Document 13111133
advertisement

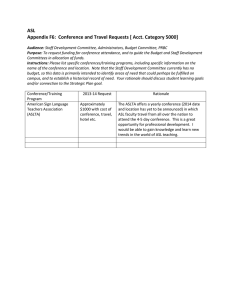
ASL Methods and Poten/al for pHMRI Michael Kelly, PhD Layout • Introduc/on to cerebral perfusion • Arterial spin labelling • • • • • Basics Techniques (con/nuous ASL, pulsed ASL, pseudo-­‐con/nuous ASL) Quan/fica/on of CBF (Buxton model, alterna/ves) Typical setup for pCASL experiment Current applica/ons (at FMRIB) • Poten/al of ASL for pHMRI • Advantages • Confounds • Recent pHMRI ASL studies Introduc/on • Cerebral perfusion – “the process involved in the delivery of nutri/ve blood to the brain /ssue capillary bed” • Various modali/es: PET, SPECT, CeCT, Doppler ultrasound…. • Many parameters: CBF (ml/100g /ssue/min), CBV (ml/100g), MTT (s), blood velocity (cm/s)….. • Two main quan/ta/ve MRI techniques: DSC-­‐MRI & ASL Introduc/on • Why might we want to measure / quan/fy cerebral perfusion? • Altered in various disease states… • Stroke -­‐ possible to iden/fy ischaemic core and penumbra of possibly salvageable /ssue: (1) CBF map from stroke survivor shows ischaemic region (measured by ASL) • Hyperperfusion in tumours: (2) CBF map of glioblastoma. Hyper-­‐ perfusion within periphery (measured by ASL) (1) Brumm et al, Neuroimage, (2010) 51(3):995-­‐1005. (2) Deibler et al, AJNR, (2008) 29:1428-­‐1435. Introduc/on • Func/onal MRI… • • • BOLD signal is a combina/on of changes in CBF, CBV and CMRO2 BOLD signal % -­‐ not a quan/ta/ve physiological parameter Direct measures of CBF and CBV may be more closely localised at the site of neuronal ac/vity Combined BOLD & ASL CMRO2 (and more…) • www.fmrib.ox.ac.uk/educa/on/fmri MRI perfusion techniques DSC-­‐MRI • Capture first pass of intravenously injected bolus of paramagne/c contrast agent (Gadolinium) • Contrast is either relaxivity (T1) / suscep/bility (T2 and T2*) based Østergaard, JMRI, (2005) 22:710-­‐717 MRI perfusion techniques Note the units of the perfusion parameters! Drawbacks: • Requires injec/on of exogenous contrast agent • Quan/fica/on requires accurate measurement of arterial input func/on • Not suitable for longitudinal experiments / mul/ple measurements • Not suitable in certain disease states Non-­‐invasive quan/ta/ve MRI method?? – ASL (1) Ohtonari et al, Neurol Med Chir, (2008) 48:331-­‐336. ASL -­‐ Basics Arterial Spin Labelling (ASL) • Acquire tag image inflowing arterial blood water labelled by magne/c inversion: Time delay between 1 and 2: Labelled water reaches capillary bed and is exchanged with water molecules in the /ssue signal change • Acquire control image inflowing blood is not labelled: • Difference between control and tag image is perfusion-­‐weighted: www.umich.edu/~fmri/asl.html Arterial Spin Labelling: Tag Imaging slice Inflowing arterial blood water Arterial Spin Labelling: Tag Imaging slice Inflowing arterial blood water Inversion Arterial Spin Labelling: Tag CBF (inverted spins) arteries veins capillaries Arterial Spin Labelling: Tag CBF arteries veins capillaries Arterial Spin Labelling: Tag CBF arteries veins capillaries Arterial Spin Labelling: Control Imaging slice Inflowing arterial blood water Arterial Spin Labelling: Control Imaging slice Inflowing arterial blood water Inversion Arterial Spin Labelling: Control CBF arteries veins capillaries Arterial Spin Labelling: Control CBF arteries veins capillaries Arterial Spin Labelling: Control CBF arteries veins capillaries Arrival of labelled blood Flow Arterial Arrival Time