Control of bacterial growth:-
advertisement
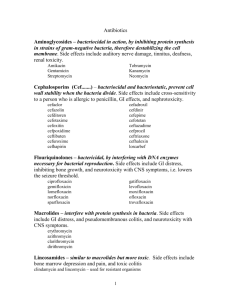
Dr. Lamees A. Razzak Control of bacterial growth:- Control of growth, means to prevent growth of microorganisms. This control is effected in two basic ways: (1) by killing microorganisms (2) by inhibiting the growth of microorganisms. Bactericidal:- chemical agent to killing bacteria pathogenic and nonpathogenic but not necessary spore when applied to either living tissue or intimate surface. Bacteriostatic:- agent to inhibiting the growth of bacterial cells. Disinfectants:- are substances that are applied to non-living objects to destroy microorganisms that are living on the objects. Disinfection:-The process or act of destroying pathogenic microorganisms. Reducing the number of viable microorganisms present in a sample. does not necessarily kill all microorganisms, especially resistant bacterial spores Septic:- presence of pathogenic microbes in living tissue. Aseptic:- absence of pathogenic microbes. Antiseptic:- chemical agent that destroy or inhibit the growth of microorganism in living tissue. Sterilization:- a physical or chemical process that completely destroys or removes all microbial life, including spore. Methods used for sterilization or disinfection:Physical agents:A- Application of heat:Autoclaving (steam under pressure or pressure cooker, moist heat): Autoclaving is the most effective and most efficient means of sterilization. All autoclaves operate on a time/temperature relationship. These two variables are extremely important. Higher temperatures ensure more rapid killing. The usual standard temperature/pressure employed is 121ºC/15 psi for 15 minutes. Autoclaving is ideal for sterilizing biohazardous waste, surgical dressings, glassware, many types of microbiologic media, liquids, and many other things. However, certain items, such as plastics and certain medical instruments (e.g. fiberoptic endoscopes), cannot withstand autoclaving and should be sterilized with chemical or gas sterilants. kills all forms of life including bacterial endospores. *Moist heat not under pressure:1- Boiling: Most of vegetative form of bacteria and fungi are killed at 50-70ºC for short time. 100ºC for 30 minutes (more time at high altitude). Kills everything except some endospores. It also inactivates viruses. At this degree is sterilize needle and instrument and boiling of water. 1 2- Pasteurization:is the use of mild heat to reduce the number of microorganisms in a product or food. Pasteurization does not sterilize, but does kill disease producing bacteria. In the case of pasteurization of milk, the time and temperature depend on killing potential pathogens that are transmitted in milk, i.e., staphylococci, streptococci, Brucella abortus and Mycobacterium tuberculosis. Pasteurization occurs via either of two procedure:a- holding method:- the liquid is heated to 62ºC for 30 minutes. b- flesh method:- the liquid is heated to 71ºC for 15 to 20 second. *Dry heat:1- Hot air oven:Basically the cooking oven. The rules of relating time and temperature apply, but dry heat is not as effective as moist heat (i.e., higher temperatures are needed for longer periods of time). For example 160 ºC /2hours or 170 ºC /1hour is necessary for sterilization. The dry heat oven is used for glassware, metal, and objects that won't melt. 2- Flaming:Is the direct exposure of instruments or inoculating loops to open flames for brief period. 3- Incineration: Rapidly destroying any material and contaminating microorganisms that may be present. B- Radiation: Usually destroys or distorts nucleic acids. Ultraviolet light is commonly used to sterilize the surfaces of objects, although x-rays, gamma radiation and electron beam radiation are also used. a-Ultraviolet:possess bactericidal or bacteriostatic properties. The maximum killing effect is 260nm. Isolation room or laboratory can be exposed to UV light to prevent the spread of disease producing microorganism. UV light is damaging to human tissue and direct exposure must be avoided UV light causes following change in cell:1- damage of DNA 2- denaturation of protein 3- inhibition of DNA replication 4- formation of H2O2 and organic peroxidase in culture media 2 b- X-ray and other ionizing radiation:ionizing radiation have great capacity to induce lethal change in DNA of cell by break one or both DNA strands and interfere with DNA replication. Ionizing radiation is used to sterilize product like surgical instrument and disposable plastic items as well as heat processed canned meat. C- Filtration:involves the physical removal (exclusion) of all cells in a liquid or gas. It is especially important for sterilization of