Comparative Review of Ultrasound Based Siddhi Bhandarkar
advertisement

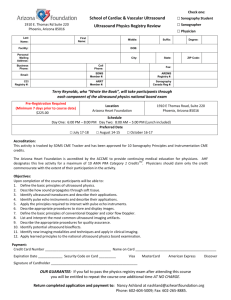
International Journal of Engineering Trends and Technology (IJETT) – Volume23 Number 3- May 2015 Comparative Review of Ultrasound Based Techniques used for Diagnosis of Prostate Cancer Siddhi Bhandarkar[1], Antara Dandekar[1], Milparinka Desai[1], Purva Nanivadekar[2] [1] U.G. Student, Biomedical Engineering Department, D.J. Sanghvi College of Engineering [2] Assistant Professor, Biomedical Engineering Department, D.J. Sanghvi College of Engineering Abstract-Prostate cancer is one of the leading causes for high mortality rates in men worldwide. Hence, it becomes necessary to diagnose and treat the disease in its rudimentary stage. In this paper, we review three effective techniques used to diagnose and even, treat prostate cancer. They are mostly used or are the derivative of the conventional Transrectal Ultrasound. We have compared three methods namelyAugmentation detection using TRUS with RF time series, Prostate detection using Contrast Ultrasound and 3-D Ultrasound imaging. In this paper, we aim at finding the most efficient method for the task. Keywords: Prostate Cancer, Trans-rectal Ultrasound (TRUS), RF time series, 3D Ultrasound, Contrast Ultrasound. I.INTRODUCTION Ultrasound Imaging is a non-invasive technique which involves using ultrasound waves to determine the dimensions or location of any organ inside the body. It is used to diagnose the conditions of fetus inside the mother’s uterus, and can even be used to detect and treat kidney stones and so on. In this paper, we discuss the application of Ultrasound in diagnosis of Prostate cancer. Prostate cancer is the disease in which the cells of the prostate gland, of the male reproductive system, metastasize abnormally, leading to enlargement of the gland, which causes discomfort and pain. If medical attention in not given, prostate cancer may also prove fatal. Apart from being the most diagnosed cancer disease among men, prostate cancer has second highest mortality rate among men worldwide. It is difficult to examine the organ, due to its location.The annual incidence rate of prostate cancer in North America increased since 1980[1].This was because of the introduction of the PSA (Prostate specific antigen) blood test. The PSA and the digital rectal examination are the most widely used screening techniques. But, it was the use of ultrasound technique which accounts for the minimal invasiveness of all the three methods not enough to simply screen the disease but, there was a need to bring various therapeutic methods to treat the disease as well. With time, many new techniques were introduced. In this review paper, we discuss three of the advanced methods used in diagnosis and therapy of prostate cancer. Percutaneous ultrasound-guided prostate therapy techniques such as cryosurgery and brachytherapy, are currently under intense investigation. Although these techniques are each capable of destroying tumors while adjacent structures, the inconsistency and wide variability of their outcomes in different institutions suggest that current practice is highly operator-dependent. The conventional method for imaging is 2D TRUS(Trans-rectal ultrasound), which includes image guided cryosurgery and image guided brachysurgery. It is generally agreed that the conventional 2-D TRUS examination is an important, cost-effective and useful technique for imaging the prostate. However, it is also agreed that conventional 2-D ISSN: 2231-5381 TRUS has some serious limitations like time consumption, low-accuracy, repeatability etc. The techniques evolved are 3D Ultrasound imaging, Contrast ultrasound imaging and TRUS using RF time series. II. 3-D ULTRASOUND IMAGING SYSTEM After acquiring a series of 2-D ultrasound images, a 3-D image is reconstructed. The 3-D image is available to the physician, permitting the prostate to be viewed interactively in multiple simultaneous planes, allowing better visualization of its internal architecture. This approach allows the physician to record and view the whole prostate in successive examinations, making 3-D TRUS well suited to performing prospective or follow-up studies.