Whole-­‐brain CBF maps CBF (ml / 100 g /ssue / min) Whole-­‐brain AAT maps AAT (seconds) ASL -­‐ Techniques (Con/nuous ASL, Pulsed ASL, Velocity-­‐selec/ve ASL) Con/nuous Arterial Spin Labelling (CASL) • First ASL technique (2) Control • 3 – 4 sec RF pulse with magne/c field gradient in direc/on of arterial flow: Label Δr Mcontrol Mlabel ∆M • Label: inflowing spins inverted by principle of flow-­‐driven adiaba/c inversion • Control: fl -­‐fl (or G -­‐G): inflowing spins are unaffected Adapted from (1) • Host sequence (e.g. EPI, GRASE) played arer /me delay (“post labelling delay”) • ΔM=Mc-­‐Ml perfusion weighted image (1) Petersen et al, Br J Radiol, (2006) 79:688-­‐701 (2) Williams et al, Proc Natl Acad Sci, (1992) 89:212-­‐216 Adiaba/c inversion RF pulses • Before understanding how flowing spins are inverted in CASL, we need to look briefly at adiaba/c inversion pulses… • Amplitude and frequency of adiaba/c inversion pulses depends on /me: A(t) and ωrf(t) • The net magne/za/on vector, M, precesses around Beff in the rota/ng frame • Principle of adiaba/c fast passage M follows Beff provided direc/on of Beff does not vary too much during one precession of M about Beff • By modula/ng A(t) and ωrf(t), Beff can be swept from +z to –z and if adiaba/c condi/on is sa/sfied, M will follow and be inverted (1) M.A. Bernstein. Handbook of MRI Pulse Sequences. Oxford: Academic Press, 2004 Adiaba/c inversion RF pulses (Used to invert large volume of spins in PASL) Flow-­‐driven Adiaba/c Inversion • Back to CASL…apply fixed RF (no amplitude or frequency modula/on) for 2 -­‐ 4 secs: No /me-­‐dependency on either A or ω • We know this pulse cannot adiaba/cally invert sta/onary (/ssue) spins (Why?) • Recall that a gradient G=Gz is applied along with the RF: Gz z • For flowing spins, B0 is swept due to Gz Spins flowing with constant velocity along z experience a linearly varying magne/c field and a resultant sweep of the resonant frequency (1) M.A. Bernstein. Handbook of MRI Pulse Sequences. Oxford: Academic Press, 2004 Flow-­‐driven Adiaba/c Inversion v • Spins moving towards r0 from r(t)<<r0 experience a /me-­‐varying frequency offset: r >> r0 r > r0 Labeling plane r < r0 r = r0 • And an effec/ve magne/c field given by: r << r0 • If velocity of flowing spins is within the correct range, this frequency offset acts on flowing spins like an adiaba/c pulse as Beff is swept by changing Δω: (1) M.A. Bernstein. Handbook of MRI Pulse Sequences. Oxford: Academic Press, 2004 Flow-­‐driven Adiaba/c Inversion (1) v z r >> r0 r > r0 Labeling plane r = r0 y r < r0 r << r0 x Spins far from labeling plane Δω is large (propor/onal to r(t) – r0) Flow-­‐driven Adiaba/c Inversion (2) z y x Spins approaching labeling plane Δω decreasing (propor/onal to r(t) – r0) Flow-­‐driven Adiaba/c Inversion (3) z y x Spins at the labeling plane Δω goes to zero (propor/onal to r(t) – r0) Flow-­‐driven Adiaba/c Inversion (4) z y x Spins moving away from labeling plane Δω starts to increase but is now posi/ve (propor/onal to r(t) – r0) Flow-­‐driven Adiaba/c Inversion (5) z y x Spins flowing into brain Δω is large (propor/onal to r(t) – r0) and flowing spins are inverted! Magne/za/on Transfer Effects • CASL – apply long off-­‐resonance RF pulse • Schema/c diagram of absorp/on spectra of free water and macromolecule protons(1): At the imaging plane ASL labelling pulse • Free water protons at the imaging plane are largely unaffected (due to