3.051J/20.340J Lecture 19 Drug Delivery: Controlled Release

3.051
J / 20 .340
J
Lecture 19
Drug Delivery: Controlled Release
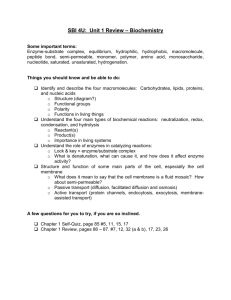
What do we mean by “controlled” release?
Control of: 1. delivery rate
2. release/activity
Need for Control drug concen.
toxic level
Traditional drug delivery
Therapeutic range t
1 t
2 time from administration longer period of dose efficacy = toxicity risk
1
3.051
J / 20 .340
J drug concen. toxic level
Controlled drug delivery
Therapeutic range time from administration
Types of Devices
1. Diffusion Controlled Delivery Devices
•
Monolithic Devices
•
Membrane Controlled Devices
•
Osmotic Pressure Devices
•
Swelling-Controlled Devices
2. Chemically Controlled Approaches
•
Matrix Erosion
•
Combined Erosion/Diffusion
•
Drug Covalently Attached to Polymer
•
Desorption of Adsorbed Drug
3. Electronic/Externally Controlled Devices
2
3.051
J / 20 .340
J
1. Diffusion Controlled Devices a) Monolithic Devices
Drug is released by diffusion out of a polymer matrix
Release rate depends on initial drug concentration i) Case of C
0
< C s
(drug concentration C
0
is below solubility limit in matrix C s
)
⇒
Diffusion through matrix limits the release rate
3 t
0
How can we control release rate? t
1
Rate control by choice of matrix : glassy matrix: D~10
-10
-10 rubbery matrix: D ~ 10
-6
-12
cm
2
-10
-7
cm
/s
2
/s t
2
3.051
J / 20 .340
J
Quantifying drug release
Governed by Fick’s Laws.
For 1D: The drug flux J is: J
= −
D dC dx
The change in drug concentration with time is:
∂
∂
C t
=
D
∂
∂
2 x
C
2
We want to calculate:
• dM t
•
M t
/dt = release rate
= amount released after time t
⇒
Solve Fick’s 2 nd
law with initial & boundary conditions.
Example: For a 1D slab loaded at an initial concentration of C
0
, with drug concentration in solution resulting in constant surface concentration of C i
.
δ
I.C.: C ( x ,0) = C
0
B.C. 1:
∂
C
∂ x x
=
0, t
=
0
B.C. 2: C(
δ
/2,t ) = C i
C
0
Solve for C(x,t) dM
Adt t
= −
D
( , ) dx x
= δ
/ 2
M t
A = cross-sectional area
C i
0
4
3.051
J / 20 .340
J
The amount of drug released is given by the series solution:
M t
M
∞
∞
∑
n
=
0
8
(
2 n
+
1
)
2 π
2 exp
⎡ −
⎣
D
(
2 n
δ
2
+
1
)
2 π
2 t
⎤
⎥
⎥ where: M ∞ = amount of drug released at long times
(e.g., total amt of drug: M ∞ = C
0
A
δ
= slab thickness
δ
)
M t
/M ∞
1
0.5
0
Release rate (from derivative) : dM t dt
=
2 M
∞
⎡
D
⎣ πδ
2 t
⎤ 1/ 2
⎦⎥ dM t dt
=
8 DM
∞
δ
2 exp
⎡ −
⎣
π
2
Dt
⎤
δ
2
⎥ time short times: ~ t
-1/2 long times: exponential decay
5
3.051
J / 20 .340
J dM t
/dt release rate
~ t
-1/2
NOTE: dM t
/dt and M t depend on geometry. See handout from
Encyclopedia of Controlled
Drug Delivery
~ exp(t )
0 time ii) Case of C
0
> C s
(drug concentration above solubility limit in matrix)
⇒
Drug dissolution in polymer matrix limits release rate
Higuchi model: assumes C i
= 0
M t
=
A DC s
(
2 C
0
−
C s
) t
⎤⎦ 1/ 2 dM t
=
A dt 2
⎣ DC s
(
2 C
0
−
C s
)
⎦⎤
1/ 2 t
−
1/ 2 drug conc.=
C s in matrix where A = surface area of the slab drug-rich
2nd phase
6
3.051
J / 20 .340
J
For C s
<< C
0
: dM dt t
=
A
⎡
2 DC C s 0
2 ⎣⎢
⎤ 1/ 2 t
⎥
How can we control release rate? b) Membrane Controlled Devices
Drug release is controlled by a semi-permeable membrane
⇒
Diffusion through membrane limits the release rate
Advantage: A constant flux device!