[1] This procedure is described in details in various steps. A. 3-D Image acquisition The 3-D ultrasound system for imaging the prostate consists of three major components: 1) an ultrasound machine with a trans-rectal ultrasound transducer; 2) a microcomputer with a video frame-grabber; and iii) an motorized assembly to rotate the transducer under computer control [1] .The microcomputer is also used for image reconstruction, display, manipulation, and analysis of the 3-D images. Fig. 1 shows the operating principle of our approach. The TRUS transducer is mounted in the assembly and is then covered with a water-filled condom and inserted into the rectum in the same manner as for a conventional TRUS examination. When the motor is activated, it rotates the transducer around its long axis. As the transducer is rotating at constant speed, conventional B-mode images are digitized and stored in the micro-computer[1]. B. 3-D image reconstruction The image reconstruction in this method is done by designation transducer axis as the z-axis and reconstruction of P(x, y) will give the image. The newly constructed image would be mapped with cylindrical co-ordinates P(r, Ɵ, z)[1]. The value of r and Ɵ will be given as from (1) and (2) r= (1) (2) By using a pre-computed lookup table of interpolation weights, which is applied repeatedly for each successive value, the 3-D image can be rapidly reconstructed from the set of 2-D images[1]. http://www.ijettjournal.org Page 138 International Journal of Engineering Trends and Technology (IJETT) – Volume23 Number 3- May 2015 III. THREE-DIMENSIONAL ULTRASOUND SYSTEM PERFORMANCE A. Distance Measurement Fig.1. Schematic diagram showing a side-firing trans-rectal ultrasound transducer being rotated for a 3-D imaging scan [1]. C. 3-D Image Viewing Once reconstructed, the 3-D image can be viewed interactively using any 3-D visualization software. We have developed a multi-planar reformatting algorithm to view the 3D image as shown in Figs. 2 and 3. In our approach, the 3-D image is displayed as a polyhedron representing the boundaries of the reconstructed volume. Each face of the polyhedron is rendered, using a texture-mapping technique with the appropriate ultrasound image painted on that face. The polyhedron can be rotated using simple mouse controls to obtain the desired orientation of the 3-D image. Any of the faces can be moved in or out (i.e.the 3-D image can be sliced), parallel to the original, or reoriented obliquely, while the appropriate ultrasound data is texture-mapped in real-time on the new revealed face. In this way, the operator always has 3D image-based cues relating the plane being manipulated to other planes and to the rest of the anatomy. Figs. 2 and 3 show examples of the use of this approach in displaying 3-D images of the prostate [1]. In reconstruction of the 3-D image from a set of acquired 2- D images, any inconsistencies may result in image distortions resulting in erroneous distance measurements. In this method,the phantom was composed of four layers of 0.25 mm diameter surgical wires, with eight parallel wires per layer. Each layer was separated from its neighbor by 10.00 0.05 mm, and each wire was also separated from its neighbors in the layer by 10.00 mm. The wire phantom was immersed in a bath composed of a 7% glycerolsolution (1540 m/s speed of sound) and then imaged with the 3-D system[1].To obtain three orthogonal separation measurements, the locations of the centroid of each wire image were determined automatically by a computer algorithm. Fig. 3.Three-dimensional ultrasound image of a prostate with a tumor in the left base (on the left of the image). The 3-D image has been “sliced” (a) in the trans-axial plane to reveal the tumor (arrow), (b) in two planes (sagittal and trans axial), and (c) in the coronal plane[1]. B. Volume Measurement in 3-D Images of Balloons An important application of 3-D imaging of the prostate is for normalizing the PSA value with the prostate volume. To evaluate the accuracy of volume measurements using the 3-D TRUS approach, five balloons filled with different known volumes of 7% glycerol solution are imaged, and compared the measured volumes obtained from the 3-D images, to the true volumes[1]. Fig. 2.three-dimensional ultrasound images showing a prostate with a tumor. The volume is “sliced” by planes that can be angulated and positioned interactively by the user to obtain the desired view. (a) The prostate image has been “cut” in the Trans axial plane to reveal the tumor as a hypo echoic