narrow RF absorp/on spectrum) • Protons bound to macromolecules at imaging plane are inverted by the off-­‐ resonance labelling pulse (due to broad spectrum of immobile protons) • Chemical exchange between the two proton pools magne/za/on transfer • Used as a posi/ve contrast mechanism (MTI – magne/za/on transfer imaging) but problema/c in ASL….why? (1) Grossman et al, Radiographics, (1994) 14:279-­‐290 Magne/za/on Transfer Effects • Water in sta/c /ssue appears to be inverted due to magne/za/on transfer • This adds to the blood water signal that we want to measure with ASL but is not true perfusion signal • Overes/mate ASL difference signal Magne/za/on Transfer Effects Label off-­‐ resonance pulse (fL) Control off-­‐ resonance pulse (-­‐fL) • To compensate for MT effect in ASL control image acquired with frequency offset fc = -­‐fL • ΔM=Mc-­‐Ml MT contribu/on should be the same in both the tag and control image removed by subtrac/on BUT • Assumes MT effect is symmetrical about ω0 • ΔM/M0 is the frac/onal signal difference between an image acquired with frequency offset +δω2 and one acquired with with frequency offset -­‐δω2 • MT effect is not symmetrical this label / control scheme (+/-­‐ fl) s/ll leads to an error in subsequent perfusion es/ma/on (1) Pekar et al, MRM, (1996) 35:70-­‐79 Magne/za/on Transfer Effects • Best solu/ons to MT problem -­‐ use dedicated labelling coil(1) • Small sensi/ve region of coil no satura/on of macromolecules at the imaging region • Can be used to easily selec/vely label main feeding arteries(2): (1) Zhang et al, MRM, (1995) 33:370-­‐376 (2) Werner et al, MRM, (2004) 52:1443-­‐1447 Pseudo-­‐con/nuous ASL • CASL drawbacks: – Magne/za/on transfer (as we have just described) – Inversion efficiency (<< 100%) – Requires applica/on of long RF pulse (“con/nuous mode opera/on”) • Pseudo-­‐conJnuous ASL (pCASL) (a) Label: B1ave≠0, Gave≠0 (b) Control: B1ave=0, Gave=0 – Magne/za/on transfer is matched between tag and control – High inversion efficiency (typically 90% increased SNR) – Can be implemented on clinical systems that do not support con/nuous RF (1) Dai et al, MRM, (2008) 60:1488-­‐1497 Pseudo-­‐con/nuous ASL Sweeping the phase shir accumulated between RF pulses results in an inversion of flowing spins • Control (doKed line): 1800 phase shir for all posi/ons (alternate sign of RF pulse + zero net gradient) • Label: Imbalance in gradients Posi/on dependent phase shir • Changing gradient imbalance sweep ϕ from -­‐1800 to +1800 causes inversion of flowing spins (1) Garcia et al, Proc ISMRM, (2005) 13:37 (2) Dai et al, MRM, (2008) 60:1488-­‐1497 Pseudo-­‐con/nuous ASL Mul/slice perfusion weighted images from pCASL experiment Vessel-­‐encoded pCASL Perfusion territory image • pCASL labelling scheme (RF and Gz) • Add transverse gradient blips (Gxy) can label selec/vely (e.g. along line A) • RF pulse phase cycled such that spins in the tag vessel (e.g. A) are inverted while spins along control vessel (e.g. B) are unaffected • Different tag / ctrl vessel combina/ons are possible Vessel-­‐encoded dynamic angio (1) (1) Okell et al, MRM,(2010) 64:698-­‐706 Pulsed Arterial Spin Labelling ConJnuous and pseudo-­‐conJnuous ASL (CASL and pCASL): • Label for a given /me at a specific loca/on (i.e. in the neck) Pulsed ASL (PASL): • Label a large volume of blood with short RF pulse • Typically use adiaba/c RF pulse (described earlier) • Wait for labeled volume (or bolus) to