Safety/Falls Risk Assessment Q. captured?
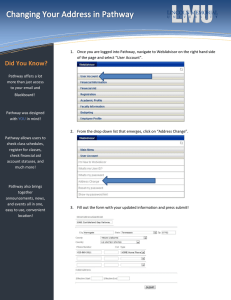
advertisement

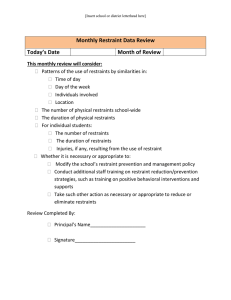
Safety/Falls Risk Assessment Q. If a patient is in restraints where will this now be documented and what elements need to be captured? A. The restraints documentation is now under the Safety Care Implemented section of the Safety/Falls Risk Assessment. The nurse should document every 2 hours the status of restraints as “on” or “off” along with the Restraint and Safety Comfort Care. When hovering over the Restraint and Safety Comfort Care field, required elements that the nurse is documented against are listed so that when the nurse documents “done” it is acknowledged that all of these elements have been performed. If for some reason one of more required action could not be done, check the box but add an annotation stating why an action was not done. Q. Should I now always have a safety priority problem present? A. A Safety Priority Problem should always be intitated/maintained when a patient is restrained. For patients not restrained, Regardless of acuity, prioritizing problems and determining the focus for care on a given shift often requires complex decision making. Some general principles that may help: If the patient is NOT tracking as expected against the pathway, what is causing the variation? That is probably a priority problem. For example, if a patient on an Abdominal Aneurism Repair pathway is meeting all goals on the pathway at the expected time EXCEPT by Post Op Day 2, they have still not successfully ambulated, then Activity Tolerance (or perhaps Pain or some other reason that is preventing them from meeting the Activity Goal) would be a Priority Problem. If the patient has co-morbidities not covered by the Pathway, there may be Priority Problems that are not being addressed related to those co-morbidities. For example, if a patient with ADRS related to Sepsis is also a Diabetic and they are experiencing unstable glucose control, that might be a Priority Problem. What is going on with the patient that may prolong the LOS in the ICU or the overall ? Any kind of complication (eg. a Fall, a Pressure Ulcer, etc.) would warrant consideration as a Priority Problem. Finally, focus on “nursing-centric” problems. For example, a patient with Meningitis would likely have several significant problems but nursing care is more likely to drive desired outcomes for some problems than others. For example, a skin breakdown issue or preventing injury with in a confused, restrained patient are things nurses can more directly impact and may therefore make more sense as priority problems than the Infection. Remember, you are only making decisions for your 12 hour shift and if the patient condition changes during your shift, you can always alter your focus. There’s not usually a right or wrong answer but we hope you’ll see value in the decision making process required to determine the specific problems and outcomes that will drive your care for your shift. In general, there should usually be no more than 3-4 active priority problems – the exception being when placement of Restraints might add a 5th PP. Q. Can we make Morse Falls Risk Score viewable within the OPC ? We are working on this right now and expect to have this available at some point during this pilot.