region, located just above the peri-prostatic fat region. (b) By “slicing” the image parasagittal, the prostate can be viewed with two simultaneous planes. (c) The 3-d prostate image has been “sliced” in a coronal plane to view the prostate in a plane not available using conventional 2-d TRUS[1]. ISSN: 2231-5381 IV. 2D TRUS USING RF TIME SERIES In this type of imaging, the samples were needed to be prepared for analysis.Tissue mimicking phantoms were built in the form of gelatin agar based suspensions. Microscopic glass beads with known distributions of particle sizes were added to study the effects of cell size. Gelatin and agar were http://www.ijettjournal.org Page 139 International Journal of Engineering Trends and Technology (IJETT) – Volume23 Number 3- May 2015 mixed in distilled water at room temperature and while being performed using an iU22 ultrasound scanner equipped with a constantly stirred, were heated to 90 ◦C. At this temperature, C8-4v probe[3]. The effective pulse length of two cycles point glass beads were added. Small quantities of bleach were provided an axial resolution of 0.43 mm, while a low added to avoid bacterial growth in the phantoms [2] mechanical index (MI) of 0.06 minimized SF6 microbubble disruption. The compression was set to C38 and the gain was VI. EX-VIVO HUMAN STUDIES adjustedto prevent truncation or saturation of the 8-bit grey level. All acquired B-mode videos were stored in DICOM Extracted prostate specimens were suspended in a water bath, (Digital Imaging and Communication in Medicine) format.[3] and were scanned along transverse planes that were 4 mm apart. The location of the first cross section was marked with B. Calibration two parallel needles visible in an ultrasound image as two lines. After ultrasound data acquisition, the prostate specimens To reproduce the clinical conditions, the ultrasound probe was were dissected along the scanned cross sections. positioned about 1 cm away from the UCA dispersion. For Histopathological analysis of whole mount slides was each concentration, three measurements were performed, from acquired and used as the gold standard. The contours of three different SonoVue vials. The mean acoustic intensity tumors were directly marked on the slides by a senior was evaluated in a fixed region of interest (ROI) of the pathologist. The process of histopathological characterization recorded B-mode images [3]. of the prostate tissue is a routine clinical task [2]. C. Diffusion Modelling VII. CLASSIFICATION This two-stage method of feature selection (aimed at optimizing both the dimension of the feature vector and the choice of features) was not guaranteed to provide the highest possible accuracy. An exhaustive search over all 22 features combined could have resulted in a better performing subset. However, it required examining 22 n=0 C22 n = 222 subsets that was computationally infeasible[2]. Physical modelling of the intravascular UCA transport is required to analysediffusion. The analysis is based on the local density random walk (LDRW)model. This model can provide a physical interpretation of the diffusion process, and it accurately fits UCA indicator dilution curves (IDCs)[3].IDCs measure the UCA concentration in a fixed sample volume as function of time and can thus be obtained from TDC. After a general introduction to the LDRW model, the local aspects of the diffusion process by this model are discussed [3]. B.SVM Classifier D.Parameter Estimation SVM maps the input data to a higher dimension space where a hyperplane can separate the data in different classes. The process of training an SVM classifier is equivalent to finding this optimal hyperplane in a way that minimizes the error on the training dataset and maximizes the perpendicular distance between the decision boundary and the closest data points in classes.[2] Local diffusion can be estimated from measured TDCs using the modified LDRW IDC formalization and the relation between UCA concentration and gray level. The accuracy of the parameter estimation is determined by the temporal characteristics of IDC noise, i.e., all signals that the model function (1) cannot explain (3). The accuracy of the parameter estimation is improved bylow-pass filtering the TDCs both in space and time. The spatial filter design is based on the size of the smallestmicro-vascular networks for which local diffusion must be estimated.As angiogenesis is required for cancer to grow beyond1 mm, a reliable analysis of image regions with a radiusas small as 0.62 mm is necessary.