flow into capillary bed and exchange with /ssue • Two “families” of PASL sequence: – Echo planar and signal targe/ng with alterna/ng RF (EPISTAR) – Flow sensi/ve alterna/ng inversion recovery (FAIR) • Quan/ta/ve imaging of perfusion using a single subtrac/on (QUIPSS) EPISTAR(1) Saturate spins at the imaging loca/on fl Dephase transverse magne/za/on prior to labeling fc=-­‐fl Spa/ally selec/ve adiaba/c inversion pulse • ΔMEPISTAR=MC -­‐ ML • Doesn’t account for MT asymmetry problem • PICORE drop the slab selec/on gradient in the control phase (problem with this?) • Other EPISTAR–type sequences: STAR, STAR-­‐HASTE, TILT…. (1) Edelmann et al, Radiology,(1994) 192:513-­‐520 FAIR(1) Slice selec/ve gradient: 1800 pulse only inverts spins at the imaging loca/on No slice selec/ve gradient: 1800 pulse inverts spins in the en/re sensi/ve region • ΔMFAIR=ML – MC • No off resonance RF not sensi/ve to MT effects • Other FAIR-­‐type sequences: UNFAIR, FAIRER (1) Kwong et al, Radiology,(1994) 192:513-­‐520 Quan/fica/on? • In order to quan/fy, generally vary post labelling delay and image mul/ple /me-­‐ points (usually called inversion /me (TI)= labelling dura/on + post labelling delay) • Track /me-­‐course of flowing spins at the imaging loca/on (more on this in quan/fica/on sec/on…) Voxel with arrival Time of ~200ms Voxel with arrival Time of ~500ms ? • • Transit /me sensi/vity: ΔM depends on what TI is used (in a single TI experiment) CBF quan/fica/on from single TI? Are rela/ve perfusion values between regions valid? (1) Petersen et al, Br J Radiol,(2006) 79:688-­‐701 QUIPSS • Reduces the transit /me sensi/vity of single-­‐TI PASL techniques(1) • Inplane satura/on applied arer TI1 removes contribu/on to the final difference image of spins that arrived before TI1 • Only labelled blood that arrives at the imaging loca/on between TI1 and TI2contributes to the perfusion weighted signal • Reduces transit /me sensi/vity more confidence in quan/fica/on • QUIPSS2 apply satura/on pulse at the labeling plane instead (1) Wong et al, MRM,(1998) 39:702-­‐708 Velocity Selec/ve ASL(1) • CASL and PASL label spins based on their loca/on (spa/al selec/vity) • VS-­‐ASL modulates longitudinal magne/za/on of flowing spins based on their velocity • Uses a velocity selec/ve scheme • Gradients induce a velocity-­‐dependent phase shir between each pair or RF pulse train elements: • These parameters define a cut-­‐off velocity, Vc • Only spins with V > Vc are labeled • Image acquisi/on only includes spins with V < Vc • Only decelera/ng spins are included arteriole / capillary specific (excludes venous blood) (1) Wong et al, MRM,(2006) 55:1334-­‐1341 ASL -­‐ Quan/fica/on ASL Quan/fica/on • Mul/-­‐TI ASL experiment ΔM(t) (ASL difference signal is measured as a func/on of /me) pCASL data: Labelling dura/on=1.4s, 6 x PLDs • Mathema/cal model for ΔM(t), containing flow term, T1, describing exchange of labelled water between blood and /ssue, etc. QuanJfy CBF • Fit model to data Quan/fy physiological parameters (i.e. CBF, AAT) ASL Quan/fica/on • Typically use the Buxton(1) general kine/c ASL model • ΔM(t) constructed as a sum over /me of the delivery of magne/za/on to the /ssue ΔM(t) = difference signal measured by ASL α = inversion efficiency (between 0 and 1) M0b = equilibrium magne/za/on of blood f = cerebral blood flow (CBF) Integeral = convolu/on of delivery func/on, c(t), with product of residue func/on, r(t), and