solutions which would be denatured by heat (e.g. antibiotics, injectable drugs, amino acids, vitamins, etc.). Essentially, solutions or gases are passed through a filter of sufficient pore diameter (generally 0.22 micron) to remove the smallest known bacterial cells. * Chemical agents:Chemical agents act primarily by one of three mechanism:1- Disruption of the lipid-containing cell membrane 2- Modification of proteins 3- Modification of DNA The commonly used chemical agents are:1. Phenol:Is antibacterial agent at high concentration employed (2% aqueous solution). denature proteins and disrupt cell membranes excellent for surfaces, but can cause skin irritation 2. Alcohols and isopropyl:Is bactericidal and fungicidal, but not sporicidal, concentration generally employed (70% aqueous solution), denature proteins and dissolve membrane lipids. 3. Halogens Iodine most common used chiefly in skin. Chlorine combine with water to form hydrochloric acid which in bactericidal 4. Heavy metals like Hg, Ag, As, Zn, Cu used to be common germicides, most heavy metals are bacteriostatic, not bactericidal, that is used in very low concentration because it is dangerous to the tissue. 5. Detergents:They are bactericidal and bacteriostatic detergent, disrupt membranes and may denature proteins, kill most cells, but not endospores or M. tuberculosis 6. Alkylating agents like:a- formaldehyde:- is used as disinfectant in (37% aqueous solution) b- ethylene oxide:- useful for disinfection of surgical instruments and materials which must be placed in special vacuum chambers for this purpose. 3 *Antibiotics:are natural substance of low molecular-weight (non-protein) molecules produced as secondary metabolites, mainly by microorganisms (especially Actinomycetes, Streptomyces, a few molds (Penicillium and Cephalosporium that are inhabitants of soils), that react with and inhibit the growth of other microorganisms. They are not laboratory chemicals as are the antiseptics and disinfectants. In some cases antibiotics have been synthesized by chemists in which case they are known as chemotherapeutic agents. *Mode of action of antibiotic:1- Cell Wall Synthesis Inhibitors: Bacteria contain murin or peptidoglycan that is highly essential in maintaining the cell wall structure. Cell wall synthesis inhibitors such as beta-lactams, cephalosporins and glycopeptides block the ability of microorganisms to synthesize their cell wall by inhibiting the synthesis of peptidoglycan. 2- Interfering with Protein Synthesis: These classes of antibiotics inhibit the protein synthesis machinery in the cell. Some examples include tetracycline, chloramphenicol, aminoglycosides and macrolides. 3- Cell Membrane Inhibitors: Antibiotics such as polymyxins disrupt the integrity and structure of cell membranes, thereby killing them. These set of antibiotics are mostly effective on gram negative bacteria because these are the bacteria that contain a definite cell membrane. 4- Effect on Nucleic Acids: DNA and RNA are extremely essential nucleic acids present in every living cell. Antibiotics such as quinolones and rifamycins bind to the proteins that are required for the processing of DNA and RNA, thus blocking their synthesis and thereby affecting the growth of the cells. 5- Competitive Inhibitors: Also referred to as anti-metabolites or growth factor analogs, these are antibiotics that competitively inhibit the important metabolic pathways occurring inside the bacterial cell. Important ones in this class are sulfonamides such as Trimethoprim 4 *Antibiotic resistance:The basis of microbial resistance to antibiotics are two: 1- Non-genetic mechanism:1- Bacteria can be walled off within an abscess cavity that the drug cannot penetrate effectively. 2- Organism that would be killed by penicillin can lose their cell walls and be insensitive to cell wall active drug. 3- Antibiotics are ineffective against spore because spore coat impermeable to antibiotics. 2- Genetic mechanism 1- May result from chromosome or extrachromosomal resistance 2- May involve chromosomal mutation that alter the structure of the receptor of drug or the permeability of drug 3- They result from R-plasmid that code for enzyme (beta-lactemase ) that degrade the drug The medical problem of bacterial drug resistance:If a bacterial pathogen is able to develop or acquire resistance to an antibiotic, then that substance becomes useless in the treatment of infectious disease caused by that pathogen. So, we must find new (different) antibiotics to fill the place of the old ones in treatment regimes. Natural penicillin have become useless against staphylococci and must be replaced by other antibiotics; tetracycline. 5