[3] A. Feature Selection VIII. CONTRAST ULTRASOUND IMAGING A. Data Acquisition [3] The Data Acquisition for Contrast Ultrasound Diffusion Imaging (CUDI) was performed after approval from the patients A 2.4 mL Sono Vue UCA bolus was injected intravenously in the patient’s arm. TRUS imaging was ISSN: 2231-5381 This was a brief description about the various methods that we intend to compare. In the next section, we list various parameters that differentiate each method from one another. These parameters include the various advantages and disadvantages of the methods. http://www.ijettjournal.org Page 140 International Journal of Engineering Trends and Technology (IJETT) – Volume23 Number 3- May 2015 IX.COMPARISON Parameters CUDI (Contrast Ultrasound) Phantom used for study Not used Apparatus, equipment, software 1. 2. Parameter which is detected Time required Results 2.4 ml SonoVue UCA bolus. iU22 ultrasound scanner equipped with C8-4v probe. 3. Matlab software. 4. Windows based workstation running on Intel Core2 Duo processor. Diffusion-related parameter (k) 5 minutes Sensitivity: 81.2% Specificity: 84.6% Advantages It overcomes the problem of the selection of proper TRUS plane. Disadvantages 1. 2. 3. UCA has to be injected. Validation is restricted to only peripheral zones. Validation restricted to patients whose histology did not show significant variation across subsequent slices. TRUS using SVM and RF time series Microscopic glass beads of various sizes with known distributions are added to gelatin based agar suspension. 1. Sonix RP ultrasound machine. 2. Sun microsystems 3D ultrasound imaging system Four layers of 0.25mm diameter surgical wires, with 8 parallel wires per layer. Various parameters are used. Various parameters are used. 7 seconds Acquisition rate: 22 fps Accuracy: 80.5% Sensitivity: 79.8% Specificity: 81.1% Color maps with accurately highlighted areas of tissue with high risk of cancer are created on the ultrasound image. 8 seconds Error: less than 3% Volume measurement: accuracy:2.6% Precision:2.5% 1. Minimally invasive. 2. Overcomes all drawbacks of TRUS. 3. Can be interfaced with any conventional ultrasound machine. 1) Surgeon should keep his/her hand steady for 7 seconds. 2) Detection is done in only peripheral zones but for 80% of cases cancer occur in this region. 3) In vivo studies are not conducted. 4) Selection of proper plane is difficult Not mentioned. 1. ALT Ultramark 9 ultrasound imaging system. REFERENCES CONCLUSION [1]A. Fenster, S. Tong, H. N. Cardinal, C. Blake, and D. B. Downey, Ultrasound is a novel tool for detecting prostate cancer. The three methods discussed above are reliable and under early stages of research. Principle of CUDI is an increase in angiogenesis whereas TRUS based on size of cancerous cells. 3D ultrasound imaging is a modification of TRUS. CUDI is an alternative to TRUS as it overcomes the main drawback. Moreover specificity and sensitivity is better but requirement for injection of contrast agent is its demerit and time required is also more. The technique with most benefits is 3D ultrasound since, it gives 3D image which makes it potential tool for diagnosis, therapy and follow-up of prostate disease. It can be interfaced with any conventional ultrasound machine. Cost is high and that has to be considered. ISSN: 2231-5381 “Three-Dimensional Ultrasound Imaging System for Prostate Cancer Diagnosis and Treatment”,IEEE transactions on instrumentation and measurement, vol. 47, no. 6, December 1998. [2]Mehdi Moradi, Student Member, IEEE, Purang Abolmaesumi, Member, IEEE, D. Robert Siemens, Eric E. Sauerbrei,Alexander H. Boag, and Parvin Mousavi, Senior Member, IEEE, “ Augmenting Detection of Prostate Cancerin Transrectal Ultrasound Images Using SVMand RF Time Series”,IEEE transactions on biomedical engineering, vol. 56, no. 9, September 2009. [3] Maarten P. J. Kuenen, Massimo Mischi, and Hessel Wijkstra,” Contrast-Ultrasound Diffusion Imaging for Localization of Prostate Cancer”, IEEE transactions on medical imaging, vol. 30, no. 8, August 2011. http://www.ijettjournal.org Page 141


![Jiye Jin-2014[1].3.17](http://s2.studylib.net/store/data/005485437_1-38483f116d2f44a767f9ba4fa894c894-300x300.png)