7
Semi-permeable membrane
Neat or concentrated therapeutic agent
Release rate thru membrane described by Fick’s 1 st
law.
For 1D:
J
= dM
Adt t
= −
D dC dx
Typical flux units: g/cm
2 s
3.051
J / 20 .340
J i) Nonporous semi-permeable membranes
⇒
Drug diffusion through swollen polymer membrane
Conc. inside membrane = C
2 dM t dt
=
DKA
δ
(
C
2
−
C
1
)
M t
=
DKA
δ
(
C
2
−
C
1
) t
K = membrane “partition” coefficient (unitless metric of drug solubility in membrane)
Which D is referred to?
Conc. outside membrane = C
1
δ dM t
/dt
Early release rate independent of time
8
0
Is this release profile advantageous? time
3.051
J / 20 .340
J ii) Porous semi-permeable membranes
⇒
Drug diffusion through membrane pores
Requires replacing D by D eff
:
D
= eff
D pore
ε
τ
ε = porosity 0 <
ε < 1
τ = tortuosity
τ ≥
1
9
Cross-section of porous semi-permeable membrane c) Osmotic Pressure Devices
Osmotic pressure build-up from water in-flux across semi-permeable membrane forces drug release through orifice piston
δ delivery orifice semi-permeable membrane osmotic “engine”
(NaCl) http://www.alza.com/alza/duros drug reservoir
Ex: DUROS Implant (ALZA)
•
Ti housing, 4mm
×
45 mm
•
~ 1 year duration
• in use for prostate cancer therapy
3.051
J / 20 .340
J
Release rate proportional to change in volume of drug reservoir: dM t
= dV dt dt
C
=
Ak
∆
δ
π
C
A = membrane area
∆π
= osmotic pressure differential
C = drug concentration in reservoir k = membrane permeability coefficient (~10
-6
-10
-7 g/cm/s) dM t
/dt zero-order release kinetics
10
0 time
Controlled Release via Solute Choice for Osmotic Engine (
∆π
)
Solute body tissue
Osmotic Pressure
(atm)
7
NaCl 356
KCl 245 sucrose 150 dextrose 82 potassium sulfate 39
3.051
J / 20 .340
J d) Swelling Controlled Devices
¾
Drug dispersed in a glassy, hydrophilic matrix
¾
Swelling in aqueous medium allows drug release glassy polymer matrix with dispersed drug
H
2
O swelling provides mobility for drug release
11
Complex release kinetics: modeled by fitting experimental data to power law expression.
M t
=
' n
M
∞ ln( M t
/M ∞ ) n = 1 ln( k’ ) ln( t )
3.051
J / 20 .340
J
2. Chemically Controlled Approaches a) Eroding Monolithic Device
Drug is incorporated into a bioerodible or dissolvable polymer matrix
12 t
0 t
1 t
2 i) Surface Erosion Devices dM t dt
= k A e e release rate = strong function of device geometry
A e
= instant surface area k e
= rxn or dissolution rate const.