magne/za/on relaxa/on func/on, m(t) • Fit to the solu/on to this equa/on for the type of ASL data you have acquired (i.e. CASL, PCASL or PASL) • Get voxel-­‐by-­‐voxel map of CBF (and possibly arterial transit /me (ATT)) (1) Buxton et al, MRM,(1998) 40:383-­‐396 ASL Quan/fica/on pCASL data: Labelling dura/on=1.4s, 6 x PLDs Perform voxel-­‐wise fit of CASL solu/on to general kine/c model to data (need to assume / measure values for T1, α, M0b,λ) ASL Quan/fica/on pCASL data Model fit ASL Quan/fica/on Effect of varying CBF, arterial transit /me, T1 and labelling dura/on on the general kine/c model: (1) Buxton et al, MRM,(1998) 40:383-­‐396 M0,blood Calibra/on • • Look again at the the equa/on for ΔM(t): Before CBF can be obtained in absolute units (ml/100g /ssue/min), need to measure M0,blood and es/mate or measure α M0,blood Calibra/on Measuring M0b: • Measure equilibrium magne/za/on of CSF and use this to calculate M0,blood • Acquire iden/cal image (e.g. EPI / GRASE) to ASL acquisi/on, without labelling and with long TR • Calculate mean CSF signal (i.e. within a CSF mask) M0,csf • Calculate M0,blood from the following rela/onship: • Where λ = ρblood/ρcsf = 0.87 (ml/ml) and we also correct for T2* (for gradient echo) decay of the signal within the echo /me(1) (1) Hersovitch & Raichle, JCBFM,(1985) 5:65-­‐69 Inversion Efficiency • Degree of inversion (α) achieved by labelling scheme: • CASL ≈ 0.7 -­‐ 0.8 • Can vary significantly as a func/on of velocity studies involving hypercapnia challenge (CO2)? • Aslan et al Combine phase-­‐contrast and pCASL to measure αpCASL decreased from 0.95 to 0.84 during inhala/on of 5% CO2 • Cardiac cycle, intra-­‐subject variability in BP etc need to measure on per-­‐subject basis? pCASL ≈ 0.9 – 0.95 (1) Aslan et al, MRM,(2010) 63:765-­‐771 Sources of error in General Kine/c Model (1) • Assumes plug flow no labelled spins arrive at the imaging region before Δt • Range of transit /mes more likely can lead to underesJmate of perfusion (especially with PASL) should account for distribu/on of arrival /mes (2) • Single-­‐compartment kine/cs assumes rapid exchange of labelled spins between vessels and /ssue • Some labelled spins may remain in vessels before being exchanged (some may even pass through the voxel without undergoing exchange(1)) • This assump/on also leads to an underesJmaJon of perfusion (3) • Labeled magne/za/on is assumed to decay with /ssue T1 on arrival at the imaging voxel • This assump/on leads to an overesJmaJon of perfusion (1) Silva et al, MRM,(1997) 38:232-­‐237 Typical PCASL experiment setup (1) Run /me-­‐of-­‐flight angiography to visualise vessels in the neck: (2) Run ASL sequence: (3) Run calibra/on scan(s) for M0blood calcula/on: ÷ Head coil = Body coil Sensi/vity map ASL -­‐ Current applica/ons Current ASL applica/ons (1) Okell et al, MRM,(2010) 64:698-­‐706 Current ASL applica/ons (1) Okell et al, MRM (2010) Current ASL applica/ons Kelly et al, BRAIN (2011) Current ASL applica/ons ASL + BOLD weighting (TE) + gas challenges Bulte et al, Neuroimage (2012) Current ASL applica/ons Whole-­‐brain PCASL acquisi/on, focal pain s/mulus What about 7T? • T1 of blood changes from ~1600ms at 3T to ~2000ms at 7T • Labeled signal will decay more slowly • Improved CNR and ability to acquire more slices? But… • B1 homogeneity in the neck? need specific labeling coil? • Specific absorp/on rate – more RF power needed? ASL – Poten/al for pHMRI Advantages