: ACCF/AHA Guidelines for the Diagnosis and Management of Heart Failure in Adults: a
report of the American College of Cardiology Foundation/American Heart Association Task Force on
Practice Guidelines: developed in collaboration with
the International Society for Heart and Lung
Transplantation. Circulation. 2009;119(14):19772016.
35. Smith SC Jr, Benjamin EJ, Bonow RO, et al; World
Heart Federation and the Preventive Cardiovascular
Nurses Association. AHA/ACCF Secondary Prevention and Risk Reduction Therapy for Patients with Coronary and other Atherosclerotic Vascular Disease: 2011
update: a guideline from the American Heart Association and American College of Cardiology
Foundation. Circulation. 2011;124(22):2458-2473.
36. Hammill BG, Curtis LH, Bennett-Guerrero E, et al.
Impact of heart failure on patients undergoing major
noncardiac surgery. Anesthesiology. 2008;108
(4):559-567.
37. Poldermans D, Schouten O, van Lier F, et al. Perioperative strokes and beta-blockade. Anesthesiology.
2009;111(5):940-945.
38. Bateman BT, Schumacher HC, Wang S, Shaefi S,
Berman MF. Perioperative acute ischemic stroke in noncardiac and nonvascular surgery: incidence, risk factors, and outcomes. Anesthesiology. 2009;110
(2):231-238.
JAMA, April 24, 2013—Vol 309, No. 16 1713
Corrected on April 23, 2013
Downloaded From: http://jama.jamanetwork.com/ on 06/05/2014