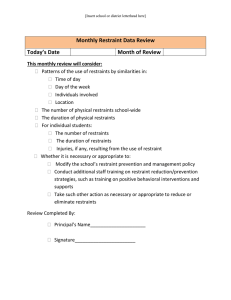
Safety ● freedom from danger, harm, or risk ● promotes safe, effective, person-centered delivery of care Hospital Errors ● medical errors are more frequently due to system problems rather than human error Culture of safety ● Prioritize safety over getting work done ● Core beliefs and values a. acknowledgment of the high-risk nature of health care and the commitment to safe operations b. maintenance of a blame-free environment where reporting is protected and expected c. promotion of teamwork and collaboration to prevent and seek solutions to patient safety issues d. systems-based perspective where the organization commits resources to address actual/potential safety issues Interconnected areas 1. culture, leadership and governance by leaders, governing bodies, and policymakers focused on safety 2. patient and family engagement that includes partnering in all aspects of their care 3. workforce safety and resilience using a systems perspective 4. establishing a network that supports continuous learning and information sharing a. These acts are meant to ADVANCE PATIENT SAFETY DRUG USE AND POISONING ● Drug use trends among college-age adults (ages 19 to 22 years) ● Accidental postining comes from misreading meds and not taking interventions to prevent death ● Such as properly labeled containers ● Items in reach for adults ● Prevention Measures include ○ Medication Calendar ○ Request large-print labels from your pharmacist ○ Report side effects from medications to your health care provider ○ Do not stop taking any prescription drug or change the dose without first consulting the provider or nurse. Intimate partner violence (IPV) involves: ● physical violence (hitting kicking, or other physical force), sexual violence (forcing a sex act, sexual touching, or a nonphysical event without consent), stalking (a pattern of repeated, unwanted attention and contact) and/or psychological aggression ● As a nurse we can ask questions if we suspect abuse ● For example a patient comes in with a ton of bruises and swelling and states they tripped walking ● This could be a sign of IPV so speaking in private and asking questions can help save this patient Intersectionality ● where race, sex, gender, class, and other individual characteristics intersect and overlap with one another, often leading to an increased burden of discrimination on several fronts and other negative outcomes FALLS ● Common in Older Adults 65+ ● falling can also cause anxiety and panic, which may make an older adult more vulnerable to a fall ● Assessments we can make include looking at history and examinations ○ ● Major causes of falls in the home include ○ ● Assistive devices that are used to prevent falls such as Cane or Walker slippery surfaces, poor lighting, clutter, and improperly fitting clothing or slippers Preventing Falls in the home ○ installing handrails in bathrooms and on stairs, ensuring good lighting, and discarding or repairing broken equipment around the home Environmental Concerns work environment ● People who work in certain occupations may experience exposure to health hazards, such as excessive noise, pollution, toxic chemicals or vapors, or infectious agents social environment ● Willing to take risk or avoid things that keep you safe ● For safety we wear seat belts in our cars. People that avoid doing this are making a voluntary choice. Involuntary would be if you got into a car with friends and none of the seat belts work. home environment ● Bad influences and actions that are not taken correctly Fire Safety/home safety ● people who die in house fires die of smoke inhalation rather than burns ● Interventions include smoke alarms ● Having a safety plan with your family on where to meet after a fire will keep you safe and ensure the better survival rates electric shock ● Overloaded electrical circuits, faulty appliances, frayed wires, careless use of electrical equipment, and handling of electrical devices and cords with wet hands or while wearing wet shoes can result in injury or death sensory perception ● Any impairment in sight, hearing, smell, taste, or touch can reduce a person’s sensitivity to the environment. Vision changes may cause a person to stumble, lose their balance, and fall ● Any patient with hearing loss or loss of smell are also at risk of following the incorrect directions and not being able to smell or hear fire/fire alarms ability to communicate ● Fatigue, stress, medication, aphasia, and language barriers are examples of factors that can affect personal communication and prevent the patient from accurately perceiving events Knowledge ● Patient teaching about safety is crucial and must be individualized, take into account health literacy, and be leveled appropriately for patients and families. stroke (cerebral vascular accident) orienting the person to surroundings ● Explaining to patients there new change in environment will help to keep them safe ● Explaining call lights, where the bathroom is, what they can physically do, how to use the call button, are important to explain to patients sentinel event ● which is an unexpected occurrence involving death or serious injury never event ● (medical error that should never occur) ● If this does happen and gets identified by a healthcare insurance provider the hospital will now take on the financial responsibility of the patient Prevent Falls in a Healthcare Facility ● Complete a risk assessment ● Leave a night light on ● Move bedside commode out of sight to discourage attempts at independent transfer using restraints in health care facilities Restraints (ONLY USE AS A LAST RESORT) ● are physical devices or chemical means used to limit a patient’s freedom and movement that cannot be easily removed (or eliminated) by the patient. ● Side rails, geriatric chairs with attached trays, and appliances tied at the wrist, ankle, or waist are types of physical restraints control behavior ● We would give chemical restraint which is used to help calm down patient or help with confusion ● This is a really great method to prevent a physical restraint from being needed Side Rails ● Using side rails can be considered a sign of a restraint ● It is not a restraint if the patient ask for the side rails to be up to aid them ○ Such as with sleep and not wanting to fear rolling out of bed ○ Sense of comfort and safety Restraint alternative ● Ambularm device ○ ○ Used to help notify personal when patient is out of bed RACE ● Rescue anyone in immediate danger ● Activate the fire code system and notify the appropriate person ● Confine the fire by closing doors and windows ● Evacuate patients and other people to a safe area Notes Based off practice questions Children Safety ● When conducting safety with children in vehicles some of the most important details such as car seats apply to all children ● Any child or infant must use Booster seats until they are 4′9″ tall and weigh between 80 and 100 lb Infants ● Safety with young infants impose a very scary and real problem ● Infants must be in the supine position when they are sleeping ● If they are placed into a prone position the child now sufferers the chance of sufferaction postural hypotension ● When your blood pressure drops when you go from lying down to sitting up, or from sitting to standing ● Sudden movement such as moving patient from bed to chair Nonadherence ● failure of an individual to follow a prescribed therapeutic regimen long-term healthcare facility Developmental Risk Factors ● Imposes potential risk for patients to not grow or develop if they are known to have potential issues ● Patients such as fall risk patients potentially can be affected since the end goal for theses long term care patients is to have them grow and develop over time (Improve) Reduce the client's chance of experiencing a fall ● A person who is familiar with his or her surroundings is less likely to experience an accidental injury. As part of the hospital admission routine, it is important to orient the client to the safety features and equipment in the room. Benzodiazepine/antiepileptics ● benzodiazepines and antiepileptics are more predictive of falls than are other drug families. Activated charcoal ● Activated charcoal is the most common treatment for many poisonings Narcotics ● are administered to manage pain Antihistamines ● are prescribed to manage allergy conditions Antacids ● are prescribed to manage gastrointestinal disorders anthrax bacillus ● We would use Antimicrobials oncology care unit ● On oncology divisions, the nurse is continually exposed to antineoplastic agents ● provide patients with cancer specialized nursing care ●