of ASL for pHMRI • Non-­‐invasive (compared to PET) – suitable for longitudinal studies • CBF – single physiological parameter quan/fied in absolute units • Don’t need to use s/mulus / task response to drug effects • Quan/fy CBF at rest and during s/mulus: – Separate effects of pharmacological agents on baseline and task-­‐ induced ac/va/on – NB where task-­‐based studies may be affected by deteriora/ng performance (clinical popula/ons) Advantages of ASL for pHMRI • Baseline CBF affects the func/onal CBF response (during visual s/mulus) but not the BOLD response (CMRO2 / CBF coupling) • Ability to detect baseline CBF with ASL (versus BOLD) is advantageous Advantages of ASL for pHMRI • Pairwise (control-­‐tag) subtrac/on in ASL acts as a high pass filter • Frequency spectrum of ASL /me series is flat (“white noise”) -­‐ as opposed to BOLD which has elevated power at low frequency • ASL is more suitable for studying slow changes in brain func/on (e.g. drug effects taking hours / days) Power BOLD –high power at low frequency 0 0.005 0.010 0.015 Ff 0.020 0.025 Frequency Frequency (Hz) Aguirre et al, Int Rev Neurobiol (2005) Advantages of ASL for pHMRI • BOLD – EPI suffers from distor/on and dropout • ASL – can use alterna/ve sequences that are resistant to magne/c field inhomogeneity (suscep/bility) effects • Improved visualiza/on of orbitofrontal, temporal and limbic regions (linked to neurotransmi…er systems) Advantages of ASL for pHMRI • 3D GRASE readout: • Aside: data demonstrates importance of acquiring mul/-­‐TI ASL data MacIntosh et al, JCBFM (2008) Advantages of ASL for pHMRI • Drug ac/on /mes range from seconds (intravenous) and hours (oral) to days and weeks (treatment cycle) • Need high test-­‐retest reliability (precision) reliability accuracy • Within-­‐subject coefficient of varia/on ~10% for global CBF and ~15% for regional measures • To detect a 15% change in CBF with 90% power and 15% varia/on between repeated measures requires ~20 subjects Wu et al, MRM (2007), Wang et al, JPET (2011) Recent important technical advances • • • • • Increased field strength Parallel imaging (increased SNR and temporal stability) Recent progress in commercialisa/on pCASL – increased labelling efficiency and SNR Background suppression to suppress background /ssue – reduces physiological noise and sensi/vity to mo/on – improves sensi/vity and temporal stability – whole brain coverage, 4mm isotropic in a few minutes Fernandez-­‐Seara et al, MRM (2008) Challenges for ASL • CBF measured by ASL – s/ll an indirect measure of regional brain func/on • Vascular confounds -­‐ Some agents may directly alter CBF (or mediators or neurovascular coupling) rather than brain func/on itself • e.g. Caffeine: • But….no change significant change in CMRO2 (measured by calibrated BOLD/ASL) coupling between CBF and CMRO2 is altered Wang et al, JPET (2011) and Perthen et al, Neuroimage (2008) Challenges for ASL • 4 doses of remifentanil PaCO2 increases with increased seda/on global CBF increase (global systemic CBF increase -­‐ A) • Need to normalize regional CBF by global CBF to iden/fy remi-­‐induced regional CBF varia/on (limbic CBF effect – B) Ko‡e et al, Anesth Analg (2007) Future direc/ons • Con/nued improvement in hardware and sequence development • Further move towards calibrated ASL or ASL/BOLD CBF, AAT, CMRO2, OEF, CBV • Perfusion-­‐based fMRI / pHMRI long behavioural tasks (stress, craving, pain…) Ques/ons?