For a slab:
A e
≈
2 M
∞
C
0
δ
≈ const dM t
=
2 dt k M e
∞
C
0
δ
⇒
zero-order release kinetics
δ
3.051
J / 20 .340
J dM t
/dt
0
For other geometries, A e is a function of time: dM t
= k A ( ) e e dt
For various geometries, the solution to this expression is: time
M t
M
∞
⎡
⎢
1 1
⎢
⎣
C
0
δ
2
⎥
⎦
⎥
⎥
⎤ n
Geometry
δ n cylinder diameter 2
13
3.051
J / 20 .340
J
Matrix Examples:
• polyanhydrides
poly(sebacic acid anyhydride)
O O
(-(CH
2
)
8
C -O- -)
N
• poly ortho esters DETOSU
14 ii) Bulk Erosion Devices
¾ uniform hydrolysis of bulk matrix polymer
¾ hydrolysis rate vs. drug diffusion controls release rate dM t ~ t n dt
Matrix Example: poly(lactide-co-glycolide)
⇒
n = -1/2 drug diffusion limited
O O
(-O-CH(CH
3
)-C -) x
r -(-O-CH
2
-C-) y
lactic acid glycolic acid
3.051
J / 20 .340
J iii) Pulsed release systems
Mixture of eroding particles with different degradation rates
Degradation Profile for Single Eroding Component (schematic)
% degrad.
100
50
0 drug concen. in vivo time in vivo
15 time from administration
3.051
J / 20 .340
J
Degradation Profile for Mixture of Components (ex., microspheres)
% degrad.
100
50
0 drug concen. in vivo time in vivo
16 time from administration
Applications Example: “one shot” vaccines with multiple antigens
TT tetanus toxoid
DT diptheria toxoid
HBSA hepatitis B surface antigen
SEB staphylococcal enterotoxoid B
Vaccines stimulate Ab production
⇒
How can we achieve different degradation rates?
3.051
J / 20 .340
J
Factors influencing degradation:
•
Composition (e.g., PLGA copolymer LA:GA ratio)
•
Geometry iv) Regulated systems
Incorporate a component that responds to the in vivo environment
•
Enzyme that catalyzes degradation in presence of a substrate
Example: GOD-regulated insulin release
Glucose + O
2
+ H
2
O
→
Gluconic acid + H
2
O
2
GOD pH drop promotes acid hydrolysis or swelling of matrix
17
3.051
J / 20 .340
J b) Polymer-Drug Conjugates
18
Therapeutic agent is covalently or ionically bound to a polymer through a cleavable bond
Purposes:
¾ increase resistance to proteolysis (protein drugs)
¾ reduce antigenicity/immunogenicity
¾ prolong plasma circulation lifetime
¾ enhance water solubility of hydrophobic agents
¾ reduce toxicity
Example 1: Therapeutic proteins tethered to polyethylene glycol (PEG) protein
⇒
Increases intravascular lifetime—why?
PEG
Some clinical systems:
•
PEG-adenosine deaminase (FDA appr. immunodeficiency therapy)
•
PEG-asparaginase (FDA appr. for lymphoblastic leukemia)
•
PEG-hemoglobin
•
PEG-interluekin 2
•
PEG-alpha interferon
•
PEG-colony stimulating factor
3.051
J / 20 .340
J
Example 2: Chemotherapeutic agent attached to water-soluble or hydrolysable backbone
19 vinyl benzyl fluorouracil
(CH CH
2
-) n maleic anhydride
(CH CH-) m
O=C C=O
O
C=O
N O hydrolysis
F
O
N
H
(CH CH
2
-) n
(CH CH-) m
O=C C=O
+
C=O
OH
OH OH
H
N O
F
O
N
H
5-fluorouracil
3.051
J / 20 .340
J
Example 3: Dendrimer Drug Conjugates (early development)
Dendrimers – sequentially synthesized, hyperbranched macromolecules
20
1 st
generation
2 nd
generation 3 rd
generation
Two strategies for controlled drug delivery drug-conjugated chain ends
Drug-filled core
(diffusion-controlled)
References
Encyclopedia of controlled drug delivery vol. 1, E. Mathiowitz, ed., John Wiley & Sons, NY, 1999.
Encyclopedia of controlled drug delivery vol. 2, E. Mathiowitz, ed., John Wiley & Sons, NY, 1999.
Biomaterials Science: An introduction to materials in medicine, B.D. Ratner et al., eds., Academic
Press, NY 1996.