NEO111 M. Jorgenson, RN BSN Patient Safety, Comfort, & Mobility
advertisement

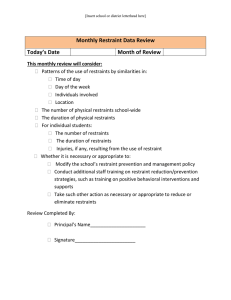
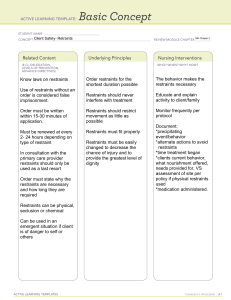
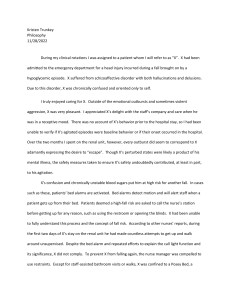
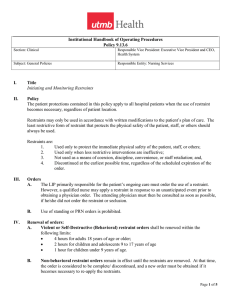
Patient Safety, Comfort, & Mobility NEO111 M. Jorgenson, RN BSN Patient Safety Fall Prevention: Everyone’s Responsibility FALLS are the fifth leading causes of death among Americans aged 75 years and older the second leading cause of mortality from related injuries in adults >65 years Elderly person who sustains a fall are more likely to die within a year’s time of the fall. Considine J, Botti M. Who, when and where? Identification of patients at risk of an in-hospital adverse event: implications for nursing practice. Int J Nurs Pract. 2004;10(1):21–31. Restraints Physical restraints considered as a last resort after other care alternatives have been unsuccessful The least restrictive restraint should be used and it should be removed at the earliest possible time Must be ordered by a MD or other licensed independent practitioner Special monitoring/ assessment Must be reassessed by ordering MD in 24 hours and new order obtained Alternatives to Restraints Ask family to stay with patient Rule out physical causes for agitation Reduce stimulation Use electronic alarm system Check for environmental hazards Offer diversion activities Consider relocation closer to nurse’s station Conceal tubes and tubing necessary for care Types of Restraints Extremity restraints Jacket or vest restraint Hand Mitt Elbow restraints Leather restraints Mummy restraints Bed alarms Restraints cont. Must be able to insert 2 fingers between restraint and pt’s ankle or wrist Restraint must be fastened on moveable part of bed frame, NEVER side rail Use a quick-release knot to tie Must be able to insert a fist between vest restraint and patient When assessing a restraint, must assess CMS Circulation Motor Sensation Call bell must be within reach Mobility Effects of Immobility Cardiovascular system Increased cardiac workload, orthostatic hypotension and venous thrombosis Respiratory system Decreased ventilatory effort and increased secretions Gastrointestinal system Poor digestion and utilization of food Constipation Urinary system UTI and renal calculi Effects of Immobility cont. Musculoskeletal system Atrophy, osteoporosis Metabolic system Decrease in metabolism Integument system Skin breakdown Psychological well-being Diminished self-esteem, social disturbances Preparing for Activity. Be organized and plan ahead Anticipate changes/complications Prevention versus treatment Develop good habits Proper alignment Planning Check MD orders, Nursing plan of care, PT notes, and history for any limitations on mobility Conduct a pain assessment and provide appropriate interventions Talk with the patient Talk with other members of the team Gather equipment Develop a plan Planning cont. Know policies and procedures for facility Ensure adequate assistance for nurse and patient safety Prepare for smooth, coordinated transfer-only one leader Engage brakes on equipment Body Mechanics Comfortable working height Good posture Feet shoulder width apart (wide base of support) Use large leg/arm muscles (not back) Gluteal and abdominal muscles engaged (internal girdle) Low center of gravity Body Mechanics cont. Flex knees (and hips) Head up Back straight –no twisting Smooth, coordinated movements Position self close to object Rocking motion (forward-push/back-pull) Patient Positioning Bed position Arms across chest Knees flexed and feet flat Ensure proper body alignment Trapeze bar Avoid friction/shearing Special Considerations Change patients positions frequently Smoothe clothes and linens Encourage deep breathing and coughing Apply antiembolism stockings Pad bony prominences Bed in lowest position Pillows Positioning & Protective Equipment Mattresses Hand splints Side rails Trochanter rolls Adjustable beds Heel boot Trapeze bar Foam pads Hand rolls Footboard Range of Motion Promotes circulation, prevents contractures, and provides joint mobility. Move each joint until there is resistance but not pain Incorporate into ADLs Teach patient and family Encourage pt to do as much as possible Anti-embolism Stockings Used to enhance blood flow and venous return Patient should be measured for the correct size. Assess extremity for pulses, edema, movement, sensation (CMS) Remove and